Abstract
Purpose of Review
This review investigates occupational inhalation hazards associated with biologically derived airborne particles (bioaerosols) generated in indoor cannabis cultivation and manufacturing facilities.
Recent Findings
Indoor cannabis production is growing across the US as are recent reports of respiratory diseases among cannabis workers, including occupational asthma morbidity and mortality. More information is needed to understand how bioaerosol exposure in cannabis facilities impacts worker health and occupational disease risk.
Summary
Preliminary studies demonstrate a significant fraction of airborne particles in cannabis facilities are comprised of fungal spores, bacteria, and plant material, which may also contain hazardous microbial metabolites and allergens. These bioaerosols may pose pathogenic, allergenic, toxigenic, and pro-inflammatory risks to workers. The absence of multi-level, holistic bioaerosol research in cannabis work environments necessitates further characterization of the potential respiratory hazards and effective risk prevention methods to safeguard occupational health as the cannabis industry continues to expand across the US and beyond.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the cannabis and hemp industries expand across the United States and globally, an increasing number of workers are exposed to respiratory hazards associated with the cultivation and manufacturing of Cannabis sativa products. Despite state legalization, the US federal government designates high tetrahydrocannabinol (THC)-containing cannabis as a Schedule I Drug. Therefore, there is no federal oversight of cannabis production by either the United States Department of Agriculture (USDA) or the Food and Drug Administration (FDA). Without these federal crop- and consumer-protection mechanisms, cannabis can be cultivated and processed in environments with potentially increased airborne biological hazards—including but not limited to viable plant and human pathogens, microbial metabolites, toxins, and allergenic proteins—posing health risks to workers, consumers, and plants alike.
Nevertheless, the cannabis market continues to expand in response to state legalization measures. Recently, the Centers for Disease Control (CDC) called for comprehensive measures to protect cannabis workers from inhalation hazards in response to a fatal asthma attack suffered by a worker processing cannabis flower [1]. Undoubtedly, there are large gaps in the scientific basis for providing occupational safety recommendations associated with the potential inhalation hazards unique to indoor cannabis cultivation and manufacturing, as little research has been performed to holistically characterize respiratory risk factors or develop effective prevention measures to control these hazards.
Indeed, it is challenging to parse out meaningful information from the limited body of literature on this topic, as many of the respiratory hazard evaluations in cannabis operations have been performed by state or federal governments in the weeks or months after employee complaints or adverse worker events. Moreover, some reports acknowledge that air sampling was limited as operations were not in full production or that evaluation of air quality was performed after new equipment was installed, such as post-hoc implementation of high-efficiency particulate air (HEPA) filtration [1, 2]. To add more complexity, cannabis work-associated respiratory diseases are likely underreported. This may be due to lack of awareness and training on Occupational Safety and Health Administration (OSHA) protections or due to other cannabis worker concerns about being associated with an industry that is not federally legal. Indeed, a cannabis worker who suffered a fatal asthma attack experienced several respiratory symptoms in the months leading up to their death, including a medical emergency room visit for work-related dyspnea. Moreover, four other co-workers on the associated cannabis flower production team also complained of work-related symptoms, including dyspnea, nasal congestion, and hives. These incidents were not reported until an OSHA investigation surveyed these employees after their co-worker’s death [1]. Holistic investigation of cannabis occupational inhalation hazards is lacking, which in turn prevents this growing industry from better protecting its workers.
In this context, the bioaerosols in cannabis operations are defined as airborne particulate matter comprised in whole or in part of primary biological materials directly associated with all aspects of cannabis operations; these airborne constituents are known to impact worker health in parallel agricultural and manufacturing industries as well as many common indoor environments [3,4,5,6,7,8,9,10,11,12,13]. Bioaerosols remain poorly characterized in the cannabis industry, despite increasing reports of cannabis work-related respiratory diseases linked to bioaerosol exposure [1, 14, 15]. The complexity of bioaerosols, combined with the federal status of state-sanctioned cannabis operations, adds additional barriers for traditional academic research and funding to further investigate cannabis workplace hazards.
In response, this review presents the most current research describing bioaerosols associated with cannabis work environments, outlining the diversity, distribution, and abundance of these airborne constituents, as well as the potential respiratory hazards they pose to workers. We draw from relevant research in indoor and occupational environments, allergy and asthma, and aerobiology of the built environment to investigate respiratory diseases observed in cannabis workers that have potential causal links to related bioaerosol exposures. Where relevant, we will compare bioaerosol exposures observed in parallel industries and environments where indoor air quality (IAQ) and occupational exposure limit (OEL) information is available to provide frame of precedence on the bioaerosol types and exposure levels associated with occupational respiratory diseases.
Cannabis Cultivation and Bioaerosol Generation
The C. sativa plant is divided into two categories based on the abundance of the intoxicating compound THC. This cannabinoid is found within the inflorescence, also known as the flower, of the female plant. Hemp is defined as containing lower levels of THC content by dry weight (< 0.3% THC by weight), while cannabis, often referred to as marijuana, contains higher levels of THC (> 0.3% THC by weight). As such, cannabis is designated as a Schedule I Drug by the Controlled Substances Act and is federally illegal, despite many states legalizing cannabis for medical and recreational use [16, 17].
In addition to differences in cannabinoid content, hemp and cannabis are cultivated and processed to produce distinct end products. Hemp is grown in industrial agricultural settings for its fiber, seed oil, and its non-intoxicating cannabidiol (CBD) content. In contrast, cannabis is grown on a smaller horticultural scale, most often in indoor controlled environment agriculture (CEA) settings to produce flower products and extracts with significantly higher THC content. As such, there is a large diversity of building types and environmental conditions that contain cannabis growing, processing, formulation, and packaging operations [16, 17].
The indoor cannabis CEA environment is optimized for plant growth and flower production, often by regulating temperature, relative humidity (RH), carbon dioxide (CO2) levels, and light exposure. Following harvest of mature female plants, cannabis flower is dried and cured to remove excess moisture, followed by processing steps that include milling, trimming, pre-roll manufacturing, and/or extraction of flower materials into cannabinoid-containing oils [16, 17]. Each of these cultivation and manufacturing processes involve different steps that may expose workers to unique respiratory hazards, including exposure to airborne particulate matter (PM).
Airborne PM, comprised either in part or in whole of primary biological materials, makes up a significant portion of PM in the respirable size range (< 10 µm; PM10) in both indoor and outdoor settings. Respirable PM is of high concern as it can pass through the nasal passages and deposit into the airways and lungs. Fine PM, smaller than 2.5 µm (PM2.5), may directly absorb into the bloodstream from the lung and is linked to several respiratory and systemic diseases, including negative cardiovascular and neurodegenerative effects [18,19,20]. In addition to differences in respiratory deposition, the indoor settling time also differs depending on the size of these airborne particles. Larger PM settles within seconds to minutes, while finer PM2.5 settles in time frames of hours or days, persisting in the work environment. Respiratory exposures are assessed as a combination of the indoor pollutant concentration and the exposure time; thus, respirable bioaerosols may also result in more significant respiratory exposures [21,22,23,24].
