Abstract
Purpose of Review
There is emerging evidence that the post-acute and chronic phases of COVID-19 infection are associated with various significant cardiovascular sequelae.
Recent Findings
Long COVID has been shown to be associated with multiple cardiovascular sequelae including direct myocardial injury, arrhythmias, and cardiomyopathies. Hypotheses on the mechanism of myocardial injury include direct viral infiltration and autoimmune dysregulation. Long COVID is associated with persistent cardiac ischemia in patients with no previous history of coronary disease, atrial and ventricular arrhythmias, and the development of new-onset heart failure in previously healthy patients. Onset of long COVID may be related to severity of the initial SARS-CoV2 infection. Cardiac MRI is a valuable tool in assessing myocarditis and the development of cardiomyopathies in the setting of long COVID.
Summary
Both patients with and without pre-existing cardiovascular disease are at risk of developing myocardial injury in the setting of long COVID. Future studies will elucidate both cardiovascular mortality and cardiac rehabilitation in the post-acute and chronic phases of COVID-19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
SARS-CoV2, the virus responsible for the Coronavirus-2019 (COVID-19) pandemic, is most notably known for activating both the innate and adaptive immune responses in the host causing uncontrolled inflammation which may lead to local and systemic tissue damage in the acute setting [1]. However, as we continue to learn from the effects of the COVID-19 pandemic, an increasing number of reports have been published regarding post-acute illness following initial infection with SARS-CoV2 [2, 3].
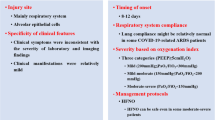
Persistent illness or symptoms following initial SARS-CoV2 infection have been termed “Post-Acute COVID Syndrome” or “Long COVID.” The National Institute for Health and Care Excellence in the UK has attempted to further differentiate these illnesses by assigning the name long COVID to persistent symptoms present 4 weeks after initial SARS-CoV2 infection and post-COVID-19 syndrome (PCS) to persistent symptoms present 12 weeks after initial SARS-CoV2 infection [4]. Nonetheless, for practical purposes, these terms have remained interchangeable in discussions regarding symptoms following COVID-19 infection that cannot be explained by an alternative diagnosis. Cardiovascular sequelae of long COVID have been of particular interest because of its associated morbidity and mortality. A prospective cohort study of over 150,000 individuals who had survived 30 days following their index SARS-CoV2 infection were found to be at increased risk of developing cardiovascular complications including ischemic heart disease, dysrhythmias, myocarditis, pericarditis, heart failure, and thromboembolic disease compared to matched, historical controls [5••].
Given the sizeable public health impact caused by cardiac complications of long COVID-19 infection, we performed a narrative literature review to examine the currently available information. We searched the PubMed, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), and Cumulative Index to Nursing and Allied Health Literature (CINAHL) databases through July 30, 2022, with no restrictions on language. Key words of SARS-CoV2, COVID-19, Long COVID, post COVID syndrome myocardial injury, and cardiac injury were used in these searches. Case series, large prospective studies, meta-analyses, and systematic reviews were included, although notably, there are virtually no randomized clinical trials on the subject. Relevant references in the articles that were identified were then manually searched. Given the nature of this review and no direct patient contact, Institutional Review Board approval was not necessary.
Incidence and Risk Factors of “Long COVID”
The reported incidence of long COVID has been variable, ranging from 21 to 62% of patients following initial SARS-CoV2 infection, with as many as 87.4% of patients reporting persistence of at least 1 symptom [6, 7]. A retrospective cohort study of nearly 275,000 COVID-19 survivors found that 57% suffered from long COVID with the most common symptoms being abnormal breathing, fatigue, chest pain, headache, and anxiety and depression [8]. Another prospective cohort study found that even after controlling for pre-existing symptoms, approximately 1 in 8 patients will likely be affected by post-acute sequelae following COVID-19 infection [9].
Onset of long COVID may be related to severity of the initial SARS-CoV2 infection. A prospective cohort study found that long COVID is more commonly identified in patients who required hospitalization for their index SARS-CoV2 infection and in women [10]. However, patients with asymptomatic and mild SARS-CoV2 infection are also susceptible not only to developing long COVID but also to developing multi-organ impairment as a result [11].
Previously diagnosed cardiovascular disease (CVD) may also be a risk factor for developing further complications from long COVID. A retrospective cohort study found that patients with pre-existing (CVD) or risk factors for cardiovascular disease (CVD) who had chronic myocardial injury at the time of index SARS-CoV2 infection had higher mortality at 6 months compared to the control group [12•]. Additionally, a prospective cohort study of patients hospitalized due to initial SARS-CoV2 infection also found that older patients were at greater risk of developing cardiovascular sequelae at 12 months post-discharge [13].
SARS-CoV2 vaccination has been shown to be associated with a decreased risk of developing long COVID based on a large, observational cohort study involving over 28,000 participants in the UK [14•]. Specifically, a two-dose vaccination regimen has been shown to decrease symptoms from COVID-19 infection in the acute setting and reduce the incidence of long COVID in patients who develop breakthrough infections post-vaccination by approximately 50% [15•]. The protection of vaccines seems to extend for long-term for mortality, severity of disease, and development of long COVID [16].
Pathogenesis of “Long COVID”
The current understanding of viral-mediated injury in COVID-19 infection is that the SARS-CoV2 virus binds to and causes downregulation of ACE2 receptors on target cells, resulting in increased transformation of the pro-inflammatory angiotensin II (ANGII) hormone into the anti-inflammatory ANG1-7 hormone [17,18,19,20]. The pathogenesis of long COVID is less certain at this point. Immunofluorescence and PCR analyses of intestinal biopsies from individuals who had experienced asymptomatic SARS-CoV2 infection revealed persistence of SARS-CoV2 nucleic acids and immunoreactivity in 50% of samples 4 months after the initial infection [21]. Additionally, post-mortem biopsy in a patient 3 weeks after initial SARS-CoV2 infection also detected viral RNA in cardiac tissue, suggesting that direct viral infiltration may persist and could play a role in the propagation of long-term cardiovascular sequelae [22]. Based on these findings, long COVID may be a result of persistent viral penetration of SARS-CoV2 that extends past the initial acute phase and asymptomatic COVID-19 infection, by itself, may not be a protective factor against long COVID.
