Abstract
Background
The timely assessment of B-type natriuretic peptide (BNP) marking chronic heart failure risk in patients with coronary heart disease (CHD) helps to reduce patients’ mortality.
Objective
To evaluate the potential of wrist pulse signals for use in the cardiac monitoring of patients with CHD.
Methods
A total of 419 patients with CHD were assigned to Group 1 (BNP < 95 pg/mL, n = 249), 2 (95 < BNP < 221 pg/mL, n = 85), and 3 (BNP > 221 pg/mL, n = 85) according to BNP levels. Wrist pulse signals were measured noninvasively. Both the time-domain method and multiscale entropy (MSE) method were used to extract pulse features. Decision tree (DT) and random forest (RF) algorithms were employed to construct models for classifying three groups, and the models’ performance metrics were compared.
Results
The pulse features of the three groups differed significantly, suggesting different pathological states of the cardiovascular system in patients with CHD. Moreover, the RF models outperformed the DT models in performance metrics. Furthermore, the optimal RF model was that based on a dataset comprising both time-domain and MSE features, achieving accuracy, average precision, average recall, and average F1-score of 90.900%, 91.048%, 90.900%, and 90.897%, respectively.
Conclusions
The wrist pulse detection technology employed in this study is useful for assessing the cardiac function of patients with CHD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the World Health Organization, coronary heart disease (CHD) is the leading cause of death among cardiovascular diseases, and its global prevalence continues to increase [1, 2]. Chronic heart failure is a secondary complication to various cardiovascular diseases and is commonly observed in the terminal stage of CHD [3]. Accumulating epidemiological evidence has indicated that chronic heart failure leads to significantly higher clinical mortality and hospital readmission rates as a complication of CHD, and the prognosis is poor [4, 5]. Therefore, more attention must be paid to the cardiac function of patients with CHD to prevent progression to chronic heart failure.
B-type natriuretic peptide (BNP) is one of the most potent biomarkers secreted by cardiac ventricular myocytes [6, 7] and is extensively used for chronic heart failure risk stratification and adverse outcome prediction [8]. BNP levels can be used to determine the severity of myocardial ischemia and myocardial injury [9, 10]. Thus, timely BNP monitoring is for cardiac function assessment in patients with CHD to prevent progression to chronic heart failure. However, BNP is generally measured as a diagnostic and prognostic test for patients with cardiovascular diseases only during hospital admission. Therefore, wearable, noninvasive, and convenient technology for out-of-hospital monitoring of the cardiac function of patients with CHD is desirable.
Pulse diagnosis is a diagnostic skill unique to traditional Chinese medicine (TCM). By touching and sensing pulsations at the radial artery, TCM practitioners can distinguish pulse patterns and obtain pathophysiological information about the human body. However, TCM practitioners often have different interpretations of pulse patterns and diagnose conditions on the basis of their own experiences. Thus, the objectification and digitization of TCM pulse diagnosis are challenging but crucial for ensuring accuracy and repeatability. Considerable efforts have been made to realize objective pulse diagnosis through multidisciplinary based on sensing, computer science, and biomedicine. Multiple pulse detection instruments have been developed to record and analyze pulse signals at the radial artery. In addition, the processing of such signals, including preprocessing, feature extraction, and recognition, are crucial to objective pulse diagnosis. With the development of information technology and artificial intelligence (AI), techniques for extracting time-domain and nonlinear time series features from pulse signals through linear to nonlinear methods have been developed. Machine learning (ML), the core AI technology, provides intelligent solutions to medical classification problems. Wrist pulse detection technology, including signal identification and processing, has gradually been applied for classification in cardiovascular diseases [11,12,13,14,15]. The development of wearable healthcare devices has facilitated the application of AI to the monitoring of multiple diseases such as CVDs, corneal disease, and cancer [16,17,18].
In the present study, we investigated the potential of wrist pulse detection technology for monitoring the cardiac function of patients with CHD through BNP level assessment based on pulse signals.