A common bioaerosol assessment method is to count intact organisms, enumerating fungal spores, pollen granules, culturable colony forming units (CFU), or infectious viral particles within a known volume of air. Modern aerobiology practices can also analyze air samples via DNA- or RNA-based sequencing to identify and estimate the relative abundance of different fungal, bacterial, and viral constituents in the air. Other bioaerosol constituents like microbial metabolites (endotoxin, ergosterol, (1➔3)-β-D-glucan, peptidoglycan, and mycotoxins) and protein allergens are sometimes measured as they are also linked to less well understood mechanisms that contribute to chronic, non-infectious diseases and allergenic respiratory diseases [3,4,5,6, 9,10,11, 21,22,23,24,25,26,27,28].
Bioaerosols are challenging to characterize. While there are strong associations between respiratory exposure to dampness, mold, and organic dusts, direct causation and dose–response data are often lacking. This is partly due to methodological limitations in exposure assessments and to the diverse categories of inhalable biological constituents described above. Bioaerosols also vary temporally and spatially and can have complex interactions with other PM, gasses, humidity, and light in the atmospheric environment [21,22,23,24]. Despite these challenges, it is essential to understand bioaerosol size, composition, and abundance, as airborne pathogenic microbes, microbial metabolites, and protein allergens are inhalation hazards associated with a variety of acute and chronic diseases in agricultural and indoor settings that share many aspects with cannabis operations [3,4,5,6,7,8,9,10,11,12,13].
Bioaerosol Exposure Association with Respiratory Diseases of Cannabis Workers
Unique bioaerosols are present at each stage of the indoor cannabis cultivation and manufacturing process, and exposure may result in neutral, potentially positive, or negative health effects. These bioaerosols likely rapidly cycle in space and time and differ by source generation and operational activity. Indeed, it is likely that the plants and harvested plant matter generate and host much of the bioaerosols associated with indoor cannabis operations; however, there are many other sources as well, including but not limited to the growing substrate, amendments, beneficial organisms, irrigation water and its delivery system, surfaces, floors, ceilings, walls, the HVAC system (both ventilation and humidity controllers), and the workers themselves (Fig. 1).
Bioaerosols in cannabis indoor work environments. The cultivation, post-harvest dry/cure, processing, pre-roll manufacturing, and packaging operations all generate unique bioaerosols that vary in composition and size, as well as vary within the operational activity and over time. These airborne biological materials may be harmful, neutral, or potentially beneficial to worker health. Sources for these bioaerosols include cannabis plant matter, microorganisms associated with the plant, building materials, substrates, and post-harvest spoilage, irrigation water and its delivery system, growing substrate and amendments, surfaces, floors, ceilings, walls, HVAC system (ventilation and humidity controllers), and the workers themselves
Causal relationships between bioaerosol exposure and respiratory diseases are difficult to establish. When considering the etiological origins of environmental and occupational lung disease, an important component of disease progression is aberrant immune activation and/or inflammation that is not efficiently resolved, ultimately progressing to tissue injury and/or remodeling that yields the classic hallmarks of diseases such as asthma, chronic obstructive pulmonary disease (COPD), hypersensitivity pneumonitis, and various interstitial lung diseases. As highlighted throughout this review, PM composition is an important determinant to respiratory disease (as well as systemic disease) etiology. For example, inorganic PM (such as black carbon or silica) exposure is often associated with interstitial lung disease pathologies (pneumoconioses) [29, 30], while bioaerosols composed of organic dust PM are commonly associated with allergic, asthmatic, and/or other inflammatory pathologies [10, 11].
At a mechanistic level, the diverse constituents of bioaerosols, including microbial pathogens and their metabolites, as well as allergenic proteins, can drive both inflammation and hypersensitivity responses in exposed individuals. For example, many occupational asthma cases have a clear Type I Hypersensitivity (Immunoglobulin E (IgE)-mediated) response to an allergen in the environment, although some cases are driven by chronic inflammation (without an allergenic component) that leads to bronchoconstriction and tissue remodeling [31,32,33]. As another example, hypersensitivity pneumonitis is a common interstitial lung disease identified in individuals exposed to certain organic dusts; this immune-mediated process is classically driven by Type III and Type IV Hypersensitivity responses to antigens of bacteria, molds, animals, or low molecular weight chemical compounds [34]. Overall, it is recognized that repeated or chronic exposure to organic dust-derived bioaerosols increases the likelihood for long-term negative respiratory consequences.
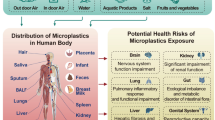
Indeed, bioaerosols linked to disease can contain complex combinations of various inflammatory or otherwise allergenic components that share many similarities with preliminary bioaerosol investigations in cannabis cultivation and manufacturing environments, where bioaerosols have been shown to impact worker safety, plant health, and even regulatory compliance of cannabis flower products [1, 14, 15, 35,36,37,38,39,40,41,42]. Characterization of the airborne PM components in hemp and cannabis workspaces has demonstrated potential for significant levels of bioaerosols, composed of bacteria, fungi, and actinomycetes, as well as high levels of airborne plant matter, protein, and endotoxins—all of which have been associated with a range of health hazards [2, 43,44,45,46,47,48]. Based on the growing body of research on cannabis- and hemp-related bioaerosols, we categorize bioaerosols that pose inhalation hazards to cannabis workers here as the following: 1) microbial pathogens, 2) toxigenic or pro-inflammatory microbial metabolites, and 3) protein allergens; each of these categories are associated with diverse exposure effects and respiratory diseases (Fig. 2).
Exposure to complex bioaerosol constituents relevant to cannabis workplaces may contribute to diverse respiratory and systemic effects. Cannabis cultivation and manufacturing facilities harbor airborne bacteria, fungi, plant matter, and other bioaerosol constituents. Airborne pathogens may be inhaled and could result in infection, particularly in susceptible individuals. Other bioaerosol constituents like microbial metabolites and protein allergens are associated with non-infectious and allergenic respiratory diseases. The complex nature of bioaerosols, challenges assessing worker exposure, lack of diagnostic and research tools, and the Schedule I status of cannabis all contribute to the limited data available to directly connect cannabis-relevant bioaerosol exposure to respiratory disease in workers. Therefore, clear causal relationships between bioaerosol exposure and respiratory effects are not fully elucidated
Bioaerosols and their Constituents in Cannabis Work Environments
Microbial Pathogens
The C. sativa microbiome includes many microorganisms, the majority of which are not pathogenic to plants or people; however, there are several toxigenic, allergenic, and/or pathogenic microbial species that have been identified on cannabis plants and flower products [49, 50]. Therefore, these organisms and their metabolites are likely present in cannabis cultivation and manufacturing environments. Studies investigating airborne microorganisms in hemp and cannabis facilities have identified many types of potentially harmful bacterial and fungal microorganisms, including but not limited to Actinobacteria, Pseudomonas aeruginosa, Staphylococcus, Escherichia coli, Enterobacter, Enterococcus, Botrytis, Aspergillus, Penicillium, Cladosporium, Alternaria alternata, Trichoderma viride, Wallemia, Mucor, Rhizopus, Candida albicans, and Stachybotrys chartarum [2, 43,44,45,46,47,48].