COVID-19 infection has also been associated with increased autoantibody formation against immunomodulatory proteins compared to uninfected individuals [23]. Previous studies have found that T cells formed during the immune response to other human coronavirus infections have been shown to cross-react to myelin in patients with multiple sclerosis [24]. While it is unclear if SARS-CoV2-specific T cells react against self-antigens as well, this mechanism of “molecular mimicry” also seen in autoimmune disorders could potentially be another possible route through which long COVID develops [25]. Other possible hypothesis is that persistence of the spike protein itself, separate from the coronavirus, may contribute to the development of long COVID. Studies have shown that even in isolation, the SARS-CoV2 spike protein can cause inflammation and cellular injury [26, 27]. Another possible mechanism is uncontrolled inflammation as patients with PACS have been found to have increased levels of cytokine biomarkers such as tumor necrosis factor-α and interferon-γ during early recovery [28]. The exact mechanism of development of long COVID remains an area of active investigation.
Myocardial Injury and Ischemic Heart Disease
Concomitant diagnosis of COVID-19 in patients presenting with ST-elevation myocardial infarction (STEMI) is associated with increased mortality in the acute setting when compared to a cohort of patients presenting with STEMI who were negative for COVID-19 [29]. Nonetheless, whether the worse outcomes in concomitant COVID infection and STEMI extends long-term is less clear as patients with COVID-19 were significantly less likely to undergo invasive diagnosis or therapeutic coronary procedures [19], particularly for in-hospital STEMI presentations. In a large prospective cohort study of patients with post-acute COVID-19 syndrome (PCS), these patients had a 4.8% rate of hospital readmission over a period of 8 months due to a major cardiovascular event, a composite outcome of myocardial infarction, heart failure, stroke, or arrhythmia, which was three times higher than in the matched, control group [30]. This pattern of increased risk for cardiovascular events and complications following acute myocardial infarction (AMI) has also been described in the setting of other viral infections as influenza. A review of nearly 2.5 million patients with AMI found that patients with concomitant influenza infection not only had greater in-hospital mortality in the acute setting but also increased complications in the post-acute setting leading to greater rate of 30-day hospital readmission [31]. Comparably, a single-center retrospective cohort study following patients with concomitant diagnosis of COVID-19 with STEMI for one year after index admission found long-term mortality rates in these patients that survived to discharge to be comparable to a COVID-negative STEMI cohort [32]. The discrepancy between these reports could be related to differences in the study populations, severity of COVID-19 infection at the time of presentation, and improved treatment modalities for COVID-19 infection.
There is further evidence to suggest persistent myocardial injury after initial COVID-19 infection. A prospective cohort study of 148 patients with COVID-19 infection requiring hospital admission found evidence of infarction or ischemic heart disease on cardiac magnetic resonance (CMR) imaging in 22% of patients two months following discharge [33•]. Ischemic injury pattern, defined as having either sub-endocardial or transmural late gadolinium enhancement (LGE) on CMR or inducible ischemia on adenosine stress test, was found in 66% of patients with no prior history of coronary disease. Another study comparing patients who developed myocardial injury, defined by high-sensitivity troponin T (hsTnT) elevation exceeding the 99th percentile, during hospitalization for COVID-19 infection versus those without myocardial injury found that patients with myocardial injury had higher frequency of impaired diastolic function, larger left atrial size, and higher values of pulmonary artery pressure at three-month follow-up as compared to the group that did not develop myocardial injury during hospitalization for COVID-19 infection [34]. Another prospective cohort study evaluating 159 patients found that at 4–9 weeks post-hospitalization for COVID-19 infection, patients recovering from COVID-19 were at greater risk of developing myocardial scarring and persistent cardio-renal dysfunction as compared to matched control [35].
Moreover, there is some evidence to suggest that mild COVID-19 infection may result in persistent myocardial injury as well. A study evaluating 137 previously health collegiate athletes 2 weeks after largely, mildly symptomatic COVID-19 infection found that 2.9% of participants had cardiac troponin I (cTnI) elevation exceeding the 99th percentile despite exhibiting no specific cardiac complaints [36].
Arrhythmias
COVID-19 infection is an inflammatory state and have been associated with development of cardiac arrhythmias. In a study using the national healthcare databases of the US Department of Veterans Affairs involving 73,435 non-hospitalized veterans, those infected with COVID-19 were eight times more likely to develop arrhythmias over a median follow-up of four months [37•]. A retrospective cohort study of over 250,000 individuals found that when compared to a cumulative group of other lower respiratory pathogens, infection with SARS-CoV2 was associated with a higher rate of arrhythmia development at four months regardless of pre-existing conditions and independent if the index COVID-19 admission required hospitalization [38]. Another retrospective longitudinal observational follow-up study in Spain found that at 6-month follow-up, 3.1% of patients with persistent symptoms suggestive of PCS had an identifiable arrhythmia or symptomatic palpitations [39•]. In another smaller, prospective observational study, newly detected atrial fibrillation was reported in 1.0% of patients following initial COVID-19 infection that required hospital admission [40]; the lower incidence rate in this study may be due to its study design, as the presence of arrhythmias was screened with a single electrocardiogram 1–4 weeks after hospital discharge.