The highlights of the present study are as follows:
-
1.
The wrist pulse signals of patients with CHD were measured during admission, and these patients were divided into three groups based on their BNP levels at the time.
-
2.
Pulse features were extracted through time-domain and multiscale entropy (MSE) methods and were statistically analyzed to determine the differences among the three groups.
-
3.
Decision tree (DT) and random forest (RF) algorithms were respectively used to construct classification models based on pulse features; the performance of the different classification models was compared in terms of accuracy, precision, recall, and F1-score.
-
4.
The RF model based on an input data set comprising both time-domain and MSE features achieved the highest performance and may be a novel means of monitoring and assessing the cardiac function of patients with CHD.
The remainder of this manuscript is arranged as follows: “Data and methods” describe the data and methods, “Results” reveal the results, “Discussion” provides the discussion, and “Conclusion” presents the conclusions.
Data and methods
Study patients
Patients admitted to Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shuguang Hospital, and Shanghai Hospital of Traditional Chinese Medicine (affiliated with Shanghai University of Traditional Chinese Medicine) during 2018–2020 were enrolled in the present study if they (1) had a CHD diagnosis, (2) could cooperate with researchers to complete the symptom and sign assessments and provision of related medical history data, (3) were willing to undergo a complete clinical examination, and (4) provided written informed consent. Patients were excluded if they had (1) clinically acute myocardial infarction or acute heart failure; (2) severe obstruction with hypertrophic obstructive or dilated cardiomyopathy; (3) severe diseases such as malignant tumors or HIV; (4) severe respiratory diseases such as respiratory failure, tuberculosis, or primary bronchopulmonary carcinoma; or (5) a pacemaker.
All patients voluntarily participated in the present study and provided informed consent for us to use their personal information. All personal information was kept strictly confidential. This study was approved by the ethics committee of the Shanghai University of Traditional Chinese Medicine.
Grouping principles
Original BNP values were converted into five level according to the expert consensus on BNP clinical application recommendations published by the American College of Cardiology [19], the patients were divided into three groups (as presented in Table 1). Patients with BNP levels < 95 pg/mL were assigned to Group 1 (n = 249). Patients with BNP levels > 95 pg/mL were further divided; those with BNP levels > 95 and < 221 pg/mL were assigned to Group 2 (n = 85), and those with BNP levels > 221 pg/mL were assigned to Group 3 (n = 85).
Measurement of pulse signals
Smart TCM-I pulse detection equipment developed by the Shanghai University of Traditional Chinese Medicine and Shanghai Asia and Pacific Computer Information System was used to collect wrist pulse signals. All patients were instructed to lie down in a quiet environment for at least 3 min and maintain a relaxed wrist. The pressure sensor of the detection equipment was attached to a wristband wrapped around the patients’ left wrist, and the pulse signals at the peak amplitude of the pulse at the left radial artery were recorded for 60 s.
Methods of extracting features from pulse signals
The wrist pulse signals were processed for feature extraction through the time-domain and MSE methods.
Time-domain method
The time-domain method focuses on analyzing the waveform of the wrist pulse signal owing to the peak and trough points of the waveform have certain physiological significance. Seven main feature points were extracted from a representative pulse wave of a cardiac cycle shown in Fig. 1 [20], namely, the start point (A), the main wavepeak (B), the main wave gap (C), the tidal wave peak (D), the dicrotic notch (E), the dicrotic wave peak (F), and the end point (G). According to seven key feature points, three types of time-domain features, including magnitudes features, duration features, and proportional features, were finally extracted in the present study as presented in Table 2.
MSE method
Biological systems can function on multiple time scales. Typically, biosignals are multiscaled, and their properties depend on the scale of analysis. Therefore, Costa et al. proposed the MSE method for estimating entropies from an entire set of coarse-grained time series to quantify the series’ complexity [21, 22]. The MSE method has been widely applied to quantify various biosignals, including electroencephalograpy [23], electrocardiography [24], and electromyography [25] signals. The wide application of MSE in medical diagnosis and analysis are due to its ability to correct the erratic estimations of traditional entropy-based methods [26]. Therefore, we employed the MSE method to extract MSE features of pulse signals across multiple temporal scales and quantify their complexity for different physiological and pathological states of the cardiovascular system.
