Abstract
Purpose of Review
Childhood-onset systemic lupus erythematosus (cSLE) is a severe and potentially life-threatening chronic autoimmune disease. cSLE is more aggressive and has poorer outcomes than adult-onset disease. The global burden of cSLE is poorly understood, with most publications on cSLE originating from high-resourced settings. The reports from less resourced settings indicate high morbidity and mortality in these populations.
Recent Findings
In this article, we review the disparities in global access to rheumatology care and research for patients with cSLE. We highlight recent cSLE advances from all regions of the globe. We describe current obstacles to cSLE clinical care and research in all settings. Finally, we propose a path forward for high quality, equitable and accessible care to individuals with cSLE everywhere.
Summary
Individuals with cSLE are at risk for morbidity and death, yet patients worldwide face challenges to adequate access to care and research. Sustained, collaborative efforts are needed to create pathways to improve care and outcomes for these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood-onset systemic lupus erythematosus (cSLE) is a systemic autoimmune disease with no known cure. Approximately one in every five patients has disease onset in childhood years. The patients with onset in childhood years have more severe disease and worse outcomes [1]. Individuals with cSLE acquire more organ damage than adult counterparts, despite having fewer comorbidities [2]. Although this patient group is at high risk for early mort
ality and morbidity, [3] there is a paucity of research on this population. Here, we summarize recent global advances in cSLE, summarized according to geographic region. Additionally, we acknowledge that many health disparities align across higher incomes countries (HIC) in the Global North (defined as North America, Europe, Israel, Japan, South Korea, New Zealand and Australia,) and lower to middle income countries (LMIC) in the Global South (broadly comprised of Africa, Asia excluding Japan and South Korea, and the South Pacific excluding Australia and New Zealand) [4]. We describe challenges to cSLE research in different settings, and outline a path forward towards addressing gaps in cSLE care and research globally.
Recent Advances in cSLE by Region
Asia–Pacific
The Asia–Pacific region is home to approximately 4.3 billion people, (about 60% of the world’s population) and about 25% are children under 15 years of age [5]. Despite a lack of robust epidemiologic studies defining the incidence or prevalence of cSLE in Asia, more than 100,000 children are estimated to have lupus in the Asia–Pacific region [6]. Asian children are more likely to have oral ulcers and neuropsychiatric disease, [7] and have higher disease activity at presentation, possibly due to delay in diagnosis [8]. Damage accrual is comparable to that found in patients with cSLE in the United Kingdom [9]. In Southeast Asia, age of cSLE onset is similar to reports from high income countries (HIC) (with some regional differences), [10] but patients exhibit severe disease, with high disease activity scores, high rates of proliferative lupus nephritis (LN), and other organ involvement. An Australian retrospective longitudinal cohort study of patients with cSLE reported higher rates of SLE in the Indigenous population, high prevalence of LN (64%) and high rates of organ damage [11].
Management of cSLE in Asia–Pacific regions remains a challenge. Recent data from Thailand showed that only 47% of children achieved low lupus disease activity state (LLDAS) after 12 months of treatment, [9] while in India it was achieved by 57.7% of children enrolled in an inception cohort, [12] indicating a huge gap remains in achieving treat-to-target in all patients. Infections, including bacterial, viral and mycobacterial infections, are a major issue in managing patients as they are significant contributors to morbidity and mortality [13]. Mortality in the region is higher than in HIC, but some regions have shown improvement in recent years. However, infections remain the leading cause of mortality in this population. For patients with severe LN who progress to end-stage kidney disease (ESKD), the high cost of renal replacement therapy in low to middle income countries (LMIC) makes this therapy inaccessible to many patients. Lack of access to therapy further increases the mortality due to nephritis in these areas [14].
Recently, important advances in translational research have come from the Asia–Pacific region. In a recent analysis of more than 35,000 SLE patients GWAS data from European and Han Chinese ancestry it was revealed that many loci confer SLE susceptibility across ancestry, but some are specifically seen in Asian patients. A novel SLC23A9 intronic variant was disease associated in Han Chinese SLE patients [15]. This variant impairs lysosomal function and may lead to increased TLR signaling, which has been recognized in many recent studies as pivotal to cSLE pathogenesis [16]. The Asia–Pacific region is ancestrally diverse, therefore dedicated genomic and translational studies which focus on the various populations in this region are needed.
Africa
The African continent is home to almost 1.5 billion diverse individuals. Despite evidence worldwide that lupus is more common and more severe in people of African ancestry, there are fewer cases reported of childhood or adult-onset lupus from Africa compared to Europe and North America [17]. This lack of reporting reflects the lack of access to appropriate care for diagnosis and testing rather than a true lack of disease, and those of us working on the continent know that the burden of lupus in Africa is large and severely underestimated [18]. Diagnostic challenges are widespread across the continent [19]. A systematic review of LN diagnosis revealed less than 20% of studies used the recommended LN classification criteria, with better reporting and survival noted in the North African countries [19].
Data on SLE in Africa primarily comes from adult populations. The largest study to date, a meta-analysis of 896 in-hospital adult-onset SLE (aSLE) cases from 15 studies in sub-Saharan Africa, estimates an in-hospital prevalence of 1.7% for lupus [20]. The mean age of SLE onset in this analysis was 28 years, younger than in the Northern hemisphere. Infection still poses a major survival threat to lupus patients in sub-Saharan Africa: in a recent study reported a 43% mortality rate among lupus patients admitted, almost all deaths were due to infections and renal disease [21]. Other risk factors associated with death included fever, disease flare, musculoskeletal involvement, and depression [21]. A recent review and meta-analysis on the global tuberculosis (TB) incidence and prevalence in individuals with SLE noted an increased prevalence in regions. with a high TB burden, like Africa [22]. Extra pulmonary TB (EPTB) patients were significantly younger, developed TB sooner after SLE diagnosis, and had more active disease compared to pulmonary TB (PTB) patients [22].
There are even fewer studies of childhood-onset lupus than adult-onset in Africa, largely limited to small case series and case reports [23, 24]. The pediatric SLE (PULSE) cohort in South Africa, one of the largest established cohorts of individuals with cSLE in Africa to date, reports patients have a similar mean age of diagnosis and female predominance compared to those reported from North America. Notably, individuals with cSLE in this cohort had high disease activity, multi-organ involvement at diagnosis and significant disease damage at enrollment [25,26,27], suggesting delays in diagnosis. Qualitative studies in South Africa and Ghana reported caregivers of lupus patients face challenges including lack of exposure or awareness of the disease, financial hardships, and the social stigma of SLE. Health system barriers to an cSLE diagnosis were identified as lack of rheumatology informed healthcare workforce, a complexity of the medical system, and misdiagnosis [26, 28, 29]. Similar issues were reported in Kenya, revealing gaps in pediatric rheumatology knowledge amongst healthcare workers that contribute to delayed diagnosis and suboptimal management [30].