A prospective, observational cohort study of over 4000 individuals found that of patients with PCS, 6.1% reported symptomatic palpitations or persistent tachycardia 28 days following acute illness [41]. A longitudinal study of clinical sequelae 3 months after COVID-19 infection found that 11.1% of patients reported a resting heart rate more than 20 beats per minute higher than prior to COVID-19 infection and 4.8% of patients reported occasional palpitations [42]. Another retrospective observational study found that between 3 and 6 months after COVID-19 infection, up to 11% of patients still complain of intermittent episodes of palpitations [43].
The incidence of ventricular arrhythmia in patients with COVID-19 infection is less well-documented. A combined multi-center prospective cohort study and cross-sectional case control study involving 408 patients found that at 3-month follow-up, arrhythmias were found in 27% of the patients with the majority comprising of premature ventricular contractions and non-sustained ventricular tachycardia (18% and 5%, respectively) [44]. In a meta-analysis involving 11,439 COVID patients, the overall incidence of arrhythmias was 10.1%, with atrial arrhythmias presenting 10.4% of patients in the reported studies, ventricular arrhythmias 2.1% (sustained ventricular tachycardia/ventricular fibrillation in 1.1%), and atrioventricular block in 1.2% of cases [45]. It is noteworthy that the characterization of cardiac arrhythmias is poor is most studies, and the severity and clinical significance are not well-documented.
Given the previously studied association between myocarditis and the post-acute phase of COVID-19 infection, a single-center prospective study of myocarditis patients found that polymorphic ventricular arrhythmias (VA) are more common during the active inflammatory phase, whereas monomorphic VA are associated with healed myocarditis [46].
Autonomic dysfunction has also been reported post-acute SARS-CoV2 infection. In 6 previously healthy patients, 6 weeks following acute SARS-CoV2 infection that did not require hospitalization found that 66% had findings consistent with postural orthostatic tachycardia syndrome (POTS) on evaluation, suggesting that PCS may cause some autonomic dysfunction [47]. However, a larger prospective observational study with 180 patients presenting between 4 weeks and 9 months of initial COVID-19 infection failed to find a single case of POTS on similar autonomic evaluation [48].
Heart Failure and Cardiomyopathies
Patients with PCS have been found to have excess disease burden of heart failure nearly 4 times that of matched controls [37•]. While up to 55% of patients with acute SARS-CoV2 infection have an abnormal echocardiogram, there is evidence to suggest that some of these abnormalities persist. A Spanish cross-sectional analysis found new-onset heart failure in 2.0% of patients at one year following acute COVID-19 infection [49, 50]. Biomarkers as brain natriuretic peptide levels have also been found to remain elevated in 7.4% of patients at 6 months post-discharge following hospital admission for COVID-19 infection [51]. A short course of corticosteroids remains the standard treatment for patients hospitalized with COVID-19 who require supplemental oxygen, but a recent retrospective review found that a brief course of less than 14 days was associated with an increased development of new heart failure up to 90 days following treatment [52]. The authors did not provide more characterization of these incident heart failure cases.
While some acute abnormalities in ventricular size or function among hospitalized patients with COVID-19 pneumonia resolve post-acute infection, a multi-center prospective, echocardiographic-based, observational cohort study in the UK showed persistent evidence of adverse ventricular remodeling in nearly one-third (29%) of cases 3 months post-infection [53]. The most commonly identified changes in this study were significantly lower RV basal dimensions and a significant increase in RV fractional area change at 3 months when compared with baseline measurements. Echocardiographic parameters of diastolic dysfunction have also has been found in 55–60% and 55% of patients after 2 or 3 months post COVID-19 infection [54]. At 3 months after hospital discharge with COVID-19, right ventricular function has been found to be continued to be mildly impaired, and diastolic dysfunction was reported twice as commonly in these patients as compared with controls [44]. Reduced left ventricular global longitudinal strain (LVGLS) has also been observed in up to 70% of patients without cardiac symptoms as far as 5 months post COVID-19 infection [55]. Subclinical right ventricular dysfunction has also been seen to occur in patients with no previously identified risk factors for cardiovascular disease 30 days after hospital discharge following treatment for moderate to severe COVID-19 pneumonia [56]. An observational study in patients 3 months after hospital discharge for COVID-19 pneumonia found that depressed endocardial RV free wall longitudinal stress to −19.3% (called hidden right ventricular (RV) systolic dysfunction by the authors) was associated with increased pulmonary vascular resistance ≥ 1.5 Wood units [57].
In patients with persistent symptoms 5 months after initial SARS-CoV2 infection, 39% had echocardiographic findings of RV dilatation, 16% had findings of left ventricular (LV) diastolic dysfunction, and 10% had findings of LV systolic dysfunction [58•]. Another prospective cohort study in low-risk patients with PCS 4 months post-infection found that 9% of patients had some systolic dysfunction on CMR with the incidence increasing as the severity of PCS increased [59•]. Acute infection with SARS-CoV2 has also been linked to the development of Takotsubo cardiomyopathy [60]. This predisposition in developing Takotsubo cardiomyopathy could perhaps be a factor in the persistence in some of these cardiac abnormalities as a recent case–control study showed long-term symptomatic and functional impairment despite normalized ejection fraction in patients found to have Takotsubo cardiomyopathy [61].
Myocarditis and Pericarditis
Acute SARS-CoV2 infection has been associated with both myocardial and pericardial inflammation [62]. However, there is also evidence to suggest that this myocardial inflammation could be persistent. In a prospective, observational, cohort study utilizing CMR (n = 100), at 10 weeks following initial SARS-CoV2 infection cardiac involvement was seeing in 78 patients (78%) and ongoing myocardial inflammation in 60 patients (60%), independent of pre-existing conditions, severity and overall course of the acute illness, and time from the original diagnosis [63]. Chronic inflammation in the setting of long COVID may also cause adverse cardiac remodeling as well. Further utilization of CMR continued to find not only evidence of persistent cardiac inflammation but also cardiac fibrosis 2 months after initial infection with SARS-CoV2 [64].