MSE is an improvement of sample entropy. The procedure for the computation of MSE involves the construction of coarse-grained time series at a specific time scale and the computation of the series’ sample entropy.
Given a time series \(x=\left\{{x}_{i}\right\},\mathrm{i}=1,\dots ,\mathrm{N}.\) The coarse-grained time series was constructed by taking the average value of consecutive data points in a non-overlapping window of data samples equal in length to time scale (Fig. 2) [27] and was described with the following formula:
where yj is a data point after a “coarse-grained” time series, s is the scale factor, xi is a data point in the original time series, and N is the length of the original time series. In this paper, the maximum of scale factor s is 5.
Illustration of the signal coarse-grained procedure [28]
In the present study, multiscale analysis was using the mean operator’s coarse-grained procedure for all pulse signals to generate the time series at a specific scale. For each scale factor s (s = 1, 2, 3, 4, 5), the sample entropy of each coarse-grained time series was calculated. MSEs (s = 1, 2, 3,4,5) represents the value of sample entropy of s-th scale.
ML methods
ML algorithms are the mainstream approaches to using AI for disease diagnosis and prediction. In the present study, we used two common ML algorithms—the DT and RF algorithms—to construct models for classifying patients into three groups.
A DT is a tree-like regression classifier in which nodes represent attributes, links represent decision rules, and leaf nodes represent output classes. Optimal classification is achieved through the construction of a tree-like structure for feature input and creation of a unique output for every leaf [29]. However, an RF algorithm is constructed from a series of decision trees with low reciprocal correlation, and the class output by the most decision trees is the class output by the RF. The RF algorithm uses features randomly selected through bootstrap aggregation to obtain precise and stable classifications and predictions. Figure 3 illustrates how RF functions for classification [30].
Evaluation metrics
In the present study, various classification models were constructed on the basis of three data sets and two ML algorithms. The accuracy, precision, recall, and F1-score of these methods were calculated. These were calculated as follows:
Statistical analysis
Data analysis was performed using SPSS Statistics 25.0 (IBM, Armonk, NY, USA) to compare the pulse features and other data among the three groups.
Continuous variables were compared using the nonparametric Wilcoxon–Mann–Whitney test and are presented as median values with first and third quartiles (M (Q1, Q3)). Categorical data were compared using the chi-square test, and the results are expressed as numbers (percentages). A P value of < 0.05 was considered statistically significant.
Results
General group information
The groups’ general information (sex distributions, age, body mass index (BMI)) is presented in Table 3. The age of Group 1 was lower than those of Groups 2 and 3 (P < 0.05). BMI was lower in Group 3 than in Groups 1 and 2 (P < 0.05). The sex distributions did not differ significantly among the groups (P = 0.556).
Comparison of time-domain features among BNP level groups
Among the time-domain features, the duration and proportional features in Table 2 can objectively reflect pathophysiological morphological changes in the pulse waveform; therefore, these features were selected for comparison among the three groups. The time-domain features that differed significantly among the three groups were t5, T, h4/h1, t1/T, w1, w2, w1/T, and w2/T (Table 4), whereas the other features were not significantly different. Here, t5 represents the left ventricular diastolic period; T represents the cardiac cycle, reflecting heart rate; h4/h1 reflects peripheral resistance; t1/T reflects the ejection function of the heart; and w1, w2, w1/T, and w2/T reflect the duration of elevated aortic pressure [31].
As shown in Table 4, Group 3 had lower h4/h1 (P < 0.01), w1 (P < 0.05), w1/T (P < 0.01), and w2/T (P < 0.05) values than Group 1; lower t5, T (P < 0.01), and w2 (P < 0.05) values than Group 2; and a higher t1/T (P < 0.05) value than Group 2.