One report estimated levels of airborne mold spores in cannabis facilities at > 500,000 spores/m3. When air samples were processed to enumerate airborne CFU, many samples overloaded culture plates, and culturable airborne microorganisms could not be quantified (highest reported as > 11,300 CFU/m3). These authors cautioned that elevated mold spore levels warranted respirator use in these environments [43]. Genetic identification of fungal species within cannabis cultivation air samples also showed elevated and enriched mold species typically associated with water-damaged homes [44, 45]. Notably, airborne levels of culturable bacteria and fungi regularly exceeded 1,000,000 CFU/m3 within a hemp facility, and workers were provided with respirators for their protection [2]. Although there is evidence that waste collection workers exposed to environmental pathogens are at risk for infectious diseases [51], it is poorly understood how exposure to bioaerosols found in cannabis facilities may cause infection in cannabis workers. Indeed, there is no established OSHA OEL for airborne spores or bacterial/fungal CFU despite the World Health Organization (WHO) categorizing “high” levels of airborne culturable fungal species as ≥ 1,000 CFU/m3 [52]. Of note, this WHO categorization is not uniformly accepted in many regulatory circles, and lower levels have been suggested for airborne pathogens and thermophilic actinomycetes as they may be harmful at lower abundance [52,53,54].
Elevated airborne fungi and bacteria levels in these environments could also contribute to non-pathogenic and allergenic pulmonary diseases within cannabis workers due to respiratory exposures to associated airborne microbial breakdown products, metabolites, and/or allergens, as discussed below [3,4,5,6,7,8,9,10,11,12,13].
Microbial Metabolites
Endotoxin, also called lipopolysaccharide (LPS), is a macromolecule composed of a lipid and polysaccharide that is found within the Gram-negative bacterial outer membrane. In addition to its functional attributes in bacteria, it can be a potent endotoxin that activates the mammalian immune system and causes inflammation, fever, and septic shock; moreover, endotoxin is an established inhalation hazard linked to inflammatory lung diseases [3, 9,10,11, 25, 55, 56]. Airborne endotoxin levels are measured as endotoxin units normalized by air volume (EU/m3); however, there is no established OSHA OEL for airborne endotoxin. Recently, the Dutch Expert Committee on Occupational Safety (DECOS) proposed an OEL of ≤ 90 EU/m3 over an eight-hour weighed average work period, which is used for reference here [57].
There are limited reports measuring airborne endotoxin in hemp and cannabis operations, but they show that endotoxin levels range widely depending on the operational activity and the manufacturing environment. The highest levels of airborne endotoxin in two hemp processing studies were 1,600 EU/m3 and 59,801 EU/m3, suggesting hemp workers can be exposed to extremely high endotoxin levels [2, 58]. Reports in cannabis operations have generally observed airborne endotoxin below the DECOS exposure limit; however, in two cases endotoxin levels were elevated to 85 or 94 EU/m3 during grinding of dried cannabis flower [1, 45, 46, 59].
Importantly, exposure to airborne endotoxin levels below the DECOS limit has been associated with respiratory symptoms and a decline in lung function [56]. This is also acknowledged in the CDC report investigating a fatal cannabis occupational asthma attack, as the authors state, “Airborne respirable dust and endotoxin levels below occupational exposure limits do not exclude a sufficient level of airborne allergen to trigger asthma and other allergic symptoms” [1].
Although airborne endotoxin is a classic industrial hygiene measure, there are a multitude of other airborne microbial metabolites, breakdown products, and associated bioactive agents that may contribute to pulmonary disease following respiratory exposure, several of which are known to contribute to inflammation independent of endotoxin levels [8, 9]. Like bacterial endotoxin, ergosterol is a cell membrane component, and it is important for regulating fungal membrane fluidity. Inhalation exposure to this fungal immunologically active lipid is associated with asthma, and within mammalian cells it can induce pyroptosis, a type of necrotic and inflammatory programmed cell death [8, 25, 60, 61].
Peptidoglycan acts as the backbone of bacterial cell walls. Both Gram-negative and -positive bacteria contain this structural element, but it is present at much higher levels in the latter, and thus is utilized as a surrogate measure of Gram-positive bacteria within dust and air samples. These molecules are recognized by the mammalian innate immune system, inducing a pro-inflammatory response linked to lung inflammation, specifically in response to inhaling organic dusts [9, 62, 63].
The structural element (1➔3)-β-D-glucan is a component of fungal cell walls that is also present in some bacteria and plants. Mammalian phagocytosing cell receptors bind (1➔3)-β-D-glucan molecules, and these fungal molecules elicit pro-inflammatory and cytotoxic responses by disrupting cell cycle signaling, inducing cell death, and causing oxidative stress in vitro. Although broader epidemiological studies are lacking, the presence of (1➔3)-β-D-glucan within occupant air has been associated with airway inflammation and asthma symptoms [26, 27, 64].
Fungal organisms can produce hundreds of mycotoxins, which are low molecular weight molecules that act as virulence factors and defense chemicals. These mycotoxins can cause adverse health effects in humans by inhibiting essential cellular processes, resulting in immunotoxicity, organ-specific toxicity, and cancer [65, 66]. Indeed, parallel agricultural, animal husbandry, and indoor environments have demonstrated that airborne mycotoxins contribute to respiratory diseases as well as “sick building syndrome” [4, 66,67,68]. Many molds associated with cannabis production have the capacity to produce multiple mycotoxins, including Alternaria, Aspergillus, Penicillium, Stachybotrys, Wallemia, and Fusarium species [36, 43,44,45, 66, 69].
To the authors’ current knowledge, there are no published studies investigating the abundance of airborne ergosterol, peptidoglycan, (1➔3)-β-D-glucan, or mycotoxins within cannabis work environments or their connection to cannabis worker respiratory disease.
Protein Allergens
Allergens are most commonly protein macromolecules that activate the mammalian adaptive immune system, initiating a Type I Hypersensitivity (IgE-mediated) response. This IgE response is considered a “classic allergic” response that differs from other pro-inflammatory responses activated by other microbial metabolites described above. Airborne allergen exposure usually causes mild inflammation of the eyes, nose, inner ear, throat, and airways, but these aeroallergens can also have significant health impacts, triggering asthma attacks and even causing anaphylaxis [22, 28, 70].
Because of its complexity, direct aeroallergen monitoring is not commonly performed, and allergen abundance is often indirectly evaluated through surrogates, such as measuring dust levels, culturing airborne bacteria and fungi, microscopic spore counts, or by DNA analysis for target organisms known to produce allergens. Moreover, many bioaerosol collection methods can denature the proteins they are meant to assess; thus, appropriate collection methods must be used to preserve allergen protein structure to allow for accurate immunoassay quantification [22, 28, 70].
To date, data directly identifying and measuring aeroallergens in cannabis facilities are lacking. However, there have been several documented cannabis work-related asthma cases where exposure to airborne mold or plant materials have been contributing factors [1, 14, 15]. Cannabis and hemp work environments can present relatively high levels of airborne protein, organic dusts, molds, and plant matter, suggesting that aeroallergens may be found within these bioaerosols [2, 43,44,45,46,47]. In similar agriculture and CEA environments, allergens and allergenic responses are linked to a diversity of other worksite sources, including spider mite pests, predatory mites, paper pots, and growing substrates like coco coir and rockwool [6, 71,72,73].