CMR may be the best available modality to assess and quantify myocardial inflammation in the setting of long COVID. Comprehensive evaluation using CMR approximately 2 months after initial COVID-19 infection found that 19% of patients had non-ischemic LGE with elevated global T2-mapping values (57 to 62 ms), fulfilling the Lake Louise criteria for suspected myocarditis [65]. Myocarditis in the setting of long COVID is also associated with both RV and LV systolic dysfunction. A 3-month follow-up study after initial infection with SARS-CoV2 found that 30% of patients had LGE and further analysis in these patients showed decreased LV peak global circumferential strain (GCS), RV peak GCS, and RV peak global longitudinal strain (GLS) as compared to non-LGE patients (p < 0.05) [66].
Myocarditis seems to develop in the post-acute setting of SARS-CoV2 infection regardless of patient condition and previous CVD risk factors. A prospective cohort study in otherwise low-risk patients in the general population with PCS 4 months post-infection found that 19% of patients had MRI evidence of myocarditis [59•]. Risk of developing myocarditis remained even in highly trained athletes. A retrospective cohort study involving 26 elite athletes that had mild or asymptomatic COVID-19 infection found that 19% had CMR abnormalities including isolated myocardial edema and late gadolinium enhancement (LGE) suggestive of myocardial inflammation [67]. Even when applying the Lake Louise criteria for myocarditis, CMR evaluation in competitive college athletes revealed that 15% had CMR findings consistent with myocarditis over 3 weeks after mildly symptomatic COVID-19 infection [68]. However, a third study involving collegiate athletes found that only 2.3% of participants had either clinical or subclinical myocarditis by CMR assessment at an average of approximately 4 weeks after initial COVID-19 infection [69].
Evidence strictly pertaining to pericarditis in the post-acute phase of COVID-19 infection is scarce. CMR evaluation of 59 athletes 3 weeks following mild or asymptomatic COVID-19 infection revealed pericarditis in approximately 1.7% of participants [70]. Another similar study in professional athletes found the prevalence of pericarditis to be at 0.3% 2 weeks following acute COVID-19 infection [71]. In a study of healthcare workers with previously confirmed SARS-CoV2 infection, CMR evaluation 10 weeks after initial infection showed pericarditis in 3%, myopericarditis in 11%, and isolated myocarditis in 26% of study participants [72].
Thromboembolic Disease
Acute infection with SARS-CoV2 has been found to be associated with an increase in both major arterial and venous thromboembolisms [73]. Risk for further thromboembolic events may remain in the post-acute setting as a prospective cohort study of 384 patients following hospital discharge for COVID-19 pneumonia found that 30.1% of these patients had continued elevation in d-dimer after a mean of 54 days post-discharge [74]. In a prospective cohort study evaluating patients with persistent symptoms following initial infection with SARS-CoV2, 1.1% had experienced a thromboembolic event at 1-year follow-up [13]. Another retrospective, observational study of patients discharged following hospitalization for COVID-19 pneumonia found that these patients were at increased rate of readmission for thrombotic events both within 30 days post-discharge and even after 30 days post-discharge [75]. The incidence of thromboembolic events in long COVID has been found to be 2.4% for deep vein thrombosis (DVT) and 1.7% for pulmonary emboli (PE) in a cross-sectional analysis [50].
Current Evaluation and Management
Strategies for evaluating and managing long COVID and its cardiovascular sequelae are evolving in real-time. The American College of Cardiology (ACC) recently released an expert consensus decision pathway on the topic of cardiovascular sequelae of COVID-19 [76••]. Baseline recommendations include a multi-disciplinary approach in initial evaluation and early cardiologist involvement in the setting of abnormal cardiac test results and persistent cardiopulmonary symptoms.
For patients with chest pain and concern for ischemic heart disease, an ischemic evaluation should be performed per previously established guidelines [77•]. Low-risk patients may be assessed with coronary artery calcium testing or exercise testing whereas computed tomography (CT) angiography or stress imaging may be performed in higher risk patients. Invasive coronary angiography should be reserved for cases with strong suspicion for obstructive coronary artery disease or vasospasm.
For patients with concerns for new or worsening arrhythmias, ambulatory rhythm monitoring should be considered. Similar to other settings, the duration of monitoring can be determined based on the reported frequency of patient-reported symptoms [76••].
Future Studies
There are many gaps in our current knowledge of the cardiac complications involving long COVID. Ongoing and future studies will be key to help best guide management of these complications. One such study in progress is COVID-HEART. COVID-HEART is a multi-center, prospective, observational, longitudinal cohort study of patients with confirmed COVID-19 and elevated troponin based in the UK whose goals include evaluating differences in myocardial recovery at 6 months and further investigating the impact of myocardial recovery at 6 months on patient-reported quality of life and functional capacity [78]. The proposed CV-COVID registry will be a multi-center, observational, retrospective study conducted in both Spain and Italy and will look to compare cardiovascular mortality at 1 year in patients who were previously diagnosed with COVID-19 infection with those who did not experience COVID-19 infection [79]. The COVID-Rehab study will look to investigate the efficacy of an eight-week cardiopulmonary rehabilitation program on cardiorespiratory fitness (V˙O2max) in individuals experiencing long COVID-19 [80].
