Abstract
Purpose of Review
Low-density lipoprotein cholesterol (LDL-C) is the most important causal risk factor for atherosclerotic cardiovascular disease (ASCVD). This article reviews why LDL-C remains overlooked and underestimated despite numerous studies that have proved its role.
Recent Findings
Recently published EAS/ESC Guidelines for dyslipidemia and EAS Guidelines for prevention set new targets for LDL-C levels in primary and secondary prevention of ASCVD. These guidelines are based on data from large studies and meta-analyzes that have shown that lower LDL-C also means lower cardiovascular event rates. Real-life experience published in registries worldwide has shown us that the guidelines have not been translated to everyday clinical practice, meaning that a significant number of patients are undertreated and have LDL-C levels well above target. Potential reasons for the abovementioned are poor adherence and education of the patient and physician and health care system related factors.
Summary
Implementation of the latest version of guidelines will require continuous patient and physicians education, as well as a shared decision-making process between physician and patient.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kuijpers PMJC. History in medicine: the story of cholesterol, lipids and cardiology. e-J Cardiol Pract: Eur Soc Cardiol. 2021;19. Available from: https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-19/history-in-medicine-the-story-of-cholesterol-lipids-and-cardiology.
Siri-Tarino PW, Krauss RM. The early years of lipoprotein research: from discovery to clinical application. J Lipid Res. 2016;57(10):1771–7.
Češka R. Familiární hypercholesterolemie. Prague: Triton; 2015.
Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38(32):2459–72.
Libby P, Buring JE, Badimon L, Hansson GK, Deanfield J, Bittencourt MS, et al. Atherosclerosis Nature reviews Disease primers 2019;5(1):56.
Goldstein JL, Brown MS. A century of cholesterol and coronaries: from plaques to genes to statins. Cell. 2015;161(1):161–72.
Bergheanu SC, Bodde MC, Jukema JW. Pathophysiology and treatment of atherosclerosis: Current view and future perspective on lipoprotein modification treatment. Neth Hear J. 2017;25(4):231–42.
Brensike JF, Levy RI, Kelsey SF, Passamani ER, Richardson JM, Loh IK, et al. Effects of therapy with cholestyramine on progression of coronary arteriosclerosis: results of the NHLBI Type II Coronary Intervention Study. Circulation. 1984;69(2):313–24.
Frick MH, Elo O, Haapa K, Heinonen OP, Heinsalmi P, Helo P, et al. Helsinki Heart Study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia. Safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med. 1987;317(20):1237–45.
Frick MH, Elo O, Haapa K, Heinonen OP, Heinsalmi P, Helo P, et al. Helsinki Heart Study: Primary-Prevention Trial with Gemfibrozil in Middle-Aged Men with Dyslipidemia. 1987;317(20):1237-45.
Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet (London, England). 1994;344(8934):1383-9.
Cheung BM, Lauder IJ, Lau CP, Kumana CR. Meta-analysis of large randomized controlled trials to evaluate the impact of statins on cardiovascular outcomes. Br J Clin Pharmacol. 2004;57(5):640–51.
Fulcher J, O'Connell R, Voysey M, Emberson J, Blackwell L, Mihaylova B, et al. Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials. Lancet (London, England). 2015;385(9976):1397–405.
Stroes E. Statins and LDL-cholesterol lowering: an overview. Curr Med Res Opin. 2005;21(Suppl 6):S9–16.
Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372(25):2387–97.
Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376(18):1713–22.
Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379(22):2097–107.
Ridker PM, Revkin J, Amarenco P, Brunell R, Curto M, Civeira F, et al. Cardiovascular efficacy and safety of bococizumab in high-risk patients. N Engl J Med. 2017;376(16):1527–39.
•• 2019 ESC/EAS. Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Atherosclerosis. 2019;290:140–205 2019 ESC/EAS guidelines are based on clinica trials which have shown that LDL-C is causally related to ASCVD, and that lower LDL-C value means the lower risk of future CV events. Guidelines recommended new LDL-C goals in primary and secondary prevention as well as therapeutic strategy on how to acchieve it.
Češka R, Paragh G, Reiner Ž, Banach M, Tokgözoğlu L, Susekov AV, et al. ScreenPro FH - screening project for familial hypercholesterolemia in central, southern and eastern Europe: rationale and design. Vnitr Lek. 2017;63(1):43–8.
