Opinion statement
Isolated limb perfusion (ILP) with chemotherapy alone has uniformly failed in the treatment of irresectable extremity soft tissue sarcomas. The addition of tumor necrosis factor-alpha (TNF-α) to this treatment approach contributed to a major step forward in the treatment of locally advanced extremity soft tissue sarcoma (STS). High response rates and limb salvage rates have been reported in multicenter trials, which combined ILP with TNF-α plus melphalan, which resulted in the approval of TNF-α for this indication in Europe in 1998. Subsequently a series of confirmatory single institution reports on the efficacy of the procedure have now been published. TNF-α has an early and a late effect; it enhances tumor-selective drug uptake during the perfusion and plays an essential role in the subsequent selective destruction of the tumor vasculature. These effects result in a high response rate in high-grade soft tissue sarcomas. This induction therapy thus allows for resection of tumor remnants some 3 months after ILP and thus avoidance of limb amputation. TNF-α-based ILP is a well-established treatment to avoid amputations. It represents an important example of tumor vasculatory-modulating combination therapy and should be offered in large volume tertiary referral centers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with a large, high-grade soft tissue sarcoma (STS) of the extremities have a high risk for local and systemic recurrences. The local situation in the limb may require extensive and mutilating surgery followed by radiotherapy. Several studies suggested that amputation of the limb did not result in an improved survival. The tendency to perform more limb-preserving surgery has led to the exploration of isolated limb perfusion (ILP) as a procedure enabling limb salvage surgery in cases of primarily STS, requiring mutilating surgery or even amputation of the limb. The technique of ILP achieves regional drug concentrations 15–25 times higher than systemic administration and is without systemic side effects [1,2]. Isolation of the limb is achieved by clamping and cannulation of the major artery and vein, connection to an oxygenated extracorporeal circuit, ligation of collateral vessels, and application of a tourniquet (Fig. 1). Because of its efficacy and low regional toxicity profile, melphalan (l-phenyl-alaninemustard) is the standard drug and is most commonly used at a dose range of 10 mg/L (for the leg) to 13 mg/L (for the arm) [3]. ILP procedures are performed under mild hyperthermic conditions (38.5–40°C) as it has become clear that hyperthermia can increase the drug uptake in the cells, but that true hyperthermia (>41°C) is associated with increased local toxicity. Tissue temperatures are monitored and radiolabeled serum albumen or erythrocytes are injected into the perfusate to detect leakage into the systemic circulation by a precordial scintillation probe. Leakage monitoring is mandatory especially now that TNF-α is used, since leakage of TNF-α can theoretically lead to significant toxicity such as hypotension and septic shock-like syndrome. After 1–1.5 hours of perfusion, the limb is rinsed with an electrolyte solution, cannulas are removed, and the vessels are repaired. Acute tissue reactions after perfusion are classified in a 5-grade system according to Wieberdink et al. [4] (I) no reaction; (II) slight erythema and/or edema; (III) considerable erythema and/or edema with some blistering; (IV) extensive epidermolysis and/or obvious damage to the deep tissues causing definite functional disturbances; threatening or manifest compartmental syndrome; (V) reaction which may necessitate amputation. The advent of TNF-α has greatly expanded the successful application of ILP, and we will discuss these relatively recent developments.