Of the fungi associated with cannabis and cannabis facility air, several are known to produce allergenic proteins, including Aspergillus, Penicillium, Cladosporium, Alternaria, Rhizopus, and Fusarium species [36, 43,44,45, 69, 74]. The opportunistic pathogen Aspergillus fumigatus was recently designated by WHO as a Critical Priority Fungal Pathogen and is known to produce several mycotoxins; furthermore, A. fumigatus also produces at least 30 known allergens listed on the WHO/IUIS (International Union of Immunological Societies) Allergen Nomenclature Database (http://www.allergen.org) [74,75,76]. This mold species exemplifies the diverse bioaerosol constituents that a single organism can produce, which may cause a wide variety of respiratory exposure responses. In wood milling operations, A. fumigatus allergens can be found in wood and wood-derived dust, presenting potential respiratory hazards to workers [77]. Indeed, some allergens are secreted by germinating A. fumigatus mycelium and are found associated with spores, so they are likely present on A. fumigatus-laden cannabis flower, on growing substrates, and/or building materials in cannabis manufacturing environments, potentially posing an inhalation risk to workers if aerosolized [78].
Studies of some hemp operations found a high prevalence of respiratory symptoms among workers exposed to respirable organic dust, where levels ranged from 10–80 mg/m3 [2, 48, 58]. According to OSHA’s Table Z-1-Limits for Air Contaminants, permissible exposure limits to cotton or grain dusts should not exceed levels 1 or 10 mg/m3, respectively, over an eight-hour work shift [79], whereas DECOS has recommended a limit of 1.5 mg/m3 of inhalable grain dust [80]. These dusts may contain a variety of microorganisms, their metabolites, and protein allergens, including cannabis allergens.
Like many plants, C. sativa also produces allergenic proteins, and sensitization to crude cannabis extracts and specific cannabis proteins has been documented in cannabis workers, cannabis consumers, and cannabis laboratory personnel [15, 38,39,40,41,42, 81,82,83,84]. In cannabis production environments, the handling and processing of cannabis materials during cultivation and manufacturing likely exposes workers to cannabis allergens, especially during milling and pre-roll manufacturing where aerosolization of dried plant materials often occurs. Indeed, one study found that C. sativa DNA sequences made up to 80% of bioaerosol sequencing reads in cannabis worker personal air samples, suggesting plant matter itself composes a large portion of bioaerosols in these environments [45].
Five C. sativa allergens are currently listed in the WHO/IUIS Allergen Nomenclature Database: Can s 2, Can s 3, Can s 4, Can s 5, and Can s 7 [76]. Several of these allergens have been covered thoroughly in recent reviews discussing their characteristics, homology to other known plant allergens, and their connection to allergic responses, specifically in cannabis workers [40,41,42]. Despite the link between cannabis allergen exposure and worker allergic responses, there are limited clinical diagnostic tests to understand cannabis protein mediators of IgE-specific sensitization. Crude cannabis extracts are often used in skin prick tests to determine cannabis-specific allergic sensitization; however, these cannabis extracts are not strictly reproducible, can be difficult to procure in many states, and positive results do not identify the causal allergen(s) involved in IgE-mediated responses. There are Can s 3-based diagnostic tests that detect specific anti-Can s 3 IgE antibodies or patient basophil activation following exposure to purified Can s 3; however, to date, there are no clinically available tests that investigate sensitization to the other four identified cannabis allergens [42, 85].
It is important to emphasize that despite the high levels of plant material suspended in the air of cannabis and hemp facilities, there is no peer-reviewed literature thus far identifying or quantifying airborne cannabis allergens within cannabis workspaces. Moreover, foundational knowledge on cannabis allergens is limited, with little understanding on the tissue-specific expression or chemotype/strain-dependent abundance of cannabis allergens. A recent proteomics investigation of cannabis and hemp flower protein extracts identified 49 potential allergens present across the four different chemotypes tested, including known C. sativa allergens Can s 2, Can s 3, and Can s 5; yet Can s 4 was absent in all protein extracts [86]. Indeed, there are large gaps in the basic research of cannabis allergenic proteins, likely due to the limited availability of commercial antibody-based allergen detection methods capable of quantifying these allergens and due to the federal limitations that impede cannabis research under Schedule I classification.
Overall, more diagnostic tool development and associated exposure research is desperately needed to investigate the aeroallergens present within cannabis cultivation and manufacturing environments and connect the presence of these unique aeroallergens to respiratory diseases observed in workers.
Bioaerosol Synergies
Although we simplify bioaerosols into three categories in Fig. 2, many types of bioaerosols occur simultaneously in the air and several are known to act synergistically to elicit negative health outcomes; therefore, in-depth, multi-level analysis of the diversity of bioaerosols within cannabis environments is needed to understand the multifaced nature of respiratory exposure and associated disease potential. For example, the mycotoxin deoxynivalenol (DON) is produced by the cannabis pathogen Fusarium, and it sensitizes mice to protein allergens [36, 64, 87], suggesting it may exacerbate responses to mold or cannabis allergens. Endotoxin can also potentiate the effects of DON, increasing susceptibility of animals and humans to bacterial infections by altering immune responses and enhancing one another’s toxicity [88]. Moreover, general PM exposure in combination with mycotoxins, (1➔3)-β-D-glucan, or allergens can act synergistically to enhance cytotoxicity and inflammation [64, 89, 90]. Thus, it is essential to understand the diverse inhalable risk constituents by developing and implementing meaningful, holistic exposure assessments to better understand the links between diverse, dynamic exposures and disease.
Management and Prevention
Cannabis industry manufacturers and regulatory bodies should take simple, prophylactic actions to protect workers from potential respiratory hazards, despite the lack of scientific literature on this topic. There are established hierarchy of controls for similar occupational settings to proactively address respiratory hazards [91]. Engineering controls should be implemented to reduce bioaerosol generation and exposure, drawing from effective mitigation strategies that manage other damp, indoor environments [52]. Building materials and substrates should be updated to prevent growth of harmful microorganisms, their metabolites, and allergens. Best practices should be adopted, including appropriate HVAC implementation and enhanced air filtration to control bioaerosols in CEA environments [92].
In a parallel study, worker exposure to airborne fungi, (1➔3)-β-D-glucan, bacteria, endotoxin, and dust in vegetable greenhouses was higher when handling dried plant materials versus freshly harvested material [93]. This demonstrates how simple aerosol management measures, including HEPA air filtration, should be a top priority in cannabis cultivation, processing, pre-roll manufacturing, and packaging to reduce overall bioaerosol levels, with a specific focus on post-harvest handling and processing of dried plant materials. Cost-effective air quality monitoring tools are available that measure PM10 and PM2.5, allowing real-time evaluation of respirable PM and verification of the effectiveness of these control measures. Personal protective equipment (PPE) and respiratory protection programs may be required if other steps within the hierarchy of controls do not effectively control these hazards. Worker education and training programs should also be standardized to inform workers about the bioaerosol exposure risks in cannabis work environments, how to report any adverse health effects, and how to best protect themselves. Expansion and more consistent implementation of these programs is needed across the US.