Comparison of MSE features among BNP level groups
The MSE features of the three groups are listed in Table 5. The MSEs (s = 1, 2, 3, 4, 5) values in Group 1 were higher than those in Groups 2 and 3, and the difference from Group 2 was significant (P < 0.05). However, the MSEs (s = 1, 2, 3, 4, 5) values in Group 2 were lower than those in Group 3 (P < 0.05).
ML models for classifying BNP level groups
Learning the distribution pattern of an input data set aids in medical data classification using ML. In the present study, 419 samples were used to train and test the models. Because the three groups had different sample sizes, the synthetic minority oversampling technique (SMOTE) algorithm [32] was employed to equalize the sample size (n = 249) and avoid overfitting. The input data sets for modeling were (1) Dataset1, containing time-domain features and general information; (2) Dataset2, containing MSE features and general information; and (3) Dataset3, containing time-domain features, MSE features, and general information. The DT and RF algorithms were used to construct classification models based on all three datasets. The models were validated through fivefold cross-validation; that is, 80% of the pulse samples were used for training, and the remaining 20% were used for testing.
DT models for classifying BNP level groups
Tables 6, 7, and 8 present the classification results of DT models based on Dataset1, Dataset2, and Dataset3, respectively. Because the sample sizes of the three groups were balanced, accuracy and average recall were equivalent. The model based on Dataset3 had the best performance, followed by the models based on Dataset2 and Dataset1. Specifically, the model based on Dataset3 had the highest average precision, recall, and F1-score: 78.808%, 79.116%, and 78.684%, respectively.
RF models for classifying BNP level groups
Tables 9, 10, and 11 present the classification results of RF models based on Dataset1, Dataset2, and Dataset3, respectively. Because the sample sizes of the three groups were the same, accuracy and average recall were equivalent. The model based on Dataset3 had the highest average precision, recall, and F1-score: 91.048%, 90.897%, and 90.797%, respectively.
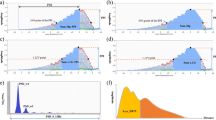
Performance comparison of DT and RF models
All RF models outperformed all DT models in terms of accuracy, average precision, average recall, and average F1-score (Fig. 4). Therefore, the RF algorithm was considered more suitable for modeling. The best performance among the RF models was achieved by that based on Datasets3, indicating that a combination of pulse feature types could yield more useful information than either type alone because of their reflection of different types of cardiovascular information.
Discussion
Pulse waves are formed by the contraction of the heart and propagate outward through the arteries and blood. Various physiological factors such as blood flow, blood pressure, and the elasticity of the vascular walls of arteries and branches affect pulse waves; thus, pulse waves contain rich physiological and pathological information regarding the cardiovascular system. In TCM, pulse diagnosis is a method of measuring pulse pulsations at the radial artery to obtain human physiological and pathological information including cardiovascular information. AI facilitates medical practice and patient care and may be a powerful tool for digitalizing pulse diagnosis and improving the clinical value of the technique.
CHD complicated by chronic heart failure is common. Monitoring and identifying the emergence and development of CHD complicated by chronic heart failure and providing timely and effective clinical intervention can significantly reduce the mortality rate of patients. Current cardiac function detection methods involve coronary angiography, ultrasonic and conventional electrocardiography, and the monitoring of myocardial injury markers. These detection methods are complex and require professionals to perform, limiting their out-of-hospital application. However, wrist pulse detection can be used to conveniently, affordably, and noninvasively obtain information on the cardiovascular system through the safe monitoring of pulse signals. Therefore, we analyzed wrist pulse signals to classify patients with CHD by three BNP levels, thereby exploring the potential role of pulse signals in the real-time monitoring of cardiac function. Our findings were as follows.
The CHD patients in Group 3, who had the highest BNP levels, were older and had a lower average BMI, suggesting that cardiac function deterioration in patients with CHD is associated with old age and low BMI. A recent study observed higher mortality in lightweight patients with cardiovascular diseases than in overweight patients; this association is attributable to factors such as aging and the sarcopenia and poor nutrition of the underweight population [33].