Failure of ILP with chemotherapy alone
• Achieving limb salvage has become a key element in the management of locally advanced soft tissue sarcomas (STS) of the extremities, because there is ample evidence that amputations do not improve survival rates in patients with large (>5 cm) deep-seated high-grade sarcomas [5,6]. Locally advanced STS are often large at the time of diagnosis, and treatment options may consist of an amputation or a limb sparing extensive surgical procedure followed by radiation therapy which may cause severe disability of the limb. The insight that limb-preserving surgery is equal to amputation in terms of overall survival [7,8] greatly enhanced the interest in neoadjuvant treatment options that could reduce the size of the tumors and hence make function-preserving surgery possible. The possible role of induction chemotherapy was recently studied by the MD Anderson Cancer Center, but although a tumor response was observed in 43% of these patients, the therapy could only reduce the extent of operation in 13% and no scheduled amputation could be prevented [9]. Preoperative radiotherapy has not been studied as an induction therapy in patients with primary irresectable extremity STS. It has been shown to be as effective as postoperative radiotherapy in STS patients, but at the cost of higher wound complication rates [10]. Literature suggests that combined neoadjuvant chemoradiotherapy with limb salvage surgery is an option for treating patients with deep STS of the extremity, but up to now, this treatment option remains investigational and results from large studies have to be awaited [11–13]. ILP has the ability to deliver the highest doses of (bio)chemotherapy to the affected limb and is thus a treatment modality that can be effective in the neoadjuvant setting. In contrast to the efficacy of melphalan-based ILP for small intransit melanoma metastases, however, results of ILP with melphalan, doxorubicin, or any other drug for large STS have been very disappointing. Presumably this is mainly due to impaired drug uptake in large tumors. For treating advanced STS, ILP with chemotherapy alone was abandoned after studies in the 1970s and 1980s [14–17]. These findings were reinforced by a study of ILP with doxorubicin, where Feig and coworkers reported a dismal 0% response rate and an amputation rate of 75% [18], in line with our experience.
Success of TNF-α plus chemotherapy in ILP
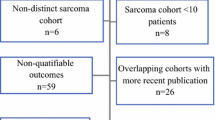
• The introduction of TNF-α in the ILP setting was pioneered by Lejeune et al. [19]. In 13 melanoma patients and four locally advanced STS cases impressive and very rapid responses were observed. This observation was followed by multicenter trials in patients with locally advanced STS [14,16,18,20] and melanoma [21–23]. Table 1 summarizes all literature reports on TNF-α-based ILP in STS patients. In the STS trials, TNF-α-based ILP was established as a highly effective new method of induction biochemotherapy for extremity STS with a 20%–30% complete remission (CR) rate and ∼50% partial remission (PR) rate [20,41,26,28]. On the basis of our multicenter trials TNF-α was approved and registered in Europe for sarcoma treatment in 1998 [28]. In four studies over a 10-year-period, the European TNF/ILP assessment group evaluated 270 ILPs in 246 patients with irresectable STS. All cases were reviewed by an independent review committee and compared with a population based Scandinavian STS database of patients receiving conventional treatment (often an amputation). There were 246 patients with local and very advanced disease. Primary sarcomas occurred in 55% of patients, local recurrent sarcomas in 45%, multifocal primary or multiple local recurrences in 22%, and overt concurrent metastatic disease in 15%. Tumors >10 cm were found in 46% of patients, and tumors were a high grade with 95% showing grade II–III tumors. In 76% of cases a delayed marginal resection of the tumor remnant was usually performed 2–4 months after ILP. Major responses were seen in 56.5%–82.6% of patients, after which resection of the sarcoma became possible in most cases. Limb salvage was achieved in 74%–87% in these four studies. In 71% of the 196 patients who had been classified by the independent review committee, 87% were considered cases that could only have been managed by amputation and 13% by functionally debilitating resection plus radiotherapy. A matched control study with cases from the Scandinavian STS Databank showed that TNF-α had no negative effect on survival (P = 0.96). In this high-risk population overall survival was around 50% at 5 years [28]. It was concluded that ILP with TNF-α and melphalan represents a new and successful option in the management of irresectable locally advanced extremity STS [28]. The approval in Europe of TNF-α for its use in the ILP setting for locally advanced STS has led to training and activation of over 40 centers in Europe to provide one or more referral programs in each country. These programs are running well and experiences are rather uniform and in line with the initial trials as is indicated by the list of single center studies that have been published over the years (Table 1) Unfortunately TNF-α is not clinically available in North America because the patent and licensing rights of TNF-α are in the hands of a different company and thus the registration file has not been presented to the FDA.