The formation of The Pediatric Society of the African League Against Rheumatism(PAFLAR) represents an important advance for cSLE research in Africa [31]. PAFLAR offers opportunities among African health workers treating children with rheumatic and musculoskeletal diseases to collaborate and disseminate information and improve the outcomes for patients. PAFLAR facilitates learning and collaboration through monthly educational webinars with a hybrid, synchronous and asynchronous learning platform, an annual hybrid congress uniting experts, healthcare professionals, and stakeholders in the field from over 73 countries across 5 continents, and the PAFLAR registry, which creates the opportunity to collect multi-center standardized data across the African continent. While in the early stages, this registry lays the foundation for future clinical and translational cSLE projects. PAFLAR has patient-centered care as a focus, highlighted in a pioneer project of Therapeutic Patient Education (TPE) for children with rheumatic disease across different regions in Africa. The PAFLAR efforts highlight the advances that can be made through collaborative efforts by leaders in Africa.
While there are few clinical studies which focus on cSLE in Africa, there are even fewer translational research studies from this region. A collaborative, multinational study on the genetics of cSLE included patients from South Africa, and identified many novel, rare SLE risk variants, supporting evidence from HIC that cSLE patients are enriched in rare variants [32].
South America
South America, with 447 million people ( almost half of whom live in Brazil), consists of 13 countries, with important differences in economics and healthcare access between regions [33]. There are no comprehensive studies on cSLE prevalence and incidence across South America. Some countries including Brazil and Argentina have pediatric rheumatologists, but other countries still lack any pediatric rheumatology providers [34].
The Brazilian Multicenter Group of Children and Adolescents with Pediatric Systemic Lupus Erythematosus (Brazilian Childhood-onset SLE Registry Group) is an observational cohort, with 1528 patients with cSLE from 27 university centers in Brazil [35]. They reported higher disease activity associated with earlier age of onset of lupus (< 6 years) in this cohort. Patients with cSLE in this cohort had higher rates of LN and neuropsychiatric SLE, and higher mortality rates than in HIC [36]. The main causes of death in this cohort were infections (sepsis and opportunistic infections) and alveolar hemorrhage. Patients with ESKD and central nervous system (CNS) SLE had a higher mortality risk, likely due to the severe disease and intense immunosuppression increasing infection susceptibility. Patients with cSLE with positive dsDNA, low C3, and proteinuria were at risk for early-onset LN, increased morbidity, and higher mortality [37]. In those with LN, 5.4% developed chronic kidney disease (CKD); those with proliferative LN on biopsy and CKD had lower survival rates [36]. Axonal dysfunction in patients with cSLE in Brazil correlated with levels of interferon (IFN)-γ and symptoms of depression. Measuring axonal dysfunction may be a way to predict NP-SLE [38]. Although the Brazilian Childhood-onset SLE Registry Group is a large multicenter cohort, they represent a single country and cannot be assumed to represent all of South America or other areas of the world. Individuals with cSLE in this region are more likely to have 1st and 2nd degree relatives with SLE than aSLE patients, supporting enrichment of genetic drivers of disease in this population [39]. More dedicated genomic and translational studies in South America are needed to explore the biologic drivers of cSLE in this population.
Europe
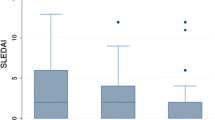
Europe, though smaller in geographical area and population than Asia, Africa, or South America, has many HIC with access to pediatric rheumatology care and research. A significant recent advance in cSLE clinical studies of cSLE is the development of Treat-to-target (T2T) strategies for cSLE. Interest in adopting T2T approaches is growing on a global scale for both cSLE [40,41,42,43,44,45] and aSLE [46]. Extensive validation of T2T endpoints in aSLE has demonstrated improved outcomes, including reduced organ damage [47,48,49,50,51,52], fewer flares [53], glucocorticoid sparing [50, 53], improved quality of life [54], and lower healthcare costs [55], though no randomized trials have assessed the efficacy of this approach. The UK’s TARGET LUPUS© research program has been established to develop T2T strategies for cSLE [40, 41]. An International cSLE T2T Task Force, including cSLE experts from the principle professional networks (PReS, CARRA, UK JSLE) across six continents. Together the Task Force has developed ‘principles and points to consider for cSLE T2T’, endorsed by the Paediatric Rheumatology European Society (PReS) [56]. They have also created consensus based, age-appropriate target definitions, including Childhood Lupus Low Disease Activity State (cLLDAS), cSLE clinical remission on steroids (cCR), and cSLE clinical remission off steroids (cCR-0) [57]. These definitions sufficiently align with the aSLE definitions, while incorporating changes to improve applicability to cSLE [57]. Future efforts are needed to validate cSLE T2T endpoints.
The Treatment Response Measure for SLE (TRM-SLE) Taskforce is developing a new clinical outcome assessment (COA) for SLE clinical trials to capture treatment effects that hold clinical significance for both patients and practitioners, aiming to serve as a trial endpoint conducive to regulatory endorsement of new SLE treatments. This COA addresses the historical challenges of gauging meaningful treatment responses in SLE, as legacy disease activity metrics did not originate within a clinical trial setting and did not integrate substantial patient input in their design, as contemporary COA guidelines recommend [58, 59].
Emphasizing a life-course approach, the TRM-SLE Task Force has incorporated pediatric rheumatologists in its steering committee and workgroups to ensure the inclusion of pediatric perspectives in defining measurement goals, selecting assessments, and establishing consensus on domain scoring and treatment response criteria. This strategy aims to help to expedite the available treatments for younger patients, who often experience more severe disease trajectories and outcomes, thereby addressing a critical gap in therapeutic development [60]. By designing the TRM-SLE with inherent suitability for both cSLE and aSLE populations, the initiative is poised to enhance methodological robustness in aSLE and cSLE trials, increasing the likelihood of their success, and ensuring that trial endpoints are relevant and applicable across the patient lifespan [58, 59].
There have been numerous advances in cSLE translational research, specifically genomics, in Europe in recent years [61,62,63,64,65]. Gene variants regulating Type I IFNs have are important in the pathogenesis of cSLE; including those associated with primary and secondary interferonopathies [61]. Elevated Type I IFN levels induce autoantibody production and switch the production of non-neutralizing to neutralizing antibodies [62]. One study identified pathogenic genetic variants in 3.5% of a UK cSLE cohort, with 75% of those genes modifying Type I IFN production [63]. Dedicator of cytokinesis 11 (DOCK11) variants, causing deficiency of DOCK11 and disturbance of platelet morphology, have been reported in eight French patients with cSLE [64]. Variants in Protein kinase C delta (PRKCD) have been implicated in cSLE development, [66] with a recent study demonstrating that these variants upregulate the PI3K/mTOR pathway [65].