Conclusion
As time continues to pass from the onset of the COVID-19 pandemic, clinical and epidemiological evidence of cardiac sequelae in the post-acute and chronic phases of SARS-CoV2 infection continues to emerge. Understanding the risk factors, mechanism of onset, and further complications of myocardial involvement in long COVID will be a pivotal role for the cardiologist to play in the coming years. Increased utilization of non-invasive imaging modalities, such as CMR, will be crucial in identifying further long-term complications of post-acute SARS-CoV2 infection. Further studies will provide additional insight not only into longer term cardiac manifestations of COVID-19 infection but also on cardiovascular morbidity and mortality of COVID-19 vaccination and current treatments.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Anka AU, Tahir MI, Abubakar SD, et al. Coronavirus disease 2019 (COVID-19): an overview of the immunopathology, serological diagnosis and management. Scand J Immunol. 2021;93(4):e12998. https://doi.org/10.1111/sji.12998.
Carfì A, Bernabei R, Landi F, Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603–5. https://doi.org/10.1001/jama.2020.12603.
Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220–32. https://doi.org/10.1016/S0140-6736(20)32656-8.
COVID-19 rapid guideline: managing the long-term effects of COVID-19. London: National Institute for Health and Care Excellence (NICE); 2020 Dec 18. (NICE Guideline, No. 188.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK567261/
•• Xie Y, Xu E, Bowe B, Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat Med. 2022;28(3):583–90. https://doi.org/10.1038/s41591-022-01689-3. One of the largest cohort studies to date showing that patients who had a COVID-19 infection continued to be at increased risk of cardiac complications 30 days after initial infection.
Zhan Y, Zhu Y, Wang S, et al. SARS-CoV-2 immunity and functional recovery of COVID-19 patients 1-year after infection. Signal Transduct Target Ther. 2021;6(1):368. https://doi.org/10.1038/s41392-021-00777-z.
Nune A, Durkowski V, Titman A, et al. Incidence and risk factors of long COVID in the UK: a single-centre observational study. J R Coll Physicians Edinb. 2021;51(4):338–43. https://doi.org/10.4997/JRCPE.2021.405.
Taquet M, Dercon Q, Luciano S, Geddes JR, Husain M, Harrison PJ. Incidence, co-occurrence, and evolution of long-COVID features: a 6-month retrospective cohort study of 273,618 survivors of COVID-19. PLoS Med. 2021;18(9):e1003773. https://doi.org/10.1371/journal.pmed.1003773.
Ballering AV, van Zon SKR, Olde Hartman TC, Rosmalen JGM, Lifelines Corona Research Initiative. Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study. Lancet. 2022;400(10350):452–61. https://doi.org/10.1016/S0140-6736(22)01214-4.
Pérez-González A, Araújo-Ameijeiras A, Fernández-Villar A, Crespo M, Poveda E, Cohort COVID-19 of the Galicia Sur Health Research Institute. Long COVID in hospitalized and non-hospitalized patients in a large cohort in Northwest Spain, a prospective cohort study. Sci Rep. 2022;12(1):3369. https://doi.org/10.1038/s41598-022-07414-x.
Dennis A, Wamil M, Kapur S, et al. Multi-organ impairment in low-risk individuals with long COVID. BMJ. 2020. https://doi.org/10.1101/2020.10.14.20212555.
• Kini A, Cao D, Nardin M, et al. Types of myocardial injury and mid-term outcomes in patients with COVID-19. Eur Heart J Qual Care Clin Outcomes. 2021;7(5):438–46. https://doi.org/10.1093/ehjqcco/qcab053. An analysis showing that patients either with pre-existing cardiovascular disease or risk factors for cardiovascular disease who had chronic myocardial injury at the index SARS-CoV2 infection had increased mortality at 6 months compared to control.
Rivera-Izquierdo M, Láinez-Ramos-Bossini AJ, de Alba IG, et al. Long COVID 12 months after discharge: persistent symptoms in patients hospitalised due to COVID-19 and patients hospitalised due to other causes-a multicentre cohort study. BMC Med. 2022;20(1):92. https://doi.org/10.1186/s12916-022-02292-6.
• Ayoubkhani D, Bermingham C, Pouwels KB, et al. Trajectory of long COVID symptoms after COVID-19 vaccination: community based cohort study. BMJ. 2022;377:e069676. https://doi.org/10.1136/bmj-2021-069676. A large observational cohort study in the UK showed that the incidence of long COVID was significantly decreased in patients who received COVID-19 vaccination.
• Antonelli M, Penfold RS, Merino J, et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case-control study. Lancet Infect Dis. 2022;22(1):43–55. https://doi.org/10.1016/S1473-3099(21)00460-6. This prospective, community-based, nested, case-control study from the UK showed that the odds of having long COVID is significantly reduced in patients who received a two dose vaccine series.
Al-Aly Z, Bowe B, Xie Y. Long COVID after breakthrough SARS-CoV-2 infection. Nat Med. 2022;28(7):1461–7. https://doi.org/10.1038/s41591-022-01840-0.
Wrapp D, Wang N, Corbett KS, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367(6483):1260–3. https://doi.org/10.1126/science.abb2507.
Kuba K, Imai Y, Rao S, et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. 2005;11(8):875–9. https://doi.org/10.1038/nm1267.
Iwasaki M, Saito J, Zhao H, Sakamoto A, Hirota K, Ma D. Inflammation triggered by SARS-CoV-2 and ACE2 augment drives multiple organ failure of severe COVID-19: molecular mechanisms and implications. Inflammation. 2021;44(1):13–34. https://doi.org/10.1007/s10753-020-01337-3.
Benigni A, Cassis P, Remuzzi G. Angiotensin II revisited: new roles in inflammation, immunology and aging. EMBO Mol Med. 2010;2(7):247–57. https://doi.org/10.1002/emmm.201000080.
Gaebler C, Wang Z, Lorenzi JCC, et al. Evolution of antibody immunity to SARS-CoV-2. Nature. 2021;591(7851):639–44. https://doi.org/10.1038/s41586-021-03207-w.