Vasculotoxic mechanism of TNF-α plus chemotherapy
• As TNF-α targets the tumor vasculature, which is a common denominator in all these tumor types, the use of TNF-α is very attractive and it explains its efficacy in combination with chemotherapy across these numerous histologies. The selective destructive effects of TNF-α-based ILP on tumor-associated vessels are illustrated in the pre- and postperfusion angiographies in Fig. 2. In magnetic resonance spectrometry studies, we have shown that shutdown of the tumor is virtually complete within 16 hours after the perfusion, confirming the likelihood of TNF-α-mediated effects on the vasculature of the tumor [42]. At the histopathological level, it has been demonstrated that TNF-α induces microvascular damage through loss of endothelial cohesion [43]. This leads to intravascular effects, such as thrombocyte aggregation and erythrostasis, with hemorrhagic necrosis as the result. The vascular destruction is important in the early and late stages after ILP [44–46]. Moreover, besides the small direct cytotoxic effect of TNF-α and the far more important vasculotoxic mechanism, speculations exist on a third role, namely the ability of TNF-α to cause an immediate drop in interstitial pressure within the tumor [47].
TNF-α enhances selective drug uptake in tumors
• We have recently demonstrated that the addition of high-dose TNF-α to the perfusate results in a 4–6 fold increased uptake by the tumor of the cytostatic drugs melphalan and doxorubicin [48,49]. Importantly this uptake was tumor specific and no increased uptake was noted in the normal tissues, thus emphasizing the selective action of TNF-α on the tumor vasculature. The more vascular the tumor was, the better the synergistic effect was between TNF-α and the chemotherapeutic agent [50]. We also demonstrated that 10 µg of TNF-α (a 5-fold reduction of the ‘standard dose of 50 µg’) was the minimum threshold dose for activity of TNF-α in our rat tumor extremity perfusion model. At 2 µg doses of TNF-α all effects were lost [51]. The results from our tumor models predict a minimum threshold activity for 1 mg TNF-α in the clinical situation and we advise not to go below that dose. We demonstrated that TNF-α and melphalan when combined with the effects of hyperthermia above 40°C leads to amputations because of normal tissue damage, and we advise against its use in the clinic [51]. Furthermore we showed that actinomycin D, commonly used in the clinical setting, leads to idiosyncratic toxicity in our models of both tumor and normal tissues, resulting in limb amputation in all cases. We strongly advise not to use TNF-α in combination with actinomycin D in the clinical setting [52].
Reports on all STS patients
• Many single center studies of TNF-α plus melphalan have been reported over the past years that showed similar response and limb salvage rates (Table 1). Studies have reported overall experience in STS patients or of special categories (see below) of STS patients. The single center reports on overall STS populations showed that response rates varied from 53% to 91% and limb salvage rates from 58% to 89%. Two reports on the combination of TNF-α with doxorubicin show very similar response rates of 62%–90% and limb salvage rates of 71%–85%, with more regional toxicity after doxorubicin compared with melphalan [29,35]. We therefore consider melphalan to be the drug of choice.
• Another aspect that has been studied in overall populations is whether high doses of TNF-α (eg, 3–4 mg) are necessary or whether lower doses (eg, 1 mg) suffice. An early clinical report by Hill and coworkers suggested that low doses of TNF-α (i.e. up to 1 mg) were sufficient because in eight STS patients eight complete responses were observed [34]. The small study size, the concomitant use of high doses of corticosteroids, and the fact that a different type of TNF-α was used, however, meant that definitive conclusions were not possible. Definitive conclusions came from the Italian studies of 1 mg TNF-α in combination with doxorubicin [29,35], the French randomized phase II trial in 100 patients on four TNF-α doses (0.5, 1.0, 2.0, and 4.0 mg) [34], and our analysis of 240 ILPs where the TNF-α doses varied from 1.0, 2.0, 3.0, and 4.0 mg. All these studies seem to indicate that TNF-α doses of 1 mg (for the arm) and 1–2 mg (for the leg) are sufficient [33]. Recently, Bedard et al. [39] confirmed their previous findings [34] of the success of low-dose TNF-α in a prospective study of 100 patients with locally advanced STS treated by ILP and 1 mg TNF-α/melphalan. This is consistent with findings from our laboratory, which indicate that doses of 1 mg TNF-α were sufficient, but further dose reduction resulted in complete loss of activity [51].
Reports on special patient categories
Patients with overt metastatic disease
• Patients who have overt metastatic disease and a limb-threatening tumor are a special category whereby tumor control can be relatively easily achieved, and amputation avoided, by a palliative TNF-α-based ILP. In nine such cases, a 77% response rate and 89% limb salvage rate was reported [53], and we observed a 84% response rate and 97% limb salvage rate in 37 cases [54]. This demonstrates that TNF-α-based ILP is an extremely attractive option in these patients.