A Netherlands-based study has used targeted multiomics to stratify patients with cSLE into different biological phenotypes. This pilot study of 17 patients with cSLE employed unsupervised hierarchical clustering and high-dimensional flow cytometry to identify three unique clusters characterized by different sets of genes, cytokines, and disease activity states [67]. It is crucial that patients from ethnically and ancestrally diverse backgrounds are included in future translational cSLE studies to fully advance understanding of cSLE, with validation of results in ethnically distinct patient cohorts. CSLE studies have the disadvantage of being relatively small compared to adult studies. Collaborative efforts, such as the British-French studies investigating the genetics of cSLE cohorts, [68] are encouraging, but further work is required in larger, more diverse patient populations.
North America
Similar to Europe, a small share of the world’s pediatric population resides in North America, but this region is well-resourced with better access to clinical care and research than regions in LMIC. Despite these resources, children with SLE in North America continue to be a high-risk population. The most severe disease manifestations such as LN and neuropsychiatric lupus (NP SLE) are ongoing research priorities in cSLE [69]. Individuals with cSLE are at risk for lupus nephritis. In the Childhood Arthritis and Rheumatology Research Alliance (CARRA) registry, 32% of children with lupus had renal disease [70]. Black patients were more likely to have progression of renal disease over the 2 year follow up period, but the role of systemic inequity could not be analyzed properly in this retrospective report. Another study reported male patients or those with older age at disease onset were more likely to have abnormal kidney function in short-term follow up, although a large variation was observed [71]. Patients with LN who require hospitalization are at high risk for readmission, with nearly 20% readmitted after discharge [72]. NP SLE is more common in cSLE, with more prevalent depression, anxiety and cognitive dysfunction in cSLE than unaffected peers of the same age, [73] which can affect medication adherence and quality of life [74, 75]. Cardiovascular disease is an important driver of SLE mortality. Abnormal blood pressure has been identified as an important predictor of renal damage and cardiac disease. Loss of the physiologic dipping of nocturnal blood pressure is prevalent in cSLE and is associated with atherosclerotic changes [76]. Patients with cSLE are at higher risk for heart failure, with hypertension and cardiac involvement likely important contributors to this risk [77].
Health disparities have been reported in individuals with cSLE, and mirror those of aSLE, where Black and Hispanic patients have higher morbidity and mortality than White counterparts [78]. Systemic racism affects health outcomes across all diseases, and SLE is no different. Inequitable inclusion in registries and clinical trials and lack of data can exacerbate existing disparities [79]. The adolescent period is a vulnerable time, as patients who are undergoing developmental stages of adolescence which include rebellion and concrete thinking often struggle with adhering to medications. The transition time, where patients must change from pediatric to adult care, has been identified as high-risk period for delays or lapses in care, culminating in disease flare [80,81,82].
Childhood-onset SLE patients, with early age of onset and more severe disease, may be a population enriched in genetic risk variants. Common variant studies have demonstrated that individuals with cSLE have similar or increased number of common SLE risk variants when compared to adult-onset patients, with some variation in ancestry [83]. Other studies have found differing associations with age of onset and association with common variants inside and outside the HLA region [84]. Many studies have reported an enrichment of rare, damaging SLE risk variants in cSLE cohorts, [32] with rates of 10–13% of cohorts when investigating with next generation sequencing [85]. Additional studies are needed to identify both known and novel risk genes in cSLE cohorts.
Optimizing treatment remains challenging in cSLE, due to highly heterogenous disease presentations with a lack of reliable predictors of prognosis or flares. Few clinical trials have focused on cSLE, and children/adolescent patients are infrequently included in adult clinical trials. Therefore, treatment protocols are often extrapolated from adult trials, and refined with case series or observational data. Cyclophosphamide (CYC) remains an important therapy for the severe manifestations such as NPSLE and LN. Recently, it was reported that pediatric rheumatologists were familiar with EuroLupus dosing regimens of CYC, and are using this more frequently than a decade ago [86]. A multicenter retrospective study did not find significant differences between EuroLupus or NIH protocol in children and adolescents with SLE [87]. Prospective trials with proper randomization are needed to compare these regimens. A retrospective study of 21 patients with cSLE from a single center revealed that individuals who received belimumab were able to reduce glucocorticoid dose [88]. Few patients in the study had lupus nephritis, but this trend may change over time. In the past few years, anti- CD-19 chimeric antigen receptor (CAR) T therapy has emerged as an exciting new therapy for refractory SLE patients [89]. These cells target eliminate CD-19 positive B cells, including pathogenic autoreactive B cells, and have demonstrated sustained remission in refractory patients [90]. While it has not yet been studied in patients who are below the age of 18, many of these refractory patients in the initial case series had age of onset before 18, again demonstrating the high severity of cSLE. These studies may provoke researchers to consider this therapy for very severe patients who are not yet adult age. Long term data about the risks and benefits will help to guide this decision.
Shared Challenges in Caring for Individuals with cSLE
Access to Care
There is no region of the world that has sufficient access to pediatric rheumatology for cSLE care [91,92,93]. Many areas of the world with the greatest number of pediatric individuals have few or no pediatric rheumatology providers [94]. In LMIC, musculoskeletal diseases are not a priority among the non-communicable leading to a lack of government funding [95]. Furthermore, access to proper cSLE diagnosis and therapy usually occurs in tertiary care hospitals in major urban centers, which translates to long travel distance for specialist care [29, 96, 97]. (Fig. 1A) This increases the cost of care as well as the indirect cost of travel and loss of wages. Even in tertiary care centers, limits of access to diagnostics and high out of pocket cost of medications and diagnostics limit access to equitable care for cSLE [98]. Large travel distances, lack of access to trained rheumatologists, affordable diagnostics and medicines all create barriers to SLE diagnosis and follow-up care, which can translate to permanent damage for individuals with cSLE (Fig. 1A) [99, 100].
Even when there is a trained pediatric rheumatologist in a region, sustained training to ensure access to care can be difficult. Sole providers are often overwhelmed with clinical demands, making it difficult to establish a formal training program as there is little time or funding for these efforts. Most pediatric rheumatology trainees are found in countries with large rheumatology workforces, reflecting the need for a critical mass of providers to sustain clinical training. limited exposure to pediatric rheumatology during medical school and pediatric training hinders development of a sustainable pediatric rheumatology workforce [101]. The absence of a local training program, the cost and burden of extended travel for fellowship training impede the development of the pediatric rheumatology workforce (Fig. 1A).
Limited data from patients with cSLE globally hinders understanding of the true burden and impact of cSLE. Key obstacles include: patients with cSLE are a smaller patient population than aSLE, and few multicenter prospective studies or clinical trial have been executed in this population. The lack of research training and infrastructure in LMIC remains a barrier to advancing cSLE research [102]. Inconsistent data collection methods, at the regional, national and international level, impede comparative studies. Lack of sustained research funding in LMICs further restricts advancing research, even if there are trained physician scientists in the region. There is enormous phenotypic and genetic diversity in Africa, the Asia–Pacific, and South America, and the lack of inclusion of diverse patients in lupus research decreases the global odds of meaningful translational research discovery. Inclusive research encompassing diverse geographic and ancestral diversity of patients with cSLE is crucial for efficient and economical use of research funding to investigate lupus.