Tian S, Xiong Y, Liu H, et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol. 2020;33(6):1007–14. https://doi.org/10.1038/s41379-020-0536-x.
Wang EY, Mao T, Klein J, et al. Diverse functional autoantibodies in patients with COVID-19. Nature. 2021;595(7866):283–8. https://doi.org/10.1038/s41586-021-03631-y.
Boucher A, Desforges M, Duquette P, Talbot PJ. Long-term human coronavirus-myelin cross-reactive T-cell clones derived from multiple sclerosis patients. Clin Immunol. 2007;123(3):258–67. https://doi.org/10.1016/j.clim.2007.02.002.
Karlsson AC, Humbert M, Buggert M. The known unknowns of T cell immunity to COVID-19. Sci Immunol. 2020;5(53):eabe8063. https://doi.org/10.1126/sciimmunol.abe8063.
Meyer K, Patra T, Vijayamahantesh, Ray R. SARS-CoV-2 spike protein induces paracrine senescence and leukocyte adhesion in endothelial cells. J Virol. 2021;95(17):e0079421. https://doi.org/10.1128/JVI.00794-21.
Lei Y, Zhang J, Schiavon CR, et al. SARS-CoV-2 spike protein impairs endothelial function via downregulation of ACE 2. Circ Res. 2021;128(9):1323–6. https://doi.org/10.1161/CIRCRESAHA.121.318902.
Peluso MJ, Lu S, Tang AF, et al. Markers of immune activation and inflammation in individuals with postacute sequelae of severe acute respiratory syndrome coronavirus 2 infection. J Infect Dis. 2021;224(11):1839–48. https://doi.org/10.1093/infdis/jiab490.
Saad M, Kennedy KF, Imran H, et al. Association between COVID-19 diagnosis and in-hospital mortality in patients hospitalized with ST-segment elevation myocardial infarction. JAMA. 2021;326(19):1940–52. https://doi.org/10.1001/jama.2021.18890.
Ayoubkhani D, Khunti K, Nafilyan V, et al. Post-COVID syndrome in individuals admitted to hospital with COVID-19: retrospective cohort study. BMJ. 2021;372:n693. https://doi.org/10.1136/bmj.n693.
Tripathi B, Kumar V, Kalra A, et al. Influence of influenza infection on in-hospital acute myocardial infarction outcomes. Am J Cardiol. 2020;130:7–14. https://doi.org/10.1016/j.amjcard.2020.05.045.
Choudry FA, Rathod KS, Baumbach A, Mathur A, Jones DA. Long-term outcomes of COVID-19 associated ST-elevation myocardial infarction treated with primary PCI [published online ahead of print, 2022 May 25]. Cardiovasc Revasc Med. 2022;S1553–8389(22)00280–9.
• Kotecha T, Knight DS, Razvi Y, et al. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur Heart J. 2021;42(19):1866–78. https://doi.org/10.1093/eurheartj/ehab075. This multi-center study done in the UK found evidence of persistent myocardial injury 2 months post-discharge in 22% of patients hospitalized due to COVID-19 infection. Of these patients, 66% had no prior history of coronary disease.
Italia L, Ingallina G, Napolano A, et al. Subclinical myocardial dysfunction in patients recovered from COVID-19. Echocardiography. 2021;38(10):1778–86. https://doi.org/10.1111/echo.15215.
Morrow AJ, Sykes R, McIntosh A, et al. A multisystem, cardio-renal investigation of post-COVID-19 illness. Nat Med. 2022;28(6):1303–13. https://doi.org/10.1038/s41591-022-01837-9.
Hendrickson BS, Stephens RE, Chang JV, et al. Cardiovascular evaluation after COVID-19 in 137 collegiate athletes: results of an algorithm-guided screening. Circulation. 2021;143(19):1926–8. https://doi.org/10.1161/CIRCULATIONAHA.121.053982.
• Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. 2021;594(7862):259–64. https://doi.org/10.1038/s41586-021-03553-9. A large VA database analysis showing that patients with post-acute sequelae of COVID-19 infection at 6 months had a disease burden that was nearly 4 times greater than control for heart failure and 8 times greater than control for arrhythmias.
Daugherty SE, Guo Y, Heath K, et al. Risk of clinical sequelae after the acute phase of SARS-CoV-2 infection: retrospective cohort study. BMJ. 2021;373:n1098. https://doi.org/10.1136/bmj.n1098.
• Romero-Duarte Á, Rivera-Izquierdo M, Guerrero-Fernández de Alba I, et al. Sequelae, persistent symptomatology and outcomes after COVID-19 hospitalization: the ANCOHVID multicentre 6-month follow-up study. BMC Med. 2021;19(1):129. https://doi.org/10.1186/s12916-021-02003-7. A retrospective observational study in Spain showing that 3.1% of patients with long COVID were found to have an identifiable arrhythmia or symptomatic palpitations 6 months after the index SARS-CoV2 infection.
Zhou M, Wong CK, Un KC, et al. Cardiovascular sequalae in uncomplicated COVID-19 survivors. PLoS ONE. 2021;16(2):e0246732. https://doi.org/10.1371/journal.pone.0246732.
Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of long COVID [published correction appears in Nat Med. 2021 Jun; 27(6):1116]. Nat Med. 2021;27(4):626–31. https://doi.org/10.1038/s41591-021-01292-y.
Xiong Q, Xu M, Li J, et al. Clinical sequelae of COVID-19 survivors in Wuhan, China: a single-centre longitudinal study. Clin Microbiol Infect. 2021;27(1):89–95. https://doi.org/10.1016/j.cmi.2020.09.023.