In the present study, the time-domain features h4/h1, w1, w1/T, and w2/T were lower in Group 3 (highest BNP level) than in Group 1, possibly because patients with CHD and severe chronic heart failure have insufficient arterial blood volume. Compared with Group 2, Group 3 had lower t5 and T values and a higher t1/T value, indicating that patients with CHD and severe chronic heart failure have faster heart rates (reflected by lower t5 and T) and inadequate cardiac ejection capacity (reflected by higher t1/T). An increase in BNP indicates the exacerbation of myocardial injury, revealing poorer myocardial contractility and leading to limited cardiac ejection capacity, insufficient arterial blood volume, and lower arterial blood pressure. As myocardial systolic function declines, the heart rate may increase to compensate. These pathological changes can be reflected by changes in the time-domain features of pulse signals.
The MSE method can be used to analyze the complexity of a biological time series on different scales [34]. Larger entropy values indicate less predictability and more complex dynamics [35]. Our results showed that the MSEs (s = 1, 2, 3, 4, 5) values in Groups 2 and 3 (higher BNP levels) were lower than those in Group 1 (normal BNP levels), indicating less complexity pulse signals (all P < 0.05). Moreover, the MSEs values in Group 2 were significantly lower in Group 2 (moderately increased BNP levels) than in Group 3 (highest BNP levels; P < 0.05). This result may be due to arrhythmias in the Group 3 patients with chronic heart failure, which may lead to more random heartbeats and thus more complex pulse signals. Therefore, MSEs values extracted from pulse signals may indicate the various pathological states associated with BNP levels.
ML, the core AI technology, is developing rapidly and provides intelligent solutions to medical classification problems. In the present study, RF and DT models based on three data sets were used to classify patients with different BNP level, and the RF models were superior to the DT models. As an ensemble learning algorithm, the RF is fast for model training, is robust to outliers, and can solve the problem of insufficient precision of a single classifier [36]. Among the RF models, the model based on the data set comprising both time-domain and MSE features achieved the best performance, indicating that a combination of pulse feature types is most informative. The time-domain features identify various morphology of pulse waveforms to obtain physiological and pathological information corresponding to different pulse morphology. MSE features represent the complexity of pulse signals because MSE is a novel nonlinear approach to measure the complexity of biological systems on multiple scales. Therefore, the two types of pulse features can complement each other to obtain rich cardiovascular information for effective classification.
Conclusion
The time-domain and MSE features of wrist pulse signals were used to construct an RF-based model for classifying BNP level; this model achieved the superior performance with an accuracy of 90.9%, average precision of 91.048%, average recall of 90.897%, and an average F1-score of 90.797%. This study demonstrates the potential of combining wearable pulse detection technology with AI to easily assess cardiac function outside of hospitals. In the future, more types of pulse features, larger data sets, and deep learning should be considered to improve analysis.
Data availability
The datasets generated and analyzed during the current study are not publicly available due to the confidentiality of the data, which is an important component of the National Science Foundation of China (No. 82074332) in China, but are available from the corresponding author on reasonable request.