Conclusions
Bioaerosol research in cannabis cultivation and manufacturing is in its early stages, but the connection between bioaerosol exposure and worker respiratory diseases is concerning. There is a large gap in the scientific literature characterizing bioaerosols that may pose inhalation hazards to cannabis workers–no comprehensive or unified approach yet exists. There is a great need to understand airborne microorganisms in these environments, as well as their aerosolized pro-inflammatory and toxic metabolites, including but not limited to the prevalence of airborne endotoxin, ergosterol, (1➔3)-β-D-glucan, peptidoglycan, and mycotoxins. Aeroallergens produced within the cannabis cultivation and manufacturing environments are also poorly understood, specifically those allergens produced by the C. sativa plant itself.
Unfortunately, the proposed re-scheduling of cannabis to a Schedule III Drug [94] will not likely alleviate the research restrictions on studying non-federally recognized, but state-sanctioned, cannabis operations and products, especially if research samples may contain THC. Federal regulatory barriers must be removed from this “gray area” between federal and state legalities, and specific funding could be made available for researchers to identify and quantify the types of bioaerosols present in cannabis occupational settings, assess worker exposure levels, and investigate the link between exposure and respiratory diseases. Only after the scientific community establishes foundational knowledge of the multi-level and diverse bioaerosol constituents in these environments, can evidence-based exposure levels be leveraged to develop meaningful occupational exposure guidelines.
Overall, a proactive, multi-level research approach investigating the abundance and diversity of bioaerosols in cannabis work environments is critical to understand and control the health risks to workers. By taking these steps, we can use evidence-based methods to better protect cannabis workers from the harmful effects of bioaerosol exposures and help ensure a safe and healthy work environment for this expanding industry.
Data Availability
No datasets were generated or analysed during the current study.
References
Weaver VM, Hua JT, Fitzsimmons KM, Laing JR, Farah W, Hart A, et al. Occupational Asthma in Cannabis Production - Massachusetts. MMWR Morb Mortal Wkly Rep. 2023;17:1257–61. https://doi.org/10.15585/mmwr.mm7246a2. (This paper discusses the serious implications of occupational asthma in the cannabis production industry, highlighting a fatal case, and emphasizing the need for improved diagnostic tools, monitoring, and preventive measures).
Fishwick D, Allan LJ, Wright A, Curran AD. Assessment of Exposure to Organic Dust in a Hemp Processing Plant. Ann Occup Hyg. 2001;45:577–83. https://doi.org/10.1093/annhyg/45.7.577.
Liebers V, Brüning T, Raulf M. Occupational endotoxin exposure and health effects. Arch Toxicol. 2020;94:3629–44. https://doi.org/10.1007/s00204-020-02905-0.
Niculita-Hirzel H, Hantier G, Storti F, Plateel G, Roger T. Frequent occupational exposure to Fusarium mycotoxins of workers in the Swiss grain industry. Toxins (Basel). 2016;8:370. https://doi.org/10.3390/toxins8120370.
Fischer G, Dott W. Relevance of airborne fungi and their secondary metabolites for environmental, occupational and indoor hygiene. Arch Microbiol. 2003;179:75–82. https://doi.org/10.1007/s00203-002-0495-2.
Madsen AM, Crook B. Occupational exposure to fungi on recyclable paper pots and growing media and associated health effects – A review of the literature. Sci Total Environ. 2021;788. https://doi.org/10.1016/j.scitotenv.2021.147832.
Douwes J, Thorne P, Pearce N, Heederik D. Bioaerosol health effects and exposure assessment: Progress and prospects. Ann Occup Hyg. 2003;47:187–200. https://doi.org/10.1093/annhyg/meg032.
Mendell MJ, Mirer AG, Cheung K, Tong M, Douwes J. Respiratory and allergic health effects of dampness, mold, and dampness-related agents: A review of the epidemiologic evidence. Environ Health Perspect. 2011;119:748–56. https://doi.org/10.1289/ehp.1002410.
Poole JA, Dooley GP, Saito R, Burrell AM, Bailey KL, Romberger DJ, et al. Muramic acid, endotoxin, 3-hydroxy fatty acids, and ergosterol content explain monocyte and epithelial cell inflammatory responses to agricultural dusts. J Toxicol Environ Health A. 2010;73:684–700. https://doi.org/10.1080/15287390903578539.
Nordgren TM, Bailey KL. Pulmonary health effects of agriculture. Curr Opin Pulm Med. 2016;22:144–9. https://doi.org/10.1097/mcp.0000000000000247.
Nordgren TM, Charavaryamath C. Agriculture Occupational Exposures and Factors Affecting Health Effects. Curr Allergy Asthma Rep. 2018;18. https://doi.org/10.1007/s11882-018-0820-8.
Plombon S, Henneberger PK, Humann MJ, Liang X, Doney BC, Kelly KM, et al. The association of chronic bronchitis and airflow obstruction with lifetime and current farm activities in a sample of rural adults in Iowa. Int Arch Occup Environ Health. 2022;95:1741–54. https://doi.org/10.1007/s00420-022-01866-4.
Von Essen S, Fryzek J, Nowakowski B, Wampler M. Respiratory symptoms and farming practices in farmers associated with an acute febrile illness after organic dust exposure. Chest. 1999;116:1452–8. https://doi.org/10.1378/chest.116.5.1452.
Reeb-Whitaker C, LaSee CR, Bonauto DK. Surveillance of work-related asthma including the emergence of a cannabis-associated case series in Washington State. J Asthma. 2022;59:1537–47. https://doi.org/10.1080/02770903.2021.1955379. (This article discusses work-related asthma in Washington State, highlighting the emergence of cannabis-associated asthma cases. It identifies the most affected industries and substances leading to work-related asthma, with a focus on the cannabis industry post-legalization. It emphasizes the importance of state-based surveillance in detecting occupational diseases and informing prevention strategies.)
Sack C, Ghodsian N, Jansen K, Silvey B, Simpson CD. Allergic and respiratory symptoms in employees of indoor cannabis grow facilities. Ann Work Expo Health. 2020;64:754–64. https://doi.org/10.1093/annweh/wxaa050. (This study investigates health symptoms among cannabis employees in Washington State, illustrating a high prevalence of cannabis work-related allergic and respiratory issues. It highlights the potential occupational hazards of cannabis production environments, such as exposure to dust and allergens, which may lead to negative health effects like work-related asthma.)
Caulkins JP, Kilborn ML. Cannabis legalization, regulation, & control: a review of key challenges for local, state, and provincial officials. Am J Drug Alcohol Abuse. 2019;45:689–97. https://doi.org/10.1080/00952990.2019.1611840.
Visković J, Zheljazkov VD, Sikora V, Noller J, Latković D, Ocamb CM, et al. Industrial Hemp (Cannabis sativa L.) Agronomy and Utilization: A Review. Agronomy. 2023;13:931. https://doi.org/10.3390/agronomy13030931.
Zhang B, Weuve J, Langa KM, D’Souza J, Szpiro A, Faul J, et al. Comparison of Particulate Air Pollution from Different Emission Sources and Incident Dementia in the US. JAMA Intern Med. 2023;183:1080–9. https://doi.org/10.1001/jamainternmed.2023.3300. (This article examines the association between long-term exposure to fine particulate matter (PM2.5) from various emission sources and the incidence of dementia in older adults in the US. It finds that higher levels of PM2.5, including organic sources from agriculture, are linked to increased rates of dementia.)