Asadi-Pooya AA, Akbari A, Emami A, et al. Risk factors associated with long COVID syndrome: a retrospective study. Iran J Med Sci. 2021;46(6):428–36. https://doi.org/10.30476/ijms.2021.92080.2326.
Ingul CB, Grimsmo J, Mecinaj A, et al. Cardiac dysfunction and arrhythmias 3 months after hospitalization for COVID-19. J Am Heart Assoc. 2022;11(3):e023473. https://doi.org/10.1161/JAHA.121.023473.
Kim S, Pellot I, Kim M, Cho JH, Cingolani E. The incidence of cardiac arrhythmias in patients with COVID-19: a meta-analysis. J Am Coll Cardiol. 2022;79(9_Supplement):2143.
Peretto G, Sala S, Rizzo S, et al. Ventricular arrhythmias in myocarditis: characterization and relationships with myocardial inflammation. J Am Coll Cardiol. 2020;75(9):1046–57. https://doi.org/10.1016/j.jacc.2020.01.036.
Goodman BP, Khoury JA, Blair JE, Grill MF. COVID-19 dysautonomia. Front Neurol. 2021;12:624968. https://doi.org/10.3389/fneur.2021.624968.
Buoite Stella A, Furlanis G, Frezza NA, Valentinotti R, Ajcevic M, Manganotti P. Autonomic dysfunction in post-COVID patients with and witfhout neurological symptoms: a prospective multidomain observational study. J Neurol. 2022;269(2):587–96. https://doi.org/10.1007/s00415-021-10735-y.
Dweck MR, Bularga A, Hahn RT, Bing R, Lee KK, Chapman AR, et al. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J Cardiovasc Imaging. 2020;21(9):949–58. https://doi.org/10.1093/ehjci/jeaa178. PMID: 32556199; PMCID: PMC7337658.
Maestre-Muñiz MM, Arias Á, Mata-Vázquez E, et al. Long-term outcomes of patients with coronavirus disease 2019 at one year after hospital discharge. J Clin Med. 2021;10(13):2945. https://doi.org/10.3390/jcm10132945.
Evans RA, McAuley H, Harrison EM, et al. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID): a UK multicentre, prospective cohort study [published correction appears in Lancet Respir Med. 2022 Jan; 10(1):e9]. Lancet Respir Med. 2021;9(11):1275–87. https://doi.org/10.1016/S2213-2600(21)00383-0.
Yao TC, Huang YW, Chang SM, Tsai SY, Wu AC, Tsai HJ. Association between oral corticosteroid bursts and severe adverse events : a nationwide population-based cohort study. Ann Intern Med. 2020;173(5):325–30. https://doi.org/10.7326/M20-0432.
Moody WE, Liu B, Mahmoud-Elsayed HM, et al. Persisting adverse ventricular remodeling in COVID-19 survivors: a longitudinal echocardiographic study. J Am Soc Echocardiogr. 2021;34(5):562–6. https://doi.org/10.1016/j.echo.2021.01.020.
Sonnweber T, Sahanic S, Pizzini A, et al. Cardiopulmonary recovery after COVID-19: an observational prospective multicentre trial. Eur Respir J. 2021;57(4):2003481. https://doi.org/10.1183/13993003.03481-2020.
Li X, Wang H, Zhao R, et al. Elevated extracellular volume fraction and reduced global longitudinal strains in participants recovered from COVID-19 without clinical cardiac findings. Radiology. 2021;299(2):E230–40. https://doi.org/10.1148/radiol.2021203998.
Günay N, Demiröz Ö, Kahyaoğlu M, et al. The effect of moderate and severe COVID-19 pneumonia on short-term right ventricular functions: a prospective observational single pandemic center analysis. Int J Cardiovasc Imaging. 2021;37(6):1883–90. https://doi.org/10.1007/s10554-021-02171-w.
Shirokov NE, Yaroslavskaya EI, Krinochkin DV, Osokina NA. Hidden systolic dysfunction of the right ventricle in patients with increased pulmonary vascular resistance 3 months after COVID-19 pneumonia. Kardiologiia. 2022;62(3):16–20. https://doi.org/10.18087//cardio.2022.3.n1743.
• Pelà G, Goldoni M, Cavalli C, et al. Long-term cardiac sequelae in patients referred into a diagnostic post-COVID-19 pathway: the different impacts on the right and left ventricles. Diagnostics (Basel). 2021;11(11):2059. https://doi.org/10.3390/diagnostics11112059. A cohort study showing that up to 39% of patients with persistent symptoms 5 months after initial COVID-19 infection may have some abnormality appreciable on echocardiogram.
• Dennis A, Wamil M, Alberts J, et al. Multiorgan impairment in low-risk individuals with post-COVID-19 syndrome: a prospective, community-based study. BMJ Open. 2021;11(3):e048391. https://doi.org/10.1136/bmjopen-2020-048391. A prospective cohort study showing that even among low-risk patients with PCS, up to 9% may have some form of systolic dysfunction appreciable on CMR.
Dweck MR, Bularga A, Hahn RT, et al. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J Cardiovasc Imaging. 2020;21(9):949–58. https://doi.org/10.1093/ehjci/jeaa178.
Scally C, Rudd A, Mezincescu A, et al. Persistent long-term structural, functional, and metabolic changes after stress-Induced (Takotsubo) cardiomyopathy. Circulation. 2018;137(10):1039–48. https://doi.org/10.1161/CIRCULATIONAHA.117.031841.
Basso C, Leone O, Rizzo S, et al. Pathological features of COVID-19-associated myocardial injury: a multicentre cardiovascular pathology study. Eur Heart J. 2020;41(39):3827–35. https://doi.org/10.1093/eurheartj/ehaa664.
Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) [published correction appears in JAMA Cardiol. 2020 Nov 1;5(11):1308]. JAMA Cardiol. 2020;5(11):1265–73. https://doi.org/10.1001/jamacardio.2020.3557.