Patients with multiple tumors in the extremity
• TNF-α-based ILP is the ideal alternative to amputation in patients with multifocal primary tumors, who are difficult to treat, such as Kaposi sarcomas [55], multiple lymphangio-sarcomas (also known as Steward Treves Syndrome) [56], or those with multiple primaries of various histologies or multiple recurrences after prior surgery [57]. Remarkably good results have been reported, and we observed a 87% response rate and a 80% limb salvage rate after 16 TNF-α-based ILPs were performed in 10 patients with Steward Treves Syndrome. In our experience, after 64 ILPs we observed a 77% response rate and 82% limb salvage rate in patients with multiple tumors. These results indicate that TNF-α-based ILP is very effective in this patient population.
Patients with recurrent tumors in an irradiated field
• We performed 29 ILPs in 26 patients with recurrent tumors in an irradiated field. In contrast to the belief that such tumors are unlikely to respond, we observed a 70% response rate and 65% limb salvage rate, indicating that in this very difficult patient category a TNF-α -based ILP approach is an attractive treatment option [58].
Patients with desmoids
• Patients with desmoid tumors and aggressive fibromatosis often present with recurrent disease, which is very difficult to treat surgically with or without radiotherapy. Lev-Lelouche et al. and our group report very similar results in 6 and 12 such cases, respectively. Response rates were 83% and 75%, respectively, and limb salvage rates were 100% in both reports, demonstrating the utility of this procedure [59,60].
Elderly patients >75 years old
• An important result was demonstrated by the report on the Rotterdam experience of patients older than 75 years with limb -threatening tumors treated with 50 TNF-α-based ILPs [61]. Results were very favorable in the 34 perfusions for limb-threatening sarcomas; a 38% CR and a 38% PR rate, achieving limb salvage in 76% of the patients, as well as in 16 perfusions for bulky melanoma intransit metastases resulting in a 75% CR and 25% PR rate, were observed. The procedure was proven safe in the elderly with limb salvage, which is of overriding importance in these patients as an amputation can abolish independency of the life [61]. In the present era of leakage-free ILPs, TNF-α-based ILPs are associated with very little toxicity problems. We have separately reported on the absence of toxicity in patients without leakage [33,62]. In the rare case of systemic leakage of TNF-α management is relatively easy and requests the use of ample hydration and non-steroid anti-inflammatory drugs, and toxicity can be minimal [63]. In our total experience of >450 ILP procedures, no toxic shock-like syndrome has occurred using this regimen. Moreover, TNF-α-based ILPs are not associated with a higher regional toxicity compared with melphalan-based ILPs, and have less regional toxicity than doxorubicin-based ILPs [64].
New vasoactive drugs
Histamine
• Because of the potential toxicity of TNF-α, alternative vasoactive drugs were investigated in our center. Histamine (Hi) is an inflammatory mediator that is formed and stored mainly in the granules of mast cells and basophils. It has also been identified in cells in regenerating or rapidly growing tissues. Its effect on fine vessels is to cause edema by increasing the flow of lump and lymph proteins into the extracellular space and also by promoting the formation of gaps between endothelial cells [65]. This effect could potentially be used to increase drug concentrations in tumor tissues. We used a sarcoma-bearing rat ILP model to assess the effects of Hi, melphalan, and the combination [66]. The antitumor effect of the combination Hi and melphalan was synergistic. The strong effect of Hi-based-ILP with melphalan was explained by three mechanisms: direct cytotoxicity to the tumor cells, direct cytotoxicity to the tumor-associated vasculature, and indirect effect through Hi-mediated increased melphalan concentration in the tumor. There are several theoretical advantages in using Hi instead of TNF-α. In brief; it has been hypothesized that ILP with Hi would likely enhance drug uptake more quickly and effectively than ILP with TNF-α, and Hi is a potentially safer drug than TNF-α in case of leakage into the systemic circulation during ILP [66].