Solutions
Training
Training of medical graduates and pediatric postgraduates in early recognition of cSLE is important. These efforts would include, but not be limited to, training of medical students, family physicians, and pediatricians in the primary health care network in cSLE, with focus on early recognition and diagnosis, and referral to specialized centers for appropriate treatment. This training can be implemented by medical schools, courses or training given by pediatric rheumatologists, or promoted by local or regional rheumatology associations/leagues such as APLAR, PAFLAR, PANLAR, EULAR, and CARRA (Fig. 1B) [103, 104]. These courses should be periodic until they reach all first-line health care workers who may care for individuals with childhood-onset systemic lupus erythematosus. Interval courses for general pediatricians and general practitioners can be supported with online education such as the open access virtual training website Pediatric Musculoskeletal Matters [96] which provides training resources in many languages for healthcare providers caring for patients with rheumatic disease. Additionally, dedicated programs and funding for training pediatric rheumatologists in underserved regions are needed.
Access to Care
Access to care can be improved at many levels. We should create region-specific guidelines for diagnosis, management, and referral, as well as educational programs related to symptom identification, therapeutic strategies, and effective communication skills [105]. Diagnostic and therapeutic guidelines and algorithms are developed and tested in HIC (including USA and Europe), based on patient phenotypes and access to care that may differ greatly from many LMIC. We need to report cSLE cases worldwide so that we may include children from LMIC in global data and develop and test diagnostic and treatment protocols tailored to these patients and their context. Recently, guidelines for juvenile arthritis in less resourced settings were published, and a similar effort in cSLE is recommended by this group [106]. Training, as described above, is a critical piece of sustainable access to care [25, 26]. Healthcare systems should be bolstered to improve affordable healthcare and access to well-developed multi-disciplinary care [105].
A strategy practiced in LMIC sites (namely India) that deserves further study is using expensive tests sparingly (at time of flare or suspected infection) to reduce cost. Other low-cost studies (urine studies, blood pressure monitoring) could be made available in or near home followed by teleconsultation. Telehealth can improve access to care and should be used in combination with occasional in-person visits, tailored for disease activity, travel burden, and patient preference (Fig. 1B) [107]. The authors recognize the need for study of pragmatic approaches to care which is the currently reality for many settings. These protocols should consider availability of medications in the setting, and region-specific risks. Some examples of such management may include studying the use of low-cost therapies, and using minimal steroids to reduce infection rates as infection load is higher in certain areas, such as those with endemic tuberculosis [108]. We continue to advocate for equitable cSLE care, and advocate for policies and programs that will enable equity. Equitable care does not mean universal guidelines, but rather location-specific guidelines that provide optimal care for the setting.
In addition, we need to establish robust referral pathways for better utilization of resources.
Raising awareness in the general public may improve awareness of patients and caregivers and mitigate some stigma of cSLE [25, 26]. Improving education about SLE at diagnosis holds potential to increase caregiver-physician trust and lower fear [25, 26]. Proposed patient interventions to be considered include social support in addition to education [105]. Community interventions that can be implemented include outreach awareness campaigns, mobilizing monetary support for patients’ care, and mobilizing patients to access diagnostic and therapeutic interventions [105].
Access to Research
One of the biggest challenges for lupus in less resourced settings is to recognize and report cases to advocate for the allocation of resources for care and research. Improving awareness and training among healthcare professionals at all levels would improve diagnosis, reporting, and create data to inform governments when allotting healthcare budgets [102]. National registries such as CARRA, PAFLAR, JIR, and UKSLE have made progress at the regional level. Recently, a team of cSLE experts convened to create infrastructure to harmonize registries across the world [109]. We call on the international lupus research community to support the inclusion of children from LMIC in global grant applications and lupus research. Funding such large registries will allow practitioners to understand cSLE natural history and factors that lead to poor outcomes in historically understudied areas. Further, we call upon policy makers and funders to create a strong and varied mechanism for funding global SLE research. We advocate for ensuring research priorities in LMIC are determined by researchers from these locations, with robust and sustained funding support which recognizes local expertise [110]. Understanding the longitudinal outcome of systemic lupus erythematosus across different countries through research and data can elucidate the role of genetics, environmental exposures, and other factors in the progression of the disease [21].
Conclusions
cSLE is a chronic, organ and life-threatening disease which begins before adulthood and confers a high risk of early mortality. The literature review of cSLE by region highlights the disparity in clinical and translational research from high-, middle-, and low-income settings. We call upon the global pediatric rheumatology community to create funding and infrastructure to begin to provide access to care and research for all children with SLE, regardless of location.
Data Availability
No datasets were generated or analysed during the current study.
References
Ardoin SP, Schanberg LE. Paediatric rheumatic disease: lessons from SLE: children are not little adults. Nat Rev Rheumatol. 2012;8(8):444–5.
Mina R, Brunner HI. Pediatric lupus–are there differences in presentation, genetics, response to therapy, and damage accrual compared with adult lupus? Rheumatic Dis Clin North Am. 2010;36(1):53–80.
Harry O, Yasin S, Brunner H. Childhood-Onset Systemic Lupus Erythematosus: A Review and Update. J Pediatr. 2018;196:22-30.e2.
Lees N. The Brandt Line after forty years: The more North-South relations change, the more they stay the same? Rev Int Stud. 2021;47(1):85–106.
Statista: world population by age and region available from: https://www.statista.com/statistics/265759/world-population-by-age-and-region/. Accessed 16 Feb 2024.
Dave M, Rankin J, Pearce M, Foster HE. Global prevalence estimates of three chronic musculoskeletal conditions: club foot, juvenile idiopathic arthritis and juvenile systemic lupus erythematosus. Pediatr Rheumatol. 2020;18(1):1–7.
Aggarwal A, Rajasekhar L, Ghosh P, Mathew A, Kavadichanda C, Shobha V, Gupta R, Tripathy S, Rathi M, Jain A, Lawrence A. Juvenile Onset SLE in India-Data from a Multi-institutional Inception (INSPIRE) Cohort of Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2022;74 (suppl 9). https://acrabstracts.org/abstract/juvenileonset-sle-in-india-data-from-a-multi-institutional-inception-inspire-cohort-of-systemic-lupus-erythematosus/. Accessed 4 Jan 2024.
Chandwar K, Aggarwal A. Systemic lupus erythematosus in children. Indian Journal of Pediatrics. 2023;15:1– 9.