Češka R, Freiberger T, Susekov AV, Paragh G, Reiner Ž, Tokgözoğlu L, et al. ScreenPro FH - screening project for familial hypercholesterolemia in central, southern and eastern Europe: basic epidemiology. Vnitr Lek. 2017;63(1):25–30.
Vallejo-Vaz AJ, De Marco M, Stevens CAT, Akram A, Freiberger T, Hovingh GK, et al. Overview of the current status of familial hypercholesterolaemia care in over 60 countries - The EAS Familial Hypercholesterolaemia Studies Collaboration (FHSC). Atherosclerosis. 2018;277:234–55.
Global perspective of familial hypercholesterolaemia. A cross-sectional study from the EAS Familial Hypercholesterolaemia Studies Collaboration (FHSC). Lancet (London, England). 2021;398(10312):1713–25.
Cuchel M, Bruckert E, Ginsberg HN, Raal FJ, Santos RD, Hegele RA, et al. Homozygous familial hypercholesterolaemia: new insights and guidance for clinicians to improve detection and clinical management. A position paper from the Consensus Panel on Familial Hypercholesterolaemia of the European Atherosclerosis Society. Eur Heart J. 2014;35(32):2146–57.
Katzmann JL, Gouni-Berthold I, Laufs U. PCSK9 Inhibition: insights from clinical trials and future prospects. Front Physiol. 2020;11:595819.
Charles R. Scriver WSS, Childs B, Beaudet AL, Valle D, Kinzler KW, Bert Vogelstein. The metabolic and molecular bases of inherited disease. 8 ed: McGraw-Hill Medical; 2018.
Kolansky DM, Cuchel M, Clark BJ, Paridon S, McCrindle BW, Wiegers SE, et al. Longitudinal evaluation and assessment of cardiovascular disease in patients with homozygous familial hypercholesterolemia. Am J Cardiol. 2008;102(11):1438–43.
Kosmas CE, Muñoz Estrella A, Skavdis A, Peña Genao E, Martinez I, Guzman E. Inclisiran for the treatment of cardiovascular disease: a short review on the emerging data and therapeutic potential. Ther Clin Risk Manag. 2020;16:1031–7.
Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet (London, England). 2005;366(9493):1267–78.
Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38(32):2459–72.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88.
Arnold SV, de Lemos JA, Liu Y, Mues KE, Bhatt DL, Cannon CP, et al. Adherence to guideline medication recommendations to prevent atherosclerotic cardiovascular disease progression among adults with prior myocardial infarction. JAMA Netw Open. 2020;3(4):e203032.
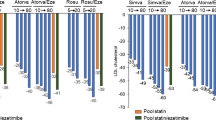
• Ray KK, Molemans B, Schoonen WM, Giovas P, Bray S, Kiru G, et al. EU-wide cross-sectional observational study of lipid-modifying therapy use in secondary and primary care: the DA VINCI study. Eur J Prev Cardiol. 2021;28(11):1279–89. Findings from this study suggest that fewer than half of high/very high-risk primary and secondary prevention patients achieved guideline recommended LDL-C goals.
Kristensen MS, Green A, Nybo M, Hede SM, Mikkelsen KH, Gislason G, et al. Lipid-lowering therapy and low-density lipoprotein cholesterol goal attainment after acute coronary syndrome: a Danish population-based cohort study. BMC Cardiovasc Disord. 2020;20(1):336.
Nishikido T, Ray KK. The power of lipid registries for cardiovascular disease prevention. Curr Opin Lipidol. 2021;32(6):342–8.
Virani SS, Kennedy KF, Akeroyd JM, Morris PB, Bittner VA, Masoudi FA, et al. Variation in lipid-lowering therapy use in patients with low-density lipoprotein cholesterol ≥190 mg/dL: insights from the National Cardiovascular Data Registry-Practice Innovation and Clinical Excellence Registry. Circulation Cardiovasc Qual outcomes. 2018;11(5):e004652.
Barrios V, Soronen J, Carter AM, Anastassopoulou A. Lipid management across Europe in the real-world setting: a rapid evidence review. Curr Med Res Opin. 2021;37(12):2049–59.