Interleukin-2
• Interleukin-2 (IL-2) is another candidate to enhance tissue uptake of cytotoxic agents. IL-2 is a mediator of immune cell activation with some antitumor activity. IL-2 causes vascular leakage and edema and for this reason we examined the antitumor activity of a combined treatment with IL-2 and melphalan in an experimental ILP setting [67]. ILPs were performed in soft tissue sarcoma-bearing rats. ILP with either IL-2 or melphalan alone has no antitumor effect, but the combination of IL-2 and melphalan resulted in a strong synergistic tumor response, without any local or systemic toxicity. IL-2 significantly enhanced melphalan uptake in tumor tissue without signs of significant vascular damage to account for this observation. Observations indicated a potentially important role for macrophages as an explanation for the strong synergistic effect of IL-2. In systemic immunotherapy, the combination of IL-2 and Hi has been used for solid tumor treatment based on immunomodulatory effects. Also because of the success of IL-2 in ILP and the earlier-mentioned success of Hi in ILP model, we studied if the two drugs combined with melphalan could further improve response rates in an experimental ILP. In a sarcoma-bearing rat ILP model the effects were assessed [68]. A negative synergistic effect was found between IL-2 and Hi in a regional setting.
Conclusions and future directions
• ILP methodology provides us an excellent tool in the clinic to obtain local control and avoid amputations of limbs in patients with limb-threatening tumors. This has been largely achieved by the success of the antivascular TNF-based biochemotherapy in this setting. TNF-α, for the first time, has brought us an effective treatment against large, bulky tumors. TNF-α-based ILP is a very successful treatment option to achieve limb salvage in the management of advanced disease, multiple or drug-resistant extremity tumors. TNF-α-based ILPs are now performed in over 40 cancer centers in Europe with referral programs for limb salvage. Provision should be made to make TNF-α available in North America. TNF-α-based antivascular therapy of cancer is here to stay and its potential needs to be studied further, including its use in the systemic setting. In the field of isolated-perfusion newly discovered vasoactive drugs await evaluation in clinical trials [69].
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: •Of importance ••Of major importance
Creech O et al. (1958) Chemotherapy of cancer: regional perfusion utilising an extracorporeal circuit. Ann Surg 148:616–632
Benckhuijsen C et al. (1988) Regional perfusion treatment with melphalan for melanoma in a limb: an evaluation of drug kinetics. Eur J Surg Oncol 14:157–163
Thompson JF, Gianoutsos MP (1992) Isolated limb perfusion for melanoma - effectiveness and toxicity of cisplatin compared with that of melphalan and other drugs. World J Surg 16:227–233
Wieberdink K et al. (1982) Dosimetry in isolation perfusion of the limbs by assessment of perfused tissue volume and grading of toxic tissue reactions. Eur J Cancer Clin Oncol 18:905–910
Stotter AT et al. (1990) The influence of local recurrence of extremity soft tissue sarcoma on metastasis and survival. Cancer 65:1119–1129
Gustafson P et al. (1991) Is local recurrence of minor importance for metastases in soft tissue sarcoma? Cancer 67:2083–2086
Rosenberg SA, Tepper J, Glatstein E et al. (1982) The treatment of soft-tissue sarcomas of the extremities: prospective randomized evaluations of (1) limb-sparing surgery plus radiation therapy compared with amputation and (2) the role of adjuvant chemotherapy. Ann Surg 196(3):305–315
Williard WC, Hajdu SI, Casper ES, Brennan MF. (1992) Comparison of amputation with limb-sparing operations for adult soft tissue sarcoma of the extremity. Ann Surg.;215(3):269–275
Meric F, Hess KR, Varma DG et al. Radiographic response to neoadjuvant chemotherapy is a predictor of local control and survival in soft tissue sarcomas. Cancer 2002;95(5):1120–1126