Na Nakorn K, Piyaphanee N, Sukharomana M, Pinpatanapong R, Charuvanij S. Outcomes of achieving lupus low disease activity state and damage accrual in childhood-onset systemic lupus erythematosus. Clin Rheumatol. 2023;42(6):1–10.
Tang SP, Lim SC, Arkachaisri T. Childhood-Onset Systemic Lupus Erythematosus: Southeast Asian Perspectives. J Clin Med. 2021;10(4):559.
Cann MP, Sage AM, McKinnon E, Lee SJ, Tunbridge D, Larkins NG, et al. Childhood Systemic Lupus Erythematosus: Presentation, management and long-term outcomes in an Australian cohort. Lupus. 2022;31(2):246–55.
Aggarwal A, Gupta R, Rajasekhar L, Mathew A, Ghosh P, Kavadichanda C, Shobha V, Das B, Rathi M, Jain A, Lawrence A. Outcome of Pediatric Lupus in South Asia: Data from Indian SLE Inception Cohort for Research (INSPIRE) [abstract]. Arthritis Rheumatol. 2023;75 (suppl 9). https://acrabstracts.org/abstract/outcome-of-pediatriclupus-in-south-asia-data-from-indian-sle-inception-cohort-for-research-inspire/. Accessed 4 Jan 2024.
Chatterjee R, Pattanaik SS, Misra DP, Agarwal V, Lawrence A, Misra R, et al. Tuberculosis remains a leading contributor to morbidity due to serious infections in Indian patients of SLE. Clin Rheumatol. 2023;42(8):1–12.
Tektonidou MG, Lewandowski LB, Hu J, Dasgupta A. Survival in adults and children with systemic lupus erythematosus: a systematic review and Bayesian meta-analysis of studies from 1950 to 2016. Ann Rheum Dis. 2017;76(12):2009–16.
Wang YF, Wei W, Tangtanatakul P, Zheng L, Lei Y, Lin Z, et al. Identification of Shared and Asian-Specific Loci for Systemic Lupus Erythematosus and Evidence for Roles of Type III Interferon Signaling and Lysosomal Function in the Disease: A Multi-Ancestral Genome-Wide Association Study. Arthritis Rheumatol. 2022;74(5):840–8.
Brown GJ, Cañete PF, Wang H, Medhavy A, Bones J, Roco JA, et al. TLR7 gain-of-function genetic variation causes human lupus. Nature. 2022;605(7909):349–56.
Lewis MJ, Jawad AS. The effect of ethnicity and genetic ancestry on the epidemiology, clinical features and outcome of systemic lupus erythematosus. Rheumatol (Oxford). 2017;56(suppl_1):i67–77.
Tiffin N. Unique considerations for advancing genomic medicine in African populations. Pers Med. 2014;11(2):187–96.
Ameh OI, Kengne AP, Jayne D, Bello AK, Hodkinson B, Gcelu A, et al. Standard of treatment and outcomes of adults with lupus nephritis in Africa: a systematic review. Lupus. 2016;25(11):1269–77.
Essouma M, Nkeck JR, Endomba FT, Bigna JJ, Singwe-Ngandeu M, Hachulla E. Systemic lupus erythematosus in Native sub-Saharan Africans: a systematic review and meta-analysis. J Autoimmun. 2020;106:102348.
Dzifa D, Boima V, Yorke E, Yawson A, Ganu V, Mate-Kole C. Predictors and outcome of systemic lupus erythematosus (SLE) admission rates in a large teaching hospital in sub-Saharan Africa. Lupus. 2018;27(2):336–42.
Al-Arbi KMS, Magula NP, Mody GM. Tuberculosis remains a major burden in systemic lupus erythematosus patients in Durban, South Africa. Front Med (Lausanne). 2023;10:1118390.
Harrison MJ, Zuhlke LJ, Lewandowski LB, Scott C. Pediatric systemic lupus erythematosus patients in South Africa have high prevalence and severity of cardiac and vascular manifestations. Pediatr Rheumatol Online J. 2019;17(1):76.
Coovadia H, Hussain A, Mwelase L. Systemic lupus erythematosus in a black South African child. S Afr Med J. 1991;79(1):101–3.
Lewandowski LB, Schanberg LE, Thielman N, Phuti A, Kalla AA, Okpechi I, et al. Severe disease presentation and poor outcomes among pediatric systemic lupus erythematosus patients in South Africa. Lupus. 2017;26(2):186–94.
Lewandowski LB, Watt MH, Schanberg LE, Thielman NM, Scott C. Missed opportunities for timely diagnosis of pediatric lupus in South Africa: a qualitative study. Pediatr Rheumatol Online J. 2017;15(1):14.
Smith EMD, Lewandowski LB, Jorgensen AL, Phuti A, Nourse P, Scott C, et al. Growing international evidence for urinary biomarker panels identifying lupus nephritis in children - verification within the South African Paediatric Lupus Cohort. Lupus. 2018;27(14):2190–9.
Dey D, Katso B, Baah A, Isaaka S, Amoako E. Exploring paediatric rheumatology care: a ten-year retrospective analysis of the patient population in Ghana. Pediatr Rheumatol. 2024;22(1):40.
Ikram N, Lewandowski LB, Watt MH, Scott C. Barriers and facilitators to medical care retention for pediatric systemic lupus erythematosus in South Africa: a qualitative study. Pediatr Rheumatol Online J. 2024;22(1):59.
Migowa A, Bernatsky S, Ngugi A, Foster HE, Muriuki P, Lusambili A, et al. An iceberg I can’t handle: a qualitative inquiry on perceptions towards paediatric rheumatology among healthcare workers in Kenya. Pediatr Rheumatol Online J. 2023;21(1):6.
PAFLAR. PAFLAR: Paediatric African league against rheumatism [Available from: https://paflar.org. Accessed 16 Feb 2024.
Vazzana KM, Musolf AM, Bailey-Wilson JE, Hiraki LT, Silverman ED, Scott C, et al. Transmission disequilibrium analysis of whole genome data in childhood-onset systemic lupus erythematosus. Genes Immun. 2023;24(4):200–6.
Country Meters available from: https://countrymeters.info/pt/South_America. Accessed 4 Jan 2024.
Russo R. SP0101 Pediatric Rheumatology in South America. Ann Rheum Dis. 2013;72(Suppl 3):A23–4.
Sakamoto AP, Silva CA, Pita AC, Trindade VC, Islabao AG, Fiorot FJ, et al. Risk factors for mortality in 1528 Brazilian childhood-onset systemic lupus erythematosus patients. Lupus. 2023;32(6):781–90.
Sakamoto AP, Silva CA, Islabão AG, Novak GV, Molinari B, Nogueira PK, et al. Chronic kidney disease in patients with childhood-onset systemic lupus erythematosus. Pediatric Nephrol (Berlin, Germany). 2023;38(6):1843–54.