Abbreviations
- CHD:
-
Coronary heart disease
- BNP:
-
B-type Natriuretic Peptide
- MSE:
-
Multiscale entropy
- ML:
-
Machine learning
- DT:
-
Decision tree
- RF:
-
Random forest
- WHO:
-
World Health Organization
- TCM:
-
Traditional Chinese medicine
- SMOTE:
-
Synthetic minority oversampling technique
- BMI:
-
Body mass index
- AI:
-
Artificial intelligence
References
WHO. Cardiovascular diseases (CVDs) key facts [EB/OL]. (2017–5–17) [2020–10–30]. https://www.who.int/zh/news-room/fact-sheets/detai/cardiovascular-diseases-(cvds)
Timmis A, Townsend N, Gale C et al (2018) ESC scientific document group. european society of cardiology: cardiovascular disease statistics 2017. Eur Heart J 39(7):508–579. https://doi.org/10.1093/eurheartj/ehx628. [PubMed] [CrossRef] [Google Scholar]
Berezin AE, Kremzer AA, Samura TA (2015) Circulating thrombospondine-2 in patients with moderate-to-severe chronic heart failure due to coronary artery disease. J Biomed Res 2:30. https://doi.org/10.7555/JBR.29.20140025. [PubMed] [CrossRef] [GoogleScholar]
Guo B, Yang T, Nan J et al (2021) Efficacy and safety of Shenfu injection combined with sodium nitroprusside in the treatment of chronic heart failure in patients with coronary heart disease: a protocol of randomized controlled trial. Medicine (Baltimore) 100(7):e24414. https://doi.org/10.1097/MD.0000000000024414. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Yu P, Liu M, Yang X et al (2016) Diagnostic utility of ANG in coronary heart disease complicating chronic heart failure: a cross-sectional study. Dis Markers 2016:2740826. https://doi.org/10.1155/2016/2740826. [PMCfreearticle] [PubMed] [CrossRef] [GoogleScholar]
Mueller C, Scholer A, Laule-Kilian K et al (2004) Use of B-type natriuretic peptide in the evaluation and management of acute dyspnea. N Engl J Med 350(7):647–654. https://doi.org/10.1056/NEJMoa031681. [PubMed] [CrossRef] [GoogleScholar]
Harrison A, Morrison LK, Krishnaswamy P et al (2002) B-type natriuretic peptide predicts future cardiac events in patients presenting to the emergency department with dyspnea. Ann Emerg Med 39(2):131–138. https://doi.org/10.1067/mem.2002.121483. [PubMed] [CrossRef] [GoogleScholar]
Brunner-La Rocca HP, Sanders-van WS (2019) Natriuretic peptides in chronic heart failure. Card Fail Rev 5(1):44–49. https://doi.org/10.15420/cfr.2018.26.1. [PMCfreearticle] [PubMed] [CrossRef] [GoogleScholar]
Zhang L, Han B, Liu H et al (2021) Circular RNA circACSL1 aggravated myocardial inflammation and myocardial injury by sponging miR-8055 and regulating MAPK14 expression. Cell Death Dis 12(5):487. https://doi.org/10.1038/s41419-021-03777-7. [PMCfreearticle] [PubMed] [CrossRef] [GoogleScholar]
Goetze JP, Christoffersen C, Perko M et al (2003) Increased cardiac BNP expression associated with myocardial ischemia. FASEB J 17(9):1105–1107. https://doi.org/10.1096/fj.02-0796fje. [PubMed] [CrossRef] [GoogleScholar]
Hao Y, Cheng F, Pham M et al (2019) A noninvasive, economical, and instant-result method to diagnose and monitor type 2 diabetes using pulse wave: case-control study. JMIR Mhealth Uhealth. 7(4):e11959. https://doi.org/10.2196/11959. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Guo R, Wang Y, Yan H et al (2015) Analysis and recognition of traditional Chinese medicine pulse based on the Hilbert-Huang transform and random forest in patients with coronary heart disease. Evid Based Complement Alternat Med 2015:895749. https://doi.org/10.1155/2015/895749. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Li FF, Sun R, Xue S et al (2015) Pulse signal analysis of patients with coronary heart diseases using Hilbert-Huang transformation and time-domain method. Chin J Integr Med 21(5):355–360. https://doi.org/10.1007/s11655-015-2173-7. [PubMed] [CrossRef] [GoogleScholar]