O’Sullivan B, Davis AM, Turcotte R et al. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Lancet 2002;359(9325):2235–2241
Pisters PW, Ballo MT, Patel SR. Preoperative chemoradiation treatment strategies for localized sarcoma. Ann Surg Oncol 2002;9(6):535–542
DeLaney TF, Spiro IJ, Suit HD et al. Neoadjuvant chemotherapy and radiotherapy for large extremity soft-tissue sarcomas. Int J Radiat Oncol Biol Phys 2003;56(4):1117–1127
Mack LA, Crowe PJ, Yang JL et al. Preoperative chemoradiotherapy (modified Eilber Protocol) provides maximum local control and minimal morbidity in patients with soft tissue sarcoma. Ann Surg Oncol 2005;12(8):646–653
Krementz ET et al. (1977) Chemotherapy of sarcomas of the limbs by regional perfusion. Ann Surg 185:555–564
Pommier RF et al. (1988) Pharmacokinetics, toxicity, and short-term results of cisplatin hyperthermic isolated limb perfusion for soft tissue sarcoma and melanoma of the extremities. Am J Surg 155:667–671
Klaase JM et al. (1989) Results of regional isolation perfusion with cytostatics in patients with soft tissue tumors of the extremities. Cancer 64:616–621
Rossi CR et al. (1994) Phase II study on neoadjuvant hyperthermic-antiblastic perfusion with doxorubicin in patients with intermediate or high grade limb sarcomas. Cancer 73:2140–2146
Feig BW et al. (2004) A prospective evaluation of isolated limb perfusion with doxorubicin in patients with unresectable extremity sarcomas. Ann Surg Oncol 11:S80
Lienard D et al. (1992) High-dose recombinant tumor necrosis factor alpha in combination with interferon gamma and melphalan in isolation perfusion of the limbs for melanoma and sarcoma. J Clin Oncol 10:50–62
Eggermont AM et al. (1996) Isolated limb perfusion with high-dose tumor necrosis factor-alpha in combination with interferon-gamma and melphalan for nonresectable extremity soft tissue sarcomas: a multicenter trial [see comments]. J Clin Oncol 14:2653–2665
Eggermont AM, Kirkwood JM. Re-evaluating the role of dacarbazine in metastatic melanoma: what have we learned in 30 years? Eur J Cancer 2004; 40:1825–1836
Lejeune FJ et al. (1993) Regional therapy of melanoma. Eur J Cancer 29A:606–612
Fraker DL et al. (1996) Treatment of patients with melanoma of the extremity using hyperthermic isolated limb perfusion with melphalan, tumor necrosis factor, and interferon gamma: results of a tumor necrosis factor dose-escalation study. J Clin Oncol 14:479–489
Hill S et al. (1993) Low dose tumor necrosis factor-alpha and melphalan in hyperthermic isolated limb perfusion. Br J Surg 80:995–997
Santinami M et al. (1996) Treatment of recurrent sarcoma of the extremities by isolated perfusion using tumor necrosis factor alpha and melphalan. Tumori 82:579–584
Eggermont AM et al. (1996) Isolated limb perfusion with tumor necrosis factor and melphalan for limb salvage in 186 patients with locally advanced soft tissue extremity sarcomas. The cumulative multicenter European experience. Ann Surg 224:756–764; discussion 764–765
Gutman M et al. (1997) High dose tumor necrosis factor-alpha and melphalan administered via isolated limb perfusion for advanced limb soft tissue sarcoma results in a >90% response rate and limb preservation. Cancer 79:1129–1137
Eggermont AM et al. (1999) Limb salvage by isolation limb perfusion with tumor necrosis factor alpha and melphalan for locally advanced extremity soft tissue sarcomas: results of 270 perfusions in 246 patients. Proc Am Soc Clin Oncol 11:497
Rossi CR et al. (1999) Soft tissue limb sarcomas: Italian clinical trials with hyperthermic antiblastic perfusion. Cancer 86:1742–1749
Lejeune FJ et al. (2000) Limb salvage by neoadjuvant isolated perfusion with TNFalpha and melphalan for non-resectable soft tissue sarcoma of the extremities. Eur J Surg Oncol 26:669–678
Hohenberger P et al. (2001) Functional outcome after preoperative isolated limb perfusion with rhTNFalpha/melphalan for high-grade extremity sarcoma. Eur J Cancer 37:S34–S35