Miguel DF, Terreri MT, Pereira RMR, Bonfá E, Silva CAA, Corrente JE, et al. Comparison of urinary parameters, biomarkers, and outcome of childhood systemic lupus erythematosus early onset-lupus nephritis. Adv Rheumatol. 2020;60(1):10.
Frittoli RB, Pereira DR, Lapa AT, Postal M, Sinicato NA, Fernandes PT, et al. Axonal dysfunction is associated with interferon-γ levels in childhood-onset systemic lupus erythematosus: a multivoxel magnetic resonance spectroscopy study. Rheumatology. 2021;61(4):1529–37.
Sinicato NA, de Oliveira L, Lapa A, Postal M, Peliçari KO, Costallat LT, et al. Familial aggregation of childhood-and adulthood-onset systemic lupus erythematosus. Arthritis Care Res. 2020;72(8):1147–51.
Smith EMD, Tharmaratnam K, Al-Abadi E, Armon K, Bailey K, Brennan M, et al. Attainment of Low Disease Activity and Remission Targets reduces the risk of severe flare and new damage in Childhood Lupus. Rheumatology (Oxford). 2021;61(8):3378–89.
Smith EMD, Gorst SL, Al-Abadi E, Hawley DP, Leone V, Pilkington C, et al. “It is good to have a target in mind”: Qualitative views of patients and parents informing a treat to target clinical trial in JSLE. Rheumatology (Oxford). 2021;60(12):5630–41.
Wahadat MJ, van den Berg L, Timmermans D, van Rijswijk K, van Dijk-Hummelman A, Bakx S, et al. LLDAS is an attainable treat-to-target goal in childhood-onset SLE. Lupus Sci Med. 2021;8(1):e000571.
Ozturk K, Caglayan S, Tanatar A, Baglan E, Yener Otar G, Kavrul Kayaalp G, et al. Low disease activity state in juvenile-onset systemic lupus erythematosus. Lupus. 2021;30(13):2144–50.
Elliott RS, Taylor E, Ainsworth J, Preston J, Smith E. Improving communication of the concept of “treat-to target” in childhood lupus: a public and patient (PPI) engagement project involving children and young people. BMC Rheumatol. 2022;6(1):69.
Smith EMD, Egbivwie N, Cowan K, Ramanan AV, Pain CE. Research priority setting for paediatric rheumatology in the UK. Lancet Rheumatol. 2022;4(7):e517–24.
van Vollenhoven RF, Mosca M, Bertsias G, Isenberg D, Kuhn A, Lerstrom K, et al. Treat-to-target in systemic lupus erythematosus: recommendations from an international task force. Ann Rheum Dis. 2014;73(6):958–67.
Franklyn K, Lau CS, Navarra SV, Louthrenoo W, Lateef A, Hamijoyo L, et al. Definition and initial validation of a Lupus Low Disease Activity State (LLDAS). Ann Rheum Dis. 2016;75(9):1615–21.
Petri M, Magder LS. Comparison of Remission and Lupus Low Disease Activity State in Damage Prevention in a United States Systemic Lupus Erythematosus Cohort. Arthritis Rheumatol. 2018;70(11):1790–5.
Piga M, Floris A, Cappellazzo G, Chessa E, Congia M, Mathieu A, et al. Failure to achieve lupus low disease activity state (LLDAS) six months after diagnosis is associated with early damage accrual in Caucasian patients with systemic lupus erythematosus. Arthritis Res Ther. 2017;19(1):247.
Tani C, Vagelli R, Stagnaro C, Carli L, Mosca M. Remission and low disease activity in systemic lupus erythematosus: an achievable goal even with fewer steroids? Real-life data from a monocentric cohort. Lupus Sci Med. 2018;5(1):e000234.
Tsang-A-Sjoe MWP, Bultink IEM, Heslinga M, Voskuyl AE. Both prolonged remission and Lupus Low Disease Activity State are associated with reduced damage accrual in systemic lupus erythematosus. Rheumatology (Oxford). 2016;56(1):121–8.
Zen M, Iaccarino L, Gatto M, Saccon F, Larosa M, Ghirardello A, et al. Lupus low disease activity state is associated with a decrease in damage progression in Caucasian patients with SLE, but overlaps with remission. Ann Rheum Dis. 2018;77(1):104–10.
Fanouriakis A, Adamichou C, Koutsoviti S, Panopoulos S, Staveri C, Klagou A, et al. Low disease activity-irrespective of serologic status at baseline-associated with reduction of corticosteroid dose and number of flares in patients with systemic lupus erythematosus treated with belimumab: A real-life observational study. Semin Arthritis Rheum. 2018;48(3):467–74.
Ugarte-Gil MF, Pons-Estel GJ, Vila LM, McGwin G, Alarcón GS. Time in remission and low disease activity state (LDAS) are associated with a better quality of life in patients with systemic lupus erythematosus: results from LUMINA (LXXIX), a multiethnic, multicentre US cohort. RMD Open. 2019;5(1):e000955.
Yeo AL, Koelmeyer R, Kandane-Rathnayake R, Golder V, Hoi A, Huq M, et al. Lupus Low Disease Activity State and Reduced Direct Health Care Costs in Patients With Systemic Lupus Erythematosus. Arthritis Care Res (Hoboken). 2020;72(9):1289–95.
Smith EMD, Aggarwal A, Ainsworth J, Al-Abadi E, Avcin T, Bortey L, et al. Towards development of Treat to Target (T2T) in Childhood-onset Systemic Lupus Erythematosus: PReS-endorsed Overarching Principles and Points-to-Consider from an International Task Force. Annal Rheum Dis. 2022;82(6):788–98.
Smith EMD, Aggarwal A, Ainsworth J, Al-Abadi E, Avcin T, Bortey L, et al. PReS-endorsed international childhood lupus T2T task force definition of childhood lupus low disease activity state (cLLDAS). Clin Immunol. 2023;250:109296.
Connelly K, Golder V, Kandane-Rathnayake R, Morand EF. Clinician-reported outcome measures in lupus trials: a problem worth solving. Lancet Rheumatol. 2021;3(8):e595–603.
Connelly K, Eades LE, Koelmeyer R, Ayton D, Golder V, Kandane-Rathnayake R, et al. Towards a novel clinical outcome assessment for systemic lupus erythematosus: first outcomes of an international taskforce. Nat Rev Rheumatol. 2023;19(9):592–602.
Gallagher KL, Patel P, Beresford MW, Smith EMD. What Have We Learnt About the Treatment of Juvenile-Onset Systemic Lupus Erythematous Since Development of the SHARE Recommendations 2012? Front Pediatr. 2022;10:884634.
Smith EMD, Lythgoe H, Hedrich CM. Current views on lupus in children. Curr Opin Rheumatol. 2023;35(2):68–81.
Anais N, Anne Perrine F, Lorna G, Christine L, Eric H, Brigitte B-M, et al. Assessment of type I interferon response in routine practice in France in 2022. RMD Open. 2023;9(2):e003211.