Qi Z, Zhao ZY, Xu JT et al (2020) Radial pulse wave signals combined with Ba-PWV for the risk prediction of hypertension and the monitoring of its accompanying metabolic risk factors. Evid Based Complement Alternat Med 29(2020):3926851. https://doi.org/10.1155/2020/3926851. [PMCfreearticle] [PubMed] [CrossRef] [GoogleScholar]
Guo R, Wang Y, Yan J, Yan H (2012) Recurrence quantification analysis on pulse morphological changes in patients with coronary heart disease. J Tradit Chin Med 32(4):571–577. https://doi.org/10.1016/s0254-6272(13)60073-4. [PubMed] [CrossRef] [GoogleScholar]
Willemink MJ, Varga-Szemes A, Schoepf UJ et al (2021) Emerging methods for the characterization of ischemic heart disease: ultrafast Doppler angiography, micro-CT, photon-counting CT, novel MRI and PET techniques, and artificial intelligence. Eur Radiol Exp 5(1):12. https://doi.org/10.1186/s41747-021-00207-3. [PMCfreearticle] [PubMed] [CrossRef] [GoogleScholar]
Tahvildari M, Singh RB, Saeed HN (2021) Application of Artificial Intelligence in the diagnosis and management of corneal diseases. Semin Ophthalmol 36(8):641–648. https://doi.org/10.1080/08820538.2021.1893763. [PubMed] [CrossRef] [Google Scholar]
Liberini V, Laudicella R, Balma M et al (2022) Radiomics and artificial intelligence in prostate cancer: new tools for molecular hybrid imaging and theragnostics. Eur Radiol Exp 6(1):27. https://doi.org/10.1186/s41747-022-00282-0. [PMCfreearticle] [PubMed] [CrossRef] [GoogleScholar]
Silver MA, Maisel A, Yancy CW, McCullough PA, Burnett JC Jr, Francis GS, Mehra MR, Peacock WF 4th, Fonarow G, Gibler WB, Morrow DA, Hollander J (2004) BNP Consensus Panel. BNP Consensus Panel 2004: A clinical approach for the diagnostic, prognostic, screening, treatment monitoring, and therapeutic roles of natriuretic peptides in cardiovascular diseases. Congest Heart Fail 10(5 Suppl 3):1–30. https://doi.org/10.1111/j.1527-5299.2004.03271.x. Erratum in: Congest Heart Fail. 2005 Mar-Apr;11(2):102. [PubMed] [CrossRef] [Google Scholar]
Yan J, Cai X, Chen S et al (2021) Ensemble learning-based pulse signal recognition: classification model development study. JMIR Med Inform 9(10):e28039. Published 2021 Oct 21. https://doi.org/10.2196/28039. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Costa M, Goldberger AL, Peng CK (2002) Multiscale entropy analysis of complex physiologic time series. Phys Rev Lett 89(6):068102. https://doi.org/10.1103/PhysRevLett.89.068102. [PubMed] [CrossRef] [Google Scholar]
Costa M, Goldberger AL, Peng CK (2005) Multiscale entropy analysis of biological signals. Phys Rev E Stat Nonlin Soft Matter Phys 71(2 Pt1):021906. https://doi.org/10.1103/PhysRevE.71.021906. [PubMed] [CrossRef] [Google Scholar]
Eroğlu G, Gürkan M, Teber S et al (2022) Changes in EEG complexity with neurofeedback and multi-sensory learning in children with dyslexia: a multiscale entropy analysis. Appl Neuropsychol Child 11(2):133–144. https://doi.org/10.1080/21622965.2020.1772794. [PubMed] [CrossRef] [Google Scholar]
Lee J, Guo Y, Ravikumar V, Tolkacheva EG (2020) Towards the development of nonlinear approaches to discriminate AF from NSR using a single-lead ECG. Entropy (Basel) 22(5):531. https://doi.org/10.3390/e22050531. [PMCfreearticle] [PubMed] [CrossRef] [GoogleScholar]
Kang HG, Dingwell JB (2016) Differential changes with age in multiscale entropy of electromyography signals from leg muscles during treadmill walking. PLoS One 11(8):e0162034. https://doi.org/10.1371/journal.pone.0162034. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Liau BY, Wu FL, Zhang K et al (2021) Using bidimensional multiscale entropy analysis of ultrasound images to assess the effect of various walking intensities on plantar soft tissues. Entropy (Basel) 23(3):264. https://doi.org/10.3390/e23030264. [PMCfreearticle] [PubMed] [CrossRef] [GoogleScholar]