Bhatnagar A. Cardiovascular Effects of Particulate Air Pollution. Annu Rev Med. 2022;73:393–406. https://doi.org/10.1146/annurev-med-042220-011549.
You R, Ho YS, Chang RCC. The pathogenic effects of particulate matter on neurodegeneration: a review. J Biomed Sci. 2022;29:15. https://doi.org/10.1186/s12929-022-00799-x.
Liu Y, Ma H, Zhang N, Li Q. A systematic literature review on indoor PM2.5 concentrations and personal exposure in urban residential buildings. Heliyon. 2022;8:10174. https://doi.org/10.1016/j.heliyon.2022.e10174.
Raulf M, Buters J, Chapman M, Cecchi L, De Blay F, Doekes G, et al. Monitoring of occupational and environmental aeroallergens--EAACI Position Paper. Concerted action of the EAACI IG occupational allergy and aerobiology & air pollution. Allergy. 2014;69:1280–99. https://doi.org/10.1111/all.12456.
Shen F, Yao M. Bioaerosol nexus of air quality, climate system and human health. Nat Sci Open. 2023;2:20220050. https://doi.org/10.1360/nso/20220050. (The article discusses the significant impact of bioaerosols on human health, air quality, and climate systems, with a specific focus on microorganisms and their fragments suspended in the air. It emphasizes the need for future interdisciplinary studies to better understand the chemical and biological processes of airborne microorganisms as well as their role in disease transmission and non-communicable diseases.)
Gilbert JA, Stephens B. Microbiology of the built environment. Nat Rev Microbiol. 2018;16:661–70. https://doi.org/10.1038/s41579-018-0065-5.
Davidson ME, Schaeffer J, Clark ML, Magzamen S, Brooks EJ, Keefe TJ, et al. Personal exposure of dairy workers to dust, endotoxin, muramic acid, ergosterol, and ammonia on large-scale dairies in the high plains western United States. J Occup Environ Hyg. 2018;15:182–93. https://doi.org/10.1080/15459624.2017.1403610.
Rylander R, Lin R-H. (1–>3)-β-D-glucan-relationship to indoor air-related symptoms, allergy and asthma. Toxicology. 2000;152:47–52. https://doi.org/10.1016/s0300-483x(00)00291-2.
Douwes J. (1–>3)-β-D-glucans and respiratory health: A review of the scientific evidence. Indoor Air. 2005;15:160–9. https://doi.org/10.1111/j.1600-0668.2005.00333.x.
Levetin E, McLoud JD, Pityn P, Rorie AC. Air Sampling and Analysis of Aeroallergens: Current and Future Approaches. Curr Allergy Asthma Rep. 2023;23:223–36. https://doi.org/10.1007/s11882-023-01073-2.
Vanka KS, Shukla S, Gomez HM, James C, Palanisami T, Williams K, et al. Understanding the pathogenesis of occupational coal and silica dust-associated lung disease. Eur Respir Rev. 2022;31:210250. https://doi.org/10.1183/16000617.0250-2021.
Schenker MB. Inorganic agricultural dust exposure causes pneumoconiosis among farmworkers. Proc Am Thorac Soc. 2010;7:107–10. https://doi.org/10.1513/pats.200906-036rm.
Romanet-Manent S, Charpin D, Magnan A, Lanteaume A, Vervloet D. Allergic vs nonallergic asthma: What makes the difference? Allergy. 2002;57:607–13. https://doi.org/10.1034/j.1398-9995.2002.23504.x.
Hammad H, Lambrecht BN. The basic immunology of asthma. Cell. 2021;184:1469–85. https://doi.org/10.1016/j.cell.2021.02.016.
Lummus ZL, Wisnewski AV, Bernstein DI. Pathogenesis and Disease Mechanisms of Occupational Asthma. Immunol Allergy Clin North Am. 2011;31:699–716. https://doi.org/10.1016/j.iac.2011.07.008.
Alberti ML, Rincon-Alvarez E, Buendia-Roldan I, Selman M. Hypersensitivity Pneumonitis: Diagnostic and Therapeutic Challenges. Front Med (Lausanne). 2021;8:718299. https://doi.org/10.3389/fmed.2021.718299.
Punja ZK, Ni L, Lung S, Buirs L. Total yeast and mold levels in high THC-containing cannabis (Cannabis sativa L.) inflorescences are influenced by genotype, environment, and pre-and post-harvest handling practices. Front Microbiol. 2023;14:1192035. https://doi.org/10.3389/fmicb.2023.1192035.
Gwinn KD, Leung MCK, Stephens AB, Punja ZK. Fungal and mycotoxin contaminants in cannabis and hemp flowers: implications for consumer health and directions for further research. Front Microbiol. 2023;14:1278189. https://doi.org/10.3389/fmicb.2023.1278189. (This paper reviews the fungal microbiome of cannabis and hemp flower, focusing on pathogenic and toxigenic fungi that pose potential health risks to consumers. It discusses gaps in current regulations that fail to assess many of these potential hazards, and it highlights approaches to reduce fungal contaminants on cannabis plants and flower by proactively addressing these risks within the cultivation and post-harvest manufacturing processes to improve product quality and protect consumer health.)
Punja ZK, Collyer D, Scott C, Lung S, Holmes J, Sutton D. Pathogens and Molds Affecting Production and Quality of Cannabis sativa L. Front Plant Sci. 2019;10:1120. https://doi.org/10.3389/fpls.2019.01120.
Chatkin JM, Zani-Silva L, Ferreira I, Zamel N. Cannabis-Associated Asthma and Allergies. Clin Rev Allergy Immunol. 2019;56:196–206. https://doi.org/10.1007/s12016-017-8644-1.
Sussman GL, Beezhold DH, Cohn JR, Silvers WS, Zeiger JS, Nayak AP. Cannabis: An emerging occupational allergen? Ann Work Expo Health. 2020;64:679–82. https://doi.org/10.1093/annweh/wxaa043.
Decuyper II, Green BJ, Sussman GL, Ebo DG, Silvers WS, Pacheco K, et al. Occupational Allergies to Cannabis. J Allergy Clin Immunol Pract. 2020;8:3331–8. https://doi.org/10.1016/j.jaip.2020.09.003. (This article targets a physician audience, discussing the rise of occupational allergies related to cannabis, and highlighting the potential for allergic sensitization among workers in the cannabis industry due to direct handling of plant matter.)
Toscano A, Ebo DG, Abbas K, Brucker H, Decuyper II, Naimi D, et al. A review of cannabis allergy in the early days of legalization. Ann Allergy Asthma Immunol. 2023;130:288–95. https://doi.org/10.1016/j.anai.2022.10.016. (This review broadly outlines cannabis allergy and underscores its increasing incidence linked to cannabis legalization. It highlights clinical features of cannabis allergy, including immediate-type hypersensitivity and potential cross-reactivities, and emphasizes the challenges in diagnosing cannabis allergy due to limited tools and legal restrictions.)