Charras A, Haldenby S, Smith EMD, Egbivwie N, Olohan L, Kenny JG, et al. Panel sequencing links rare, likely damaging gene variants with distinct clinical phenotypes and outcomes in juvenile-onset SLE. Rheumatology. 2023;62(SI2):SI210–25.
Boussard C, Delage L, Gajardo T, Kauskot A, Batignes M, Goudin N, et al. DOCK11 deficiency in patients with X-linked actinopathy and autoimmunity. Blood. 2023;141(22):2713–26.
Moreews M, Mathieu A-L, Pouxvielh K, Reuschlé Q, Drouillard A, Dessay P, et al. mTOR Activation Underlies Enhanced B Cell Proliferation and Autoimmunity in PrkcdG510S/G510S Mice. J Immunol. 2023;210(9):1209–21.
Roderick MR, Jefferson L, Renton W, Belot A. Compound Heterozygous Mutations in PRKCD Associated with Early-Onset Lupus and Severe and Invasive Infections in Siblings. J Clin Immunol. 2023;43(4):703–5.
Wahadat MJ, van Tilburg SJ, Mueller YM, de Wit H, Van Helden-Meeuwsen CG, Langerak AW, et al. Targeted multiomics in childhood-onset SLE reveal distinct biological phenotypes associated with disease activity: results from an explorative study. Lupus Sci Med. 2023;10(1):e000799.
Belot A, Rice GI, Omarjee SO, Rouchon Q, Smith EMD, Moreews M, et al. Contribution of rare and predicted pathogenic gene variants to childhood-onset lupus: a large, genetic panel analysis of British and French cohorts. Lancet Rheumatol. 2020;2(2):e99–109.
Ardoin SP, Daly RP, Merzoug L, Tse K, Ardalan K, Arkin L, et al. Research priorities in childhood-onset lupus: results of a multidisciplinary prioritization exercise. Pediatr Rheumatol. 2019;17(1):32.
Vazzana KM, Daga A, Goilav B, Ogbu EA, Okamura DM, Park C, et al. Principles of pediatric lupus nephritis in a prospective contemporary multi-center cohort. Lupus. 2021;30(10):1660–70.
Smitherman EA, Chahine RA, Beukelman T, Lewandowski LB, Rahman AKMF, Wenderfer SE, et al. Childhood-Onset Lupus Nephritis in the Childhood Arthritis and Rheumatology Research Alliance Registry: Short-Term Kidney Status and Variation in Care. Arthritis Care Res. 2023;75(7):1553–62.
Guerra A AH, Garro R, McCracken C, Rouster-Stevens K, Prahalad S. Predictors for early readmission in patients hospitalized with new onset pediatric lupus nephritis. Lupus. 2021;30(12):1991–7.
Rubinstein TB, Davis AM, Rodriguez M, Knight AM. Addressing mental health in pediatric rheumatology. Curr Treat Options Rheumatol. 2018;4:55–72.
Donnelly C, Cunningham N, Jones JT, Ji L, Brunner HI, Kashikar-Zuck S. Fatigue and depression predict reduced health-related quality of life in childhood-onset lupus. Lupus. 2018;27(1):124–33.
Kammeyer R, Ogbu EA, Cooper JC, Stolz E, Piquet AL, Fuhlbrigge RC, Bennett JL, Hutaff-Lee C. Cognitive dysfunction in pediatric systemic lupus erythematosus: current knowledge and future directions. Child Neuropsychol. 2024;30(5):818–846. https://doi.org/10.1080/09297049.2023.2273573.
Chang JC, Xiao R, Meyers KE, Mercer-Rosa L, Natarajan SS, Weiss PF, et al. Nocturnal blood pressure dipping as a marker of endothelial function and subclinical atherosclerosis in pediatric-onset systemic lupus erythematosus. Arthritis Res Ther. 2020;22(1):129.
Chang JC, Xiao R, Knight AM, Kimmel SE, Mercer-Rosa LM, Weiss PF. A population-based study of risk factors for heart failure in pediatric and adult-onset systemic lupus erythematosus. Semin Arthritis Rheum. 2020;50(4):527–33.
Vara E, Gilbert M, Ruth NM. Health disparities in outcomes of pediatric systemic lupus erythematosus. Front Pediatric. 2022;10:897208.
Woo JMP, Simmonds F, Dennos A, Son MBF, Lewandowski LB, Rubinstein TB. Health Equity Implications of Missing Data Among Youths With Childhood-Onset Systemic Lupus Erythematosus: A Proof-of-Concept Study in the Childhood Arthritis and Rheumatology Research Alliance Registry. Arthritis Care Res. 2023;75(11):2285–94.
Sadun RE, Schanberg LE. Transition and transfer of the patient with paediatric-onset lupus: a practical approach for paediatric and adult rheumatology practices. Lupus Sci Med. 2018;5(1):e000282.
Chang JC, Knight AM, Lawson EF. Patterns of Health Care Utilization and Medication Adherence Among Youth with Systemic Lupus Erythematosus During Transfer from Pediatric to Adult Care. J Rheumatol. 2020;48(1):105–13.
Haro SL, Lawson EF, Hersh AO. Disease activity and health-care utilization among young adults with childhood-onset lupus transitioning to adult care: data from the Pediatric Lupus Outcomes Study. Lupus. 2020;29(10):1206–15.
Webber D, Cao J, Dominguez D, Gladman DD, Levy DM, Ng L, et al. Association of systemic lupus erythematosus (SLE) genetic susceptibility loci with lupus nephritis in childhood-onset and adult-onset SLE. Rheumatology (Oxford). 2020;59(1):90–8.
Dominguez D, Kamphuis S, Beyene J, Wither J, Harley JB, Blanco I, et al. Relationship Between Genetic Risk and Age of Diagnosis in Systemic Lupus Erythematosus. J Rheumatol. 2021;48(6):852–8.
Misztal MC, Liao F, Couse M, Cao J, Dominguez D, Lau L, et al. Genome-Wide Sequencing Identified Rare Genetic Variants for Childhood-Onset Monogenic Lupus. J Rheumatol. 2022;50(5):671–5.
Cannon LA, Wenderfer SE, Lewandowski LB, Cooper JC, Goilav B, Knight AM, et al. Use of EuroLupus Cyclophosphamide Dosing for the Treatment of Lupus Nephritis in Childhood-onset Systemic Lupus Erythematosus in North America. J Rheumatol. 2022;49(6):607–14.
Wang CS, Sadun RE, Zhou W, Miller KR, Pyle L, Ardoin SP, et al. Renal Response Outcomes of the EuroLupus and National Institutes of Health Cyclophosphamide Dosing Regimens in Childhood-Onset Proliferative Lupus Nephritis. Arthritis Rheumatol. 2024;76(3):469–78.
