Abstract
Background
Lipid disorders are now considered causal for atherosclerotic cardiovascular disease (ASCVD) which remains one of the most important contributors to morbidity and mortality in the developed world. Identification and early treatment of lipid disarrays remains the cornerstone of good clinical practice to prevent, halt and even reverse ASCVD. Guidelines for lipid management are imperative to help promote good clinical practice. Given the detail involved in comprehensive guidelines and the multiple areas of knowledge required by clinical practitioners, abbreviated, easy to understand, practical versions of guidelines are required to ensure dissemination of the most important information. The recent ESC lipid guidelines 2019 and the ESC guidelines on CVD prevention in clinical practice 2021 (1,2), provide an excellent detailed summary of all the latest evidence supporting lipid interventions that reduce ASCVD.
Method
We therefore developed a single-page document with hyperlinks to help practitioners gain easy access to practical information on lipid management. It has been developed for future electronic use in clinical practice.
Conclusion
It is presented here in a tabular format together with printable versions of the associated hyperlinks that provide the additional information required in decision making. It is hoped to audit the impact of this approach to help guide future ways of disseminating the latest clinical guideline updates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinical lipid guidelines based on the latest available information are developed by a panel of international experts [1, 2]. They make recommendations according to the type and level of evidence supporting or not the best course of action in various circumstances. Despite an enormous effort to develop guidelines, their translation into clinical practice is often slow or challenging [3,4,5,6]. Many with severe hypercholesterolaemia go undetected or inadequately treated [7]. In the modern era of sound bites and information overload, the practicing physician and nurse have only a limited time to comprehend and utilise guidelines. Previous studies highlight that general practitioners expressed frustration concerning the length and accessibility of guidelines [8]. Despite this, all practitioners hope to have the latest most appropriate information to deliver good clinical practice. In an effort to bridge this gap, many have requested a brief summary, or clinical pathways to help them treat lipid disorders particularly within primary care. The distillation of the extensive knowledge base in guidelines into practical recommendations that are clearly visualised, understood and easy to use requires the collective effort of lipid specialists. Some members of the Irish Lipid Network which incorporates specialists engaged in advanced lipid management in the Republic of Ireland volunteered to undertake this task. They formulated an easy-to-use comprehensive short document with links to appropriate associated information in a manner that could be used electronically in clinical practice. This guide was reviewed and approved by the Quality and Safety in Practice Committee of the Irish College of General Practitioners prior to submission to ensure ease of application in routine general practice.
Methods
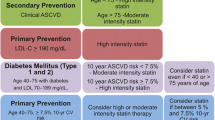
A number of members of the Irish Lipid Network were involved in the production of a document that could facilitate interpretation and management of lipid disorders in Ireland. Those involved in specialist lipid clinics are already familiar with the various aspects of lipid guidelines. As a consequence, the focus was on how to produce a short document for the larger body of practitioners particularly those in primary care, to help them manage lipid disorders when time is limited and detailed study is not possible. The specialists who participated included cardiologists, chemical pathologists, endocrinologists, clinical pharmacologists, general practitioners, nurses and scientists. Given the need to widely disseminate lipid management information, general practice was involved from the outset in this process to help guide the appropriate direction undertaken [9]. Following preliminary meetings of a core group of interested parties, a working document was produced. A single paged document (Fig. 1) that could be viewed electronically and easily incorporated into practice computer desk tops was deemed the preferred option. Careful consideration was given to highlight key elements such as the need for abbreviated guidelines, who and how to test, risk groups and target lipid levels, practical steps and suggested lipid-lowering drugs and dosages required to achieve lipid targets. An explanatory page (Fig. 2) was also produced to help guide interpretation when needed. A number of hyperlink materials were also developed to help familiarise practitioners with information that would enhance their understanding of the basis for intervention and need for further screening as deemed necessary [10,11,12,13,14,15].
Data tables and hyperlinks
Figure 1 outlines the summarised abbreviated guidelines that will be viewed on a computer desktop. It includes colourised sections to make interpretation easier. Explanatory notes to assist in the interpretation of the abbreviated guidelines are presented in Fig. 2. Risk factors are grouped into moderate, high and very high–risk categories (Fig. 3) using a calculated score from the SCORE 2 and SCORE 2 Older person (OP) charts (2). These charts are used for apparently healthy people living in a moderate CVD risk country (Ireland).
Figure 4 Lipid management algorithm for raised LDL cholesterol levels.
Figure 5 is a flow sheet highlighting the recommended treatment algorithms for those patients with atherogenic dyslipidaemia, and Fig. 6 highlights potential treatment strategies for those with severe hypertriglyceridaemia who are at risk of pancreatitis.
Supplementary information, accessible via hyperlinks from the desktop electronic version of these abbreviated guidelines, is outlined in the appendix as either hyperlink addresses or tables.