Skypala IJ, Jeimy S, Brucker H, Nayak AP, Decuyper II, Bernstein JA, et al. Cannabis-related allergies: An international overview and consensus recommendations. Allergy. 2022;77:2038–52. https://doi.org/10.1111/all.15237. (The article provides an international overview of cannabis-related allergies, presenting consensus recommendations from various experts in the field. It discusses the clinical implications of cannabis occupational exposure and cannabis use, associations between cannabis allergy and food allergy, and provides an overview of diagnostic methods like skin prick tests and specific IgE antibody tests. The article calls for efforts to standardize allergy testing and management for cannabis allergens, which challenging due to limited diagnostic tools and the illegal status of cannabis in many countries.)
Martyny JW, Serrano KA, Schaeffer JW, Van Dyke MV. Potential exposures associated with indoor marijuana growing operations. J Occup Environ Hyg. 2013;10:622–39. https://doi.org/10.1080/15459624.2013.831986.
Root KS, Magzamen S, Sharp JL, Reynolds SJ, Van Dyke M, Schaeffer JW. Application of the environmental relative moldiness index in indoor marijuana grow operations. Ann Work Expo Health. 2020;64:728–44. https://doi.org/10.1093/annweh/wxaa071.
Couch JR, Grimes GR, Wiegand DM, Green BJ, Glassford EK, Zwack LM, et al. Potential occupational and respiratory hazards in a Minnesota cannabis cultivation and processing facility. Am J Ind Med. 2019;62:874–82. https://doi.org/10.1002/ajim.23025.
Victory KR, Couch J, Lowe B, Green BJ. Occupational Hazards associated with Harvesting and Processing Cannabis-Washington, 2015–2016. MMWR Morb Mortal Wkly Rep. 2018;67:259–60. https://doi.org/10.15585/mmwr.mm6708a7.
Green BJ, Couch JR, Lemons AR, Burton NC, Victory KR, Nayak AP, et al. Microbial hazards during harvesting and processing at an outdoor United States cannabis farm. J Occup Environ Hyg. 2018;15:430–40. https://doi.org/10.1080/15459624.2018.1432863.
Zuskin E, Kanceljak B, Pokrajac D, Schachter EN, Witek TJ. Respiratory symptoms and lung function in hemp workers. Br J Ind Med. 1990;47:627–32. https://doi.org/10.1136/oem.47.9.627.
Taghinasab M, Jabaji S. Cannabis microbiome and the role of endophytes in modulating the production of secondary metabolites: An overview. Microorganisms. 2020;8:355. https://doi.org/10.3390/microorganisms8030355.
Vujanovic V, Korber DR, Vujanovic S, Vujanovic J, Jabaji S. Scientific prospects for cannabis-microbiome research to ensure quality and safety of products. Microorganisms. 2020;8:290. https://doi.org/10.3390/microorganisms8020290.
Madsen AM, Frederiksen MW, Jacobsen MH, Tendal K. Towards a risk evaluation of workers’ exposure to handborne and airborne microbial species as exemplified with waste collection workers. Environ Res. 2020;183:109177. https://doi.org/10.1016/j.envres.2020.109177.
World Health Organization. WHO Guidelines for Indoor Air Quality: Dampness and Mould. 2009. Accessed 5/27/2024 from: https://www.who.int/publications/i/item/9789289041683 .
National Institute for Occupational Safety and Health. NIOSH Manual of Analytical Methods (NMAM), Fifth Edition. 2020. Accessed 5/27/2024 from: https://www.cdc.gov/niosh/nmam .
Kim KH, Kabir E, Jahan SA. Airborne bioaerosols and their impact on human health. J Environ Sci (China). 2018;67:23–35. https://doi.org/10.1016/j.jes.2017.08.027.
Chhetry B, Dewangan K, Mahato D, Kumar P. Endotoxins Affecting Human Health during Agricultural Practices: An Overview. AppliedChem. 2022;3:11–31. https://doi.org/10.3390/appliedchem3010002.
Farokhi A, Heederik D, Smit LAM. Respiratory health effects of exposure to low levels of airborne endotoxin - A systematic review. Environ Health. 2018;17:14. https://doi.org/10.1186/s12940-018-0360-7.
Health Council of the Netherlands. Endotoxins. Health-based recommended occupational exposure Limit. 2010. Accessed 5/27/2024 from: https://www.healthcouncil.nl/documents/advisory-reports/2010/07/15/endotoxins-health-based-recommended-occupational-exposure-limit .
Er M, Emri SA, Demir AU, Thorne PS, Karakoca Y, Bilir N, et al. Byssinosis and COPD rates among factory workers manufacturing hemp and jute. Int J Occup Med Environ Health. 2016;29:55–68. https://doi.org/10.13075/ijomeh.1896.00512.
NIOSH. Evaluation of a Medicinal Cannabis Manufacturing Facility with an Indoor and Outdoor Grow Operation. Cincinnati, OH. 2018. Accessed 5/27/2024 from: https://www.cdc.gov/niosh/hhe/reports/pdfs/2016-0090-3317.pdf .
Rodrigues ML. The Multifunctional Fungal Ergosterol mBio. 2018;9:e01755-e1818. https://doi.org/10.1128/mbio.01755-18.
Koselny K, Mutlu N, Minard AY, Kumar A, Krysan DJ, Wellington MA. Genome-Wide Screen of Deletion Mutants in the Filamentous Saccharomyces cerevisiae Background Identifies Ergosterol as a Direct Trigger of Macrophage Pyroptosis. mBio. 2018;9:e01204-18. https://doi.org/10.1128/mbio.01204-18.
Wolf AJ, Underhill DM. Peptidoglycan recognition by the innate immune system. Nat Rev Immunol. 2018;18:243–54. https://doi.org/10.1038/nri.2017.136.
Nordgren TM, Bailey KL, Heires AJ, Katafiasz D, Romberger DJ. Effects of Agricultural Organic Dusts on Human Lung-Resident Mesenchymal Stem (Stromal) Cell Function. Toxicol Sci. 2018;162:635–44. https://doi.org/10.1093/toxsci/kfx286.
Turner J, McCabe K, Snawder J, Hernandez M. (1–>3) β-Glucan induces multimodal toxicity responses in parallel exposures of model human lung epithelial cells and immature macrophage. Air Qual Atmos Health. 2019;12:379–87. https://doi.org/10.1007/s11869-018-0649-2.
Throckmorton K, Wiemann P, Keller NP. Evolution of chemical diversity in a group of non-reduced polyketide gene clusters: Using phylogenetics to inform the search for novel fungal natural products. Toxins (Basel). 2015;7:3572–607. https://doi.org/10.3390/toxins7093572.
Miller JD, McMullin DR. Fungal secondary metabolites as harmful indoor air contaminants: 10 years on. Appl Microbiol Biotechnol. 2014;98:9953–66. https://doi.org/10.1007/s00253-014-6178-5.
Marcelloni AM, Pigini D, Chiominto A, Gioffrè A, Paba E. Exposure to airborne mycotoxins: the riskiest working environments and tasks. Ann Work Expo Health. 2024;68:19–35. https://doi.org/10.1093/annweh/wxad070.
Straus DC. Molds, mycotoxins, and sick building syndrome. Toxicol Ind Health. 2009;25:617–35. https://doi.org/10.1177/0748233709348287.