Noorda EM et al. (2003) Isolated limb perfusion with tumor necrosis factor-alpha and melphalan for irresectable soft tissue sarcoma of the extremities. Cancer 98:1483–1490
Grünhagen DJ et al. (2005) TNF dose reduction in isolated limb perfusion. Eur J Surg Oncol 31:1011–1019
Bonvalot S et al. (2005) Limb salvage with isolated perfusion for soft tissue sarcoma: could less TNF-alpha be better? Ann Oncol 16:1061–1068
Rossi CR et al. (2005) Hyperthermic isolated perfusion with low-dose tumor necrosis factor alpha and doxorubicin for the treatment of limb-threatening soft tissue sarcomas. Ann Surg Oncol 12:398–405
Grünhagen DJ et al. (2006) Outcome and prognostic factor analysis of 217 consecutive isolated limb perfusions with tumor necrosis factor-alpha and melphalan for limb-threatening soft tissue sarcoma. Cancer 106:1776–1784
Pennacchioli E, Deraco M, Mariani L et al. Advanced extremity soft tissue sarcoma: prognostic effect of isolated limb perfusion in a series of 88 patients treated at a single institution. Ann Surg Oncol 2007;14(2):553–559
van Ginkel RJ, Thijssens KM, Pras E, van der Graaf WT, Suurmeijer AJ, Hoekstra HJ. Isolated limb perfusion with tumor necrosis factor alpha and melphalan for locally advanced soft tissue sarcoma: three time periods at risk for amputation. Ann Surg Oncol 2007;14(4):1499–1506
Bedard V, Vataire C, Desouche C et al. A prospective database of 100 patients with locally soft tissue sarcoma (STS) treated by isolated limb perfusion with melphalan and TNFα 1 mg. J Clin Oncol Proc 2007; 25(18S):10010
Hayes AJ, Neuhaus SJ, Clark MA, Thomas JM. Isolated limb perfusion with melphalan TNF for advanced melanoma and soft-tissue sarcoma. Ann Surg Oncol 2007;14(1):230–238
Eggermont AM et al. (1993) Treatment of irresectable soft tissue sarcomas of the limbs by isolation perfusion with high dose TNF-α in combination with gamma-interferon and melphalan. In: Fiers W, Buurman WA (eds) Tumor Necrosis Factor: Molecular and Cellular Biology and Clinical Relevance. Basel, Karger Verlag, 239–243
Sijens PE et al. (1995) 31P magnetic resonance spectroscopy as predictor for clinical response in human extremity sarcomas treated by single dose TNF-alpha + melphalan isolated limb perfusion. NMR Biomed 18:215–224
Ruegg C, Yilmaz A, Bieler G, Bamat J, Chaubert P, Lejeune FJ. Evidence for the involvement of endothelial cell integrin alphaVbeta3 in the disruption of the tumor vasculature induced by TNF and IFN-gamma. Nat Med 1998; 4:408–414
Renard N et al. Early endothelium activation and polymorphonuclear cell invasion precede specific necrosis of human melanoma and sarcoma treated by intravascular high-dose tumour necrosis factor alpha (TNFα). Int J Cancer 1994; 57:656–663
Nooijen PTGA et al. (1998) Complete response of melanoma in-transit metastasis after isolated limb perfusion with tumor necrosis factor-alpha and melphalan without massive tumor necrosis: clinical and histopathological study of the delayed-type reaction patterns. Cancer Res 58:4880–4887
Fraker DL et al. (2002) A phase III trial of isolated limb perfusion for extremity melanoma comparing melphalan alone versus melphalan plus tumor necrosis factor (TNF) plus interferon gamma (IFN). Ann Surg Oncol 9:S8
Kristensen CA, Nozue M, Boucher Y, Jain RK. Reduction of interstitial fluid pressure after TNF-alpha treatment of three human melanoma xenografts. Br J Cancer 1996; 74:533–536
De Wilt JHW et al. (2000) Tumour necrosis factor alpha increases melphalan concentration in tumour tissue after isolated limb perfusion. Br J Cancer 82:1000–1003
van der Veen AH et al. (2000) TNF-alpha augments intratumoural concentration of doxorubicin in TNF-α-based isolated limb perfusion in rat sarcoma models and enhances antitumour effects. Br J Cancer 82:973–980
van Etten B et al. (2003) Degree of tumour vascularity correlates with drug accumulation and tumour response upon TNF-based isolated hepatic perfusion. Br J Cancer 87:314–319