Awan I, Aziz W, Shah IH et al (2018) Studying the dynamics of interbeat interval time series of healthy and congestive heart failure subjects using scale based symbolic entropy analysis. PLoS One 13(5):e0196823. https://doi.org/10.1371/journal.pone.0196823. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Busa MA, van Emmerik REA (2016) Multiscale entropy: a tool for understanding the complexity of postural control. J Sport Health Sci 5(1):44–51. https://doi.org/10.1016/j.jshs.2016.01.018. [PMCfreearticle] [PubMed] [CrossRef] [GoogleScholar]
Pandya R, Pandya J (2015) C5.0 algorithm to improved decision tree with feature selection and reduced error pruning. Int J Comput Appl 117:18–21. https://doi.org/10.5120/20639-3318. [CrossRef] [Google Scholar]
Dimitriadis SI, Liparas D (2018) Alzheimer’s disease neuroimaging initiative. How random is the random forest? Random forest algorithm on the service of structural imaging biomarkers for Alzheimer’s disease: from Alzheimer’s disease neuroimaging initiative (ADNI) database. Neural Regen Res 13(6):962–970. https://doi.org/10.4103/1673-5374.233433. [PMC free article] [PubMed] [CrossRef]
Fei ZF (2006) Modern pulse diagnosis in Chinese medicine, People’s Medical Publishing House, Beijin, China. pp 163–165
Fernandez A, Garcia S, Herrera F, Chawla NV (2018) SMOTE for Learning from imbalanced data: progress and challenges, marking the 15-year anniversary. J Artif Intell Res 61. https://doi.org/10.1613/jair.1.11192. [CrossRef]
Park D, Lee JH, Han S (2017) Underweight: another risk factor for cardiovascular disease?: A cross-sectional 2013 Behavioral Risk Factor Surveillance System (BRFSS) study of 491,773 individuals in the USA. Medicine (Baltimore) 96(48):e8769. https://doi.org/10.1097/MD.0000000000008769. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Hansen C, Wei Q, Shieh JS et al (2017) Sample entropy, univariate, and multivariate multi-scale entropy in comparison with classical postural sway parameters in young healthy adults. Front Hum Neurosci 26(11):206. https://doi.org/10.3389/fnhum.2017.00206. [PMCfreearticle] [PubMed] [CrossRef] [GoogleScholar]
Lipsitz LA, Goldberger AL (1992) Loss of ‘complexity’ and aging. Potential applications of fractals and chaos theory to senescence. JAMA 267(13):1806–9. [PubMed] [CrossRef] [Google Scholar]
Chen J, Li Q, Wang H, Deng M (2019) A Machine learning ensemble approach based on random forest and radial basis function neural network for risk evaluation of regional flood disaster: a case study of the Yangtze River Delta, China. Int J Environ Res Public Health 17(1):49. https://doi.org/10.3390/ijerph17010049. [PMCfreearticle] [PubMed] [CrossRef]
Acknowledgements
National Natural Science Foundation of China (No.82074332) and Shanghai Science and Technology Committee Funding (No.19441901100), and Shanghai Key Laboratory of Health Identification and Assessment (No. 21DZ2271000).
Author information
Authors and Affiliations
Contributions
Wen-jie Wu wrote the whole manuscript text, which was revised by Rui Guo, Yi-qin Wang, Hai-xia Yan, Ye-qing Zhang, and Rui Guo provided the idea and structure of this manuscript. Jian-jun Yan helped to analyze the data in the paper. Wen-jie Wu, Rui Chen, and Chun-ke Zhang collected and collated the data in the paper. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, Wj., Chen, R., Guo, R. et al. A novel method for assessing cardiac function in patients with coronary heart disease based on wrist pulse analysis. Ir J Med Sci 192, 2697–2706 (2023). https://doi.org/10.1007/s11845-023-03341-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-023-03341-6