Gwinn KD, Hansen Z, Kelly H, Ownley BH. Diseases of Cannabis sativa Caused by Diverse Fusarium Species. Front Agron. 2022;3. https://doi.org/10.3389/fagro.2021.796062.
Dramburg S, Hilger C, Santos AF, de las Vecillas L, Aalberse RC, Acevedo N, et al. EAACI Molecular Allergology User’s Guide 2.0. Pediatr Allergy Immunol. 2023;34:e13854. https://doi.org/10.1111/pai.13854.
Groenewoud G, de Graaf In T, Veld C, Van Oorschot-van Nes A, de Jong N, Vermeulen A, van Toorenenbergen AW, et al. Prevalence of sensitization to the predatory mite Amblyseius cucumeris as a new occupational allergen in horticulture. Allergy. 2002;57:614–9. https://doi.org/10.1034/j.1398-9995.2002.203511.x.
Zhou Y, Jia H, Zhou X, Cui Y, Qian J. Epidemiology of spider mite sensitivity: a meta-analysis and systematic review. Clin Transl Allergy. 2018;8:21. https://doi.org/10.1186/s13601-018-0209-8.
Panicker V, Chetambath R. Nasobronchial allergy and pulmonary function abnormalities among coir workers of Alappuzha. J Assoc Physicians India. 2010;58:420–2 Accessed 5/27/2024 from: https://www.researchgate.net/publication/49648530_Nasobronchial_allergy_and_pulmonary_function_abnormalities_among_coir_workers_of_Alappuzha .
Pomés A, Davies JM, Gadermaier G, Hilger C, Holzhauser T, Lidholm J, et al. WHO/IUIS Allergen Nomenclature: Providing a common language. Mol Immunol. 2018;100:3–13. https://doi.org/10.1016/j.molimm.2018.03.003.
World Health Organization. WHO fungal priority pathogens list to guide research, development and public health action. 2022. Accessed 5/27/2024 from: https://www.who.int/publications/i/item/9789240060241 .
World Health Organization. International Union of Immunological Societies. WHO/IUIS Allergen Nomenclature Sub-Committee. 2018. Accessed 5/27/2024 from: https://allergen.org/ .
Prester L, Macan J. Levels of the fungal allergen Asp f 1 in dust from two sawmills in Croatia: A pilot study. Aerobiologia. 2014;30:189–96. https://doi.org/10.1007/s10453-013-9317-z.
Chapman MD. Challenges associated with indoor moulds: Health effects, immune response and exposure assessment. Med Mycol. 2006;44:29–32. https://doi.org/10.1080/13693780600835740.
Occupational Safety and Health Administration. OSHA 29 CFR 1910.1000 Table Z-1 Permissible Exposure Limits for Air Contaminants. 1993. Accessed 5/27/2024 from: https://www.osha.gov/annotated-pels/table-z-1 .
Health Council of the Netherlands. Grain dust: Health-based recommended occupational exposure limit. 2011. Accessed 5/27/2024 from: https://www.healthcouncil.nl/binaries/healthcouncil/documenten/advisory-reports/2011/07/22/grain-dust-health-based-recommended-occupational-exposure-limit/advisory-report-grain-dust-health-based-recommended-occupational-exposure-limit.pdf .
Jackson B, Cleto E, Jeimy S, Jeimy S. An emerging allergen: Cannabis sativa allergy in a climate of recent legalization. Allergy Asthma Clin Immunol. 2020;16:53. https://doi.org/10.1186/s13223-020-00447-9.
Ocampo TL, Rans TS. Cannabis sativa: The unconventional “weed” allergen. Ann Allergy Asthma Immunol. 2015;114:187–92. https://doi.org/10.1016/j.anai.2015.01.004.
Herzinger T, Schöpf P, Przybilla B, Ruëff F. IgE-mediated hypersensitivity reactions to cannabis in laboratory personnel. Int Arch Allergy Immunol. 2011;156:423–6. https://doi.org/10.1159/000324444.
Nayak AP, Green BJ, Sussman G, Berlin N, Lata H, Chandra S, et al. Characterization of Cannabis sativa allergens. Ann Allergy Asthma Immunol. 2013;111:32–7. https://doi.org/10.1016/j.anai.2013.04.018.
Decuyper II, Van Gasse AL, Faber MA, Elst J, Mertens C, Rihs HP, et al. Exploring the Diagnosis and Profile of Cannabis Allergy. J Allergy Clin Immunol Pract. 2019;7:983-989.e5. https://doi.org/10.1016/j.jaip.2018.09.017.
Loblundo C, Severa J, Peruggia GA, Black KR, Chandra S, Lata H, et al. Proteomics-Based Approach for Detailing the Allergenic Profile of Cannabis Chemotypes. Int J Mol Sci. 2023;24:13964. https://doi.org/10.3390/ijms241813964.
Bol-Schoenmakers M, Braber S, Akbari P, De Graaff P, Van Roest M, Kruijssen L, et al. The mycotoxin deoxynivalenol facilitates allergic sensitization to whey in mice. Mucosal Immunol. 2016;9:1477–86. https://doi.org/10.1038/mi.2016.13.
Bonnet MS, Roux J, Mounien L, Dallaporta M, Troadec JD. Advances in deoxynivalenol toxicity mechanisms: The brain as a target. Toxins (Basel). 2012;4:1120–38. https://doi.org/10.3390/toxins4111120.
Capasso L, Longhin E, Caloni F, Camatini M, Gualtieri M. Synergistic inflammatory effect of PM10 with mycotoxin deoxynivalenol on human lung epithelial cells. Toxicon. 2015;104:65–72. https://doi.org/10.1016/j.toxicon.2015.08.008.
Lam HCY, Jarvis D, Fuertes E. Interactive effects of allergens and air pollution on respiratory health: A systematic review. Sci Total Environ. 2021;757:143924. https://doi.org/10.1016/j.scitotenv.2020.143924.
Occupational Safety and Health Administration. OSHA Recommended Practices for Safety and Health Programs. 2016. Accessed 5/27/2024 from: https://www.osha.gov/safety-management .
Resource Innovation Institute. Best Practices Guide HVAC for Controlled Environment Agriculture (CEA) Operations. 2022. Accessed 5/27/2024 from: https://catalog.resourceinnovation.org/item/controlled-environment-agriculture-hvac-practices-guide-462480 .
Madsen AM, Tendal K, Frederiksen MW. Attempts to reduce exposure to fungi, β-glucan, bacteria, endotoxin and dust in vegetable greenhouses and a packaging unit. Sci Total Environ. 2014;468–469:1112–21. https://doi.org/10.1016/j.scitotenv.2013.09.014.
Drug Enforcement Agency. Schedules of Controlled Substances: Rescheduling of Marijuana Docket No. DEA-1362; A.G. Order No. 5931–2024. 2024.
Ethics declarations
Conflict of Interest
Drs. Eidem, Nordgren, and Hernandez have nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Eidem, T., Nordgren, T. & Hernandez, M. Bioaerosol Exposures and Respiratory Diseases in Cannabis Workers. Curr Allergy Asthma Rep (2024). https://doi.org/10.1007/s11882-024-01157-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s11882-024-01157-7