DeWilt JHW et al. (1999) Prerequisites for effective isolated limb perfusion using tumour necrosis factor-alpha and melphalan in rats. Br J Cancer 80:161–166
Seynhaeve ALB et al. (2002) Isolated limb perfusion with actinomycin D and TNF-alpha results in improved tumour response in soft-tissue sarcoma-bearing rats but is accompanied by severe local toxicity. Br J Cancer 86:1174–1179
Olieman AF et al. (1998) Hyperthermic isolated limb perfusion with tumour necrosis factor-alpha and melphalan as palliative limb-saving treatment in patients with locally advanced soft-tissue sarcomas of the extremities with regional or distant metastases. Is it worthwhile? Arch Orthop Trauma Surg 118:70–74
Grünhagen DJ et al. (2006) Palliative value of TNF-based ILP in metastatic melanoma and sarcoma patients. Cancer 106:156–162
Lev-Chelouche et al. (1999) Isolated limb perfusion with high-dose tumor necrosis factor alpha and melphalan for Kaposi sarcoma. Arch Surg 134:177–180
Lans TE et al. (2002) Isolated limb perfusion with tumor necrosis factor and melphalan for nonresectable stewart-treves lymphangiosarcoma. Ann Surg Oncol 9:1004–1009
Grünhagen DJ et al. (2005) Isolated limb perfusion with tumor necrosis factor and melphalan prevents amputation in patients with multiple sarcomas in arm or leg. Ann Surg Oncol 12:473–479
Lans TE et al. (2005) Isolated limb perfusions with tumor necrosis factor and melphalan for locally recurrent soft tissue sarcoma in previously irradiated limbs. Ann Surg Oncol 12:406–411
Lev-Chelouche D et al. (1999) Limb desmoid tumors: a possible role for isolated limb perfusion with tumor necrosis factor-alpha and melphalan. Surgery 126:963–967
Grünhagen DJ et al. (2005) TNF-based isolated limb perfusion for unresectable extremity desmoid tumors. Eur J Surg Oncol 31:912–916
Etten van B et al. (2003) Fifty tumor necrosis factor-based isolated limb perfusions for limb salvage in patients older than 75 years with limb-threatening soft tissue sarcomas and other extremity tumors. Ann Surg Oncol 27:32–37
Vrouwenraets BC et al. (1999) Absence of severe systemic toxicity after leakage controlled isolated limb perfusion with tumor necrosis factor alpha and melphalan. Ann Surg Oncol 6:405–412
Stam TC et al. (2000) Systemic toxicity and cytokine/acute phase protein levels in patients after isolated limb perfusion with tumor necrosis factor-alpha complicated by high leakage [in process citation]. Ann Surg Oncol 4:268–275
Vrouenraets BC et al. (2001) Regional toxicity after isolated limb perfusion with melphalan and tumour necrosis factor-alpha versus toxicity after melphalan alone. Eur J Surg Oncol 27:390–395
Garrison JC. Histamine, bradykinin, 5-hydroxytryptamine and their antagonist. In: AG Gilman, TW Rall, AS Nie, P Taylor, editors. The Pharmacological basis of therapeutics. 8th ed. Elmsford-New York: Pergamon Press, 1990:575–599
Brunstein F et al. (2004) Synergistic antitumor activity of histamine plus melphalan in isolated limb perfusion: preclinical studies. J Natl Cancer Inst 96:1603–1610
Hoving S et al. (2005) Synergistic antitumor response of interleukin 2 with melphalan in isolated limb perfusion in soft tissue sarcoma-bearing rats. Cancer Res 65:4300–4308
Brunstein F, Hoving S, aan de Wiel-Ambagtsheer G. Decreased response rates by the combination of histamine and IL-2 in melphalan-based isolated limb perfusion. Cancer Immunol Immunother 2007;56(4):573–580
Ten Hagen TLM, Eggermont AM (2001) TNF is here to stay — revisited. Trends Immunol (Formerly Immunology Today) 22:127–129
Author information
Authors and Affiliations
Corresponding author
Additional information
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Verhoef, C., de Wilt, J.H.W., Grünhagen, D.J. et al. Isolated Limb Perfusion with Melphalan and TNF-α in the Treatment of Extremity Sarcoma. Curr. Treat. Options in Oncol. 8, 417–427 (2007). https://doi.org/10.1007/s11864-007-0044-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11864-007-0044-y