Raman B, Cassar MP, Tunnicliffe EM, et al. Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. EClinicalMedicine. 2021;31:100683. https://doi.org/10.1016/j.eclinm.2020.100683.
Ng MY, Ferreira VM, Leung ST, et al. Patients recovered from COVID-19 show ongoing subclinical myocarditis as revealed by cardiac magnetic resonance imaging. JACC Cardiovasc Imaging. 2020;13(11):2476–8. https://doi.org/10.1016/j.jcmg.2020.08.012.
Wang H, Li R, Zhou Z, et al. Cardiac involvement in COVID-19 patients: mid-term follow up by cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2021;23(1):14. https://doi.org/10.1186/s12968-021-00710-x.
Rajpal S, Tong MS, Borchers J, et al. Cardiovascular magnetic resonance findings in competitive athletes recovering from COVID-19 infection [published correction appears in JAMA Cardiol. 2021 Jan 1;6(1):123]. JAMA Cardiol. 2021;6(1):116–8. https://doi.org/10.1001/jamacardio.2020.4916.
Małek ŁA, Marczak M, Miłosz-Wieczorek B, et al. Cardiac involvement in consecutive elite athletes recovered from Covid-19: a magnetic resonance study. J Magn Reson Imaging. 2021;53(6):1723–9. https://doi.org/10.1002/jmri.27513.
Daniels CJ, Rajpal S, Greenshields JT, et al. Prevalence of clinical and subclinical myocarditis in competitive athletes with recent SARS-CoV-2 infection: results from the Big Ten COVID-19 Cardiac Registry. JAMA Cardiol. 2021;6(9):1078–87. https://doi.org/10.1001/jamacardio.2021.2065.
Clark DE, Parikh A, Dendy JM, et al. COVID-19 myocardial pathology evaluation in athletes with cardiac magnetic resonance (COMPETE CMR) [published correction appears in Circulation. 2021 Feb 9;143(6):e238]. Circulation. 2021;143(6):609–12. https://doi.org/10.1161/CIRCULATIONAHA.120.052573.
Martinez MW, Tucker AM, Bloom OJ, et al. Prevalence of inflammatory heart disease among professional athletes with prior COVID-19 infection who received systematic return-to-play cardiac screening. JAMA Cardiol. 2021;6(7):745–52. https://doi.org/10.1001/jamacardio.2021.0565.
Eiros R, Barreiro-Pérez M, Martín-García A, et al. Afección pericárdica y miocárdica tras infección por SARS-CoV-2: estudio descriptivo transversal en trabajadores sanitarios [Pericardial and myocardial involvement after SARS-CoV-2 infection: a cross-sectional descriptive study in healthcare workers] [published online ahead of print, 2022 Jan 13]. Rev Esp Cardiol. 2022. https://doi.org/10.1016/j.recesp.2021.10.021.
Piazza G, Campia U, Hurwitz S, et al. Registry of arterial and venous thromboembolic complications in patients with COVID-19. J Am Coll Cardiol. 2020;76(18):2060–72. https://doi.org/10.1016/j.jacc.2020.08.070.
Mandal S, Barnett J, Brill SE, et al. ‘Long-COVID’: a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax. 2021;76(4):396–8. https://doi.org/10.1136/thoraxjnl-2020-215818.
Albert A, Jacob J, Malchair P, et al. Predictors of revisits within 1 year by patients after acute COVID-19: the HUBCOVID365 cohort study. Predictores de revisita en pacientes con infección aguda COVID-19 con seguimiento al año: estudio de cohorte HUBCOVID365. Emergencias. 2022;34(1):38–46.
•• Writing Committee, Gluckman TJ, Bhave NM, et al. 2022 ACC Expert consensus decision pathway on cardiovascular sequelae of COVID-19 in adults: myocarditis and other myocardial involvement, post-acute sequelae of SARS-CoV-2 infection, and return to play: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022;79(17):1717–1756. https://doi.org/10.1016/j.jacc.2022.02.003. This is the expert decision pathway released by the American College of Cardiology on the topic of cardiovascular sequelae of COVID-19.
• Writing Committee Members, Gulati M, Levy PD, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;78(22):e187-e285. https://doi.org/10.1016/j.jacc.2021.07.053. This is the consensus statement by leading organizations on clinical practice guidelines regarding the evaluation and diagnosis of chest pain. These guidelines should continue to be followed when performing an ischemic evaluation in the setting of cardiovascular sequelae due to COVID-19 infection.
Gorecka M, McCann GP, Berry C, et al. Demographic, multi-morbidity and genetic impact on myocardial involvement and its recovery from COVID-19: protocol design of COVID-HEART-a UK, multicentre, observational study. J Cardiovasc Magn Reson. 2021;23(1):77. https://doi.org/10.1186/s12968-021-00752-1.
Arévalos V, Ortega-Paz L, Fernandez-Rodríguez D, et al. Long-term effects of coronavirus disease 2019 on the cardiovascular system, CV COVID registry: a structured summary of a study protocol. PLoS ONE. 2021;16(7):e0255263. https://doi.org/10.1371/journal.pone.0255263.
Besnier F, Bérubé B, Malo J, et al. Cardiopulmonary rehabilitation in long-COVID-19 patients with persistent breathlessness and fatigue: the COVID-Rehab Study. Int J Environ Res Public Health. 2022;19(7):4133. https://doi.org/10.3390/ijerph19074133.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Ischemic Heart Disease
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mohammad, K.O., Lin, A. & Rodriguez, J.B.C. Cardiac Manifestations of Post-Acute COVID-19 Infection. Curr Cardiol Rep 24, 1775–1783 (2022). https://doi.org/10.1007/s11886-022-01793-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-022-01793-3