These include hyperlink addresses to calculators for Q RISK [10], SCORE 2 and SCORE 2 OP (Ireland moderate risk country) [2] and the Dutch lipid network scoring system (Fig. 7) [11]. The Dutch Lipid Clinic Network score (DCLNS) is a tool intended to support physicians in the diagnosis of heterozygous familial hypercholesterolaemia (FH) in adults. Suggested actions regarding myopathy [12, 13] are revealed in Fig. 8. Drugs that cause hyperlipidaemia [14] are outlined in Table 1. Drugs that interact with statins are outlined in Table 2.
The diet and lifestyle are shown in Tables 3 and 4 [1] and are also included in the appendices and contain the latest evidenced-based guidelines from the ESC Dyslipidaemia Guidelines 2019.
Having electronic versions of these guidelines and associated materials provides a buildable platform which will enable continuous updates as new information and evidence arises.
Discussion
The extent of lipid problems in Ireland is significant, and lipid management [4, 6] and lipid services are inadequate [15, 16]. The significance of untreated lipid disorders on population health cannot be overestimated [17, 18], and early interventions could have far-reaching consequences on Irish lives and health care resource utilisation. Furthermore, evidence from our older population in Ireland also highlights inadequate treatment of cholesterol problems once diagnosed [19]. Following detection, lowering of LDL cholesterol levels to very low levels yields a 22% cardiovascular risk reduction for each mmol/l LDLc reduction using statins. Additionally, lowering of non-HDLc levels in those with moderately elevated triglycerides further reduces cardiovascular risks [20]. Treatment of those with severe hypertriglyceridaemia markedly reduces the risk of pancreatitis [21].
It is unacceptable that any individual has undetected serious lipid problems which are causing accelerated ASCVD or pancreatitis. As a consequence, when it comes to lipid disorders “What you don’t know may hurt you!”. Therefore, familiarisation of lipid management in primary care will facilitate more individuals being screened and more severe genetic disorders being identified earlier [22, 23]. The objective of these abbreviated guidelines is to facilitate greater understanding by distilling the most pertinent, useable information from the ESC lipid management guidelines (2019) and the ESC Cardiovascular prevention in clinical practice guidelines (2021) related to lipid disorders. Although shortened versions are likely to eliminate a lot of explanatory information that enhances understanding and management, this approach allows interventions to be undertaken quickly in a reassuring manner without the need for further detailed study. For those who wish to glean further information, appropriate links are provided to help in this regard. Since all of this information will be presented electronically on computer desktops, updates and additional information can easily be added. Auditing the use of this abbreviated lipid management tool will facilitate a better understanding of what really matters to practitioners.
As the format of limiting the information to a single page has been widely used in primary care for other conditions, it is likely that this approach to lipid management will also be useful. Endorsement by a group of specialists who are usually the main referral group for lipid management in Ireland may also help utilisation of these modified guidelines. Like all new ventures, only time will tell if this approach is valuable. Certainly, presentation of preliminary versions of these guidelines was widely accepted by general practitioners and endorsed by the Irish College of General Practitioners.
Dissemination of this information and provision of appropriate software versions of these documents for incorporation on computer desk tops will require support. Ideally, monies needed for dissemination of this information should come from various sources to help maintain and expand the development of this tool. Independence from bias on any information provided needs to be ensured in order to engage the trust of practitioners on the validity of this approach long term.
Finally, guidelines are only guidelines, and they will afford practitioners with some of the information required to help their patients. It is likely that these abbreviated guidelines will require associated educational support in order to familiarise practitioners on how to use them and also to gain feedback on their utility. It is envisioned that educational meetings, videos and short practice guidelines will be provided. As a result of increased awareness and interventions, there will also be increasing numbers of patients that need specialist lipid management. In this regard, development of guidelines needs to be followed by the necessary provision of appropriately resourced specialist lipid centres if a seamless optimal lipid management service is to be provided nationally.
Data availability
Data is available in referenced guidelines.