Roberts JE, Burn C, Sadun RE, Smitherman EA, Wenderfer SE, Son MBF. Real-world use and outcomes of belimumab in childhood-onset lupus: A single-center retrospective study. Lupus. 2023;32(9):1111–6.
Mougiakakos D, Krönke G, Völkl S, Kretschmann S, Aigner M, Kharboutli S, et al. CD19-targeted CAR T cells in refractory systemic lupus erythematosus. N Engl J Med. 2021;385(6):567–9.
Mackensen A, Müller F, Mougiakakos D, Böltz S, Wilhelm A, Aigner M, et al. Anti-CD19 CAR T cell therapy for refractory systemic lupus erythematosus. Nat Med. 2022;28(10):2124–32.
Correll CK, Ditmyer MM, Mehta J, Imundo LF, Klein-Gitelman MS, Monrad SU, et al. 2015 American College of Rheumatology workforce study and demand projections of pediatric rheumatology workforce, 2015–2030. Arthritis Care Res. 2022;74(3):340–8.
Lewandowski LB. Tackling global challenges in pediatric rheumatology. Curr Opin Rheumatol. 2020;32(5):414–20.
Migowa AN, Hadef D, Hamdi W, Mwizerwa O, Ngandeu M, Taha Y, et al. Pediatric rheumatology in Africa: thriving amidst challenges. Pediatr Rheumatol Online J. 2021;19(1):69.
Scott C, Sawhney S, Lewandowski LB. Pediatric Rheumatic Disease in Lower to Middle-Income Countries: Impact of Global Disparities, Ancestral Diversity, and the Path Forward. Rheumatic Dis Clin North Am. 2022;48(1):199–215.
Briggs AM, Jordan JE, Sharma S, Young JJ, Chua J, Foster HE, et al. Context and priorities for health systems strengthening for pain and disability in low-and middle-income countries: a secondary qualitative study and content analysis of health policies. Health Policy Plan. 2023;38(2):129–49.
Smith N, Foster HE, Jandial S. A mixed methods evaluation of the Paediatric Musculoskeletal Matters (PMM) online portfolio. Pediatric Rheumatology. 2021 9;19(1):85. https://doi.org/10.1186/s12969-021-00567-5.
Lewandowski LB, Watt MH, Schanberg LE, Thielman NM, Scott CJPR. Missed opportunities for timely diagnosis of pediatric lupus in South Africa: a qualitative study. Pediatric Rheumatol. 2017;15(1):14.
Foster HE, Scott C. Update the WHO EML to improve global paediatric rheumatology. Nat Rev Rheumatol. 2020;16(3):123.
Furia FF, Godfrey E, Mwamanenge N, Swai P. Spectrum of paediatric rheumatic disorders at a tertiary hospital in Tanzania. Pediatr Rheumatol Online J. 2020;18(1):30.
Tangcheewinsirikul S, Tang SP, Smith N, Sukharomana M, Charuvanij S, Vilaiyuk S, et al. Delivery of paediatric rheumatology care: a survey of current clinical practice in Southeast Asia and Asia-Pacific regions. Pediatr Rheumatol Online J. 2021;19(1):11.
Al Maini M, Al Weshahi Y, Foster HE, Chehade MJ, Gabriel SE, Al Saleh J, et al. A global perspective on the challenges and opportunities in learning about rheumatic and musculoskeletal diseases in undergraduate medical education. Clin Rheumatol. 2020;39(3):627–42.
Bilsborrow JB, Peláez-Ballestas I, Pons-Estel B, Scott C, Tian X, Alarcon GS, et al. Global Rheumatology Research: Frontiers, Challenges, and Opportunities. Arthritis Rheumatol (Hoboken, NJ). 2022;74(1):1–4.
Mahfud M, Jones M, Fader T, Hause E. A virtual pediatric rheumatology teaching initiative for physicians in Somaliland. Pediatr Rheumatol. 2023;21(1):1.
Lewandowski LB, Schiffenbauer A, Mican JM, Moses SJ, Fallah MP, Plotz P, et al. Rheumatology capacity building: implementing a rheumatology curriculum for Liberian health-care providers in 2016. Clin Rheumatol. 2020;39(3):689–96.
Migowa A, Bernatsky S, Ngugi AK, Foster HE, Muriuki P, Riang’a RM, et al. Bridging gaps: a qualitative inquiry on improving paediatric rheumatology care among healthcare workers in Kenya. Pediatr Rheumatol Online J. 2023;21(1):144.
Scott C, Chan M, Slamang W, Okong’o L, Petty R, Laxer RM, et al. Juvenile arthritis management in less resourced countries (JAMLess): consensus recommendations from the cradle of humankind. Clin Rheumatol. 2019;38(2):563–75.
Khubchandani R, Avčin T, Ravelli A. Towards telehealth delivery in pediatric rheumatology practice. Pediatr Rheumatol. 2023;21(1):145.
Al-Arbi KMS, Magula NP, Mody GM. Tuberculosis remains a major burden in systemic lupus erythematosus patients in Durban. South Afr Front Med. 2023;10:1118390.
Sadun R, Lewandowski L, Belot A, Smith E, Cooper J. Development of core and expanded datasets to align registries and advance international collaborative research for childhood-onset systemic lupus erythematosus [abstract]. Arthritis Rheumatol. 2022;74 (suppl 9). https://acrabstracts.org/abstract/juvenile-onset-sle-in-india-data-from-a-multi-institutional-inception-inspire-cohort-of-systemic-lupus-erythematosus/. Accessed 16 Feb 2024.
Olusanya JO, Ubogu OI, Njokanma FO, Olusanya BO. Transforming global health through equity-driven funding. Nat Med. 2021;27(7):1136–8.
Acknowledgements
The authors thank all individuals with childhood-onset SLE around the world for your valuable contribution to all the research reviewed here. We also thank Bradley Otterson, National Institutes of Health Library, for manuscript review and editing. Figures were created with Biorender.com.
Funding
Open access funding provided by the National Institutes of Health Dr. Lewandowski is funded by the NIAMS Intramural Research Program. Dr Kate Webb receives funding for research from the South African Medical Research Council (SA-MRC) with funds received from the National Treasury. The content and findings reported/illustrated are the sole deduction, view and responsibility of the researcher and do not reflect the official position and sentiments of the SAMRC or National Treasury.
Author information
Authors and Affiliations
Contributions
All authors (AA, TAPF, AM, ES, MH, KW, LBL) were involved in study concept and design, drafting the article, and revising it critically for important intellectual content. LBL created the figures. All authors read and approved the final version to be submitted for publication.
Corresponding author
Ethics declarations
Human and Animal Rights, Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Aggarwal, A., Fernandes, T.A.P., Migowa, A. et al. Childhood-Onset Systemic Lupus Erythematosus (cSLE): An International Perspective. Curr Allergy Asthma Rep 24, 559–569 (2024). https://doi.org/10.1007/s11882-024-01169-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11882-024-01169-3