References
Mach F et al (2019) ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Atherosclerosis 290:140–205. https://doi.org/10.1016/j.atherosclerosis.2019.08.014. (Epub 2019 8 31; PMID: 31591002)
Visseren FLJ et al (2021) ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 42:3227–3337. https://doi.org/10.1093/eurheartj/ehab484
De Backer G, Jankowski P, Kotseva K et al (2019) Management of dyslipidaemia in patients with coronary heart disease: results from the ESC-EORP EUROASPIRE V survey in 27 countries. Atherosclerosis 285:135–146. https://doi.org/10.1016/j.atherosclerosis.2019.03.014. (Epub 2019 Apr 24; PMID: 31054483)
Dunne M, Mac Ananey O, Markham C, Maher V (2013) Lipid targets in clinical practice: successes, failures and lessons to be learned. Ir J Med Sci. https://doi.org/10.1007/s11845-013-0954-6
Ray KK, Molemans B, Schoonen WM et al (2021) EU-wide cross-sectional observational study of lipid-modifying therapy use in secondary and primary care: the DAVINCI study. Eur J Prev Cardiol 28(11):1279–1289. https://doi.org/10.1093/eurjpc/zwaa047
Offiah G, O’Connor C, Kennedy C et al (2022) The DA VINCI study: is Ireland achieving ESC/EAS guideline–directed LDL-C goals? Ir J Med Sci. https://doi.org/10.1007/s11845-022-03050-6
Vallejo-Vaz AJ et al (2021) A global perspective of familial hypercholesterolaemia: a cross-sectional study from the EAS Familial Hypercholesterolaemia Studies Collaboration (FHSC). The Lancet 398(10312). https://doi.org/10.1016/S0140-6736(21)01122-3
Austad B, Hetlevik I, Mjølstad BP, Helvik A-S (2015) General practitioners’ experiences with multiple clinical guidelines: a qualitative study from Norway. Qual Prim Care 23(2):70–77
Fitzpatrick P, Fitzsimon N, Lonergan M et al (2011) Heartwatch: the effect of a primary care-delivered secondary prevention programme for cardiovascular disease on medication use and risk factor profiles. Eur J Prev Cardiol 18(1):129–136
Hippisley-Cox J, Coupland C, Brindle P et al (2017) Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ 357. https://doi.org/10.1136/bmj.j2099. (Published 23 May 2017) Q risk 3. https://qrisk.org/three/
Defesche JC, Lansberg PJ, Umans-Eckenhausen MA, Kastelein JJ (2004) Advanced method for the identification of patients with inherited hypercholesterolemia. Dutch Lipid Clinic Network Score (DLCNS): Semin Vasc Med 4(1):59–65. PMID: 15199434. https://doi.org/10.1055/s-2004-822987
Wiklund O, Pirazzi C, Romeo S et al (2013) Monitoring of lipids, enzymes, and creatine kinase in patients on lipid-lowering drug therapy. Curr Cardiol Rep 15:397
Egan A, Colman E (2011) Weighing the benefits of high-dose simvastatin against the risk of myopathy. N Engl J Med 365(285287):258
Herink M, Ito MK. Drug induced hyperlipidaemia. https://www.ncbi.nlm.nih.gov/books/NBK326739/
Agar R, Markham C, Prendergast M et al (2017) A snapshot of lipid levels in the Republic of Ireland in. Ir J Med Sci 2018:1–7
Agar R, Prendergast M, Maher V et al (2020) Evaluation of lipid services in the Republic of Ireland. Ir J Med Sci 189:925–931. https://doi.org/10.1007/s11845-020-02187-
Ference BA, Ginsberg HN, Graham I et al (2017) Low-density lipoproteins cause atherosclerotic cardiovascular disease. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. https://doi.org/10.1093/eurheartj/ehx144
McQueen MJ, Hawken S, Wang X et al (2008) INTERHEART study investigators Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): a case-control study. Lancet 372(9634):224–233
Murphy C, Shelley E, O’Halloran AM, Fahey T, Kenny RA (2017) Failure to control hypercholesterol-aemia in the Irish adult population: cross-sectional analysis of the baseline wave of The Irish Longitudinal Study on Ageing (TILDA). Ir J Med Sci. https://doi.org/10.1007/s11845-017-1590-3
Bhatt DL, Steg PG, Miller M et al (2019) cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia REDUCE-IT Investigators. N Engl J Med 380(1):11–22. https://doi.org/10.1056/NEJMoa1812792. (Epub 2018 Nov 10)
Toskes PP (1990) Hyperlipidaemic pancreatitis. Gastroenterol Clin N Am 19(4):783
O’Kane MJ, Menown IB, Graham I et al (2012) The detection of heterozygous familial hypercholesterolemia in Ireland. Adv Ther 29(5):456–63. https://doi.org/10.1007/s12325-012-0021-0
Arnold-Reed DE, Brett T, Troeung L et al (2017) Detection and management of familial hypercholesterolaemia in primary care in Australia: protocol for a pragmatic cluster intervention study with pre-post intervention comparisons. BMJ Open 7(10). https://doi.org/10.1136/bmjopen-2017-017539. PMID : 29061621
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This was a review of current guidelines and did not involve participants human or animal. Informed consent was not required as no intervention or data collection were performed. All guidelines used were referenced accordingly.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maher, V., Gallagher, J., Agar, R. et al. Abbreviated lipid guidelines for clinical practice. Ir J Med Sci 192, 2151–2157 (2023). https://doi.org/10.1007/s11845-023-03277-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-023-03277-x