Bates TR, Connaughton VM, Watts GF. Non-adherence to statin therapy: a major challenge for preventive cardiology. Expert Opin Pharmacother. 2009;10(18):2973–85.
Arnold SV, Cannon CP, de Lemos JA, Rosenson RS, Ballantyne CM, Liu Y, et al. What do US physicians and patients think about lipid-lowering therapy and goals of treatment? Results From the GOULD Registry. J Am Heart Assoc. 2021;10(16):e020893.
Waßmuth S, Rohe K, Noack F, Noutsias M, Treede H, Schlitt A. Adherence to lipid-lowering therapy in patients with coronary heart disease from the state Of Saxony-Anhalt, Germany. Vasc Health Risk Manage. 2019;15:477–83.
• Schiele F, Quignot N, Khachatryan A, Gusto G, Villa G, Kahangire D, et al. Clinical impact and room for improvement of intensity and adherence to lipid lowering therapy: Five years of clinical follow-up from 164,565 post-myocardial infarction patients. Int J Cardiol. 2021;332:22–8. This study showed that among patients with a history of MI, prescription of high-intensity LLT were limited and adherence to LLT was low. Higher-intensity LLT and/or adherence to statins was associated with significantly lower risk of MACE.
De Bacquer D, Astin F, Kotseva K, Pogosova N, De Smedt D, De Backer G, et al. Poor adherence to lifestyle recommendations in patients with coronary heart disease: results from the EUROASPIRE surveys. Eur J Prev Cardiol. 2021.
Penson PE, Banach M. Nocebo/drucebo effect in statin-intolerant patients: an attempt at recommendations. Eur Heart J. 2021;42(47):4787–8.
Wood FA, Howard JP, Finegold JA, Nowbar AN, Thompson DM, Arnold AD, et al. N-of-1 trial of a statin, placebo, or no treatment to assess side effects. N Engl J Med. 2020;383(22):2182–4.
Barter PJ, Yamashita S, Laufs U, Ruiz AJ, Sy R, Fang MDG, et al. Gaps in beliefs and practice in dyslipidaemia management in Japan, Germany, Colombia and the Philippines: insights from a web-based physician survey. Lipids Health Dis. 2020;19(1):131.
Vashitz G, Meyer J, Parmet Y, Henkin Y, Peleg R, Gilutz H. Physician adherence to the dyslipidemia guidelines is as challenging an issue as patient adherence. Fam Pract. 2011;28(5):524–31.
De Backer G, Jankowski P, Kotseva K, Mirrakhimov E, Reiner Ž, Rydén L, et al. Management of dyslipidaemia in patients with coronary heart disease: results from the ESC-EORP EUROASPIRE V survey in 27 countries. Atherosclerosis. 2019;285:135–46.
Kolandaivelu K, Leiden BB, O'Gara PT, Bhatt DL. Non-adherence to cardiovascular medications. Eur Heart J. 2014;35(46):3267–76.
Chia LR, Schlenk EA, Dunbar-Jacob J. Effect of personal and cultural beliefs on medication adherence in the elderly. Drugs Aging. 2006;23(3):191–202.
Ellis JJ, Erickson SR, Stevenson JG, Bernstein SJ, Stiles RA, Fendrick AM. Suboptimal statin adherence and discontinuation in primary and secondary prevention populations. J Gen Intern Med. 2004;19(6):638–45.
Helin-Salmivaara A, Korhonen MJ, Alanen T, Huupponen R. Impact of out-of-pocket expenses on discontinuation of statin therapy: a cohort study in Finland. J Clin Pharm Ther. 2012;37(1):58–64.
Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. Jama. 2002;287(3):337–44.
Rouhi-Boroujeni H, Rouhi-Boroujeni H, Heidarian E, Mohammadizadeh F, Rafieian-Kopaei M. Herbs with anti-lipid effects and their interactions with statins as a chemical anti- hyperlipidemia group drugs: a systematic review. ARYA Atheroscler. 2015;11(4):244–51.
Ahmed ST, Akeroyd JM, Mahtta D, Street R, Slagle J, Navar AM, et al. Shared decisions: a qualitative study on clinician and patient perspectives on statin therapy and statin-associated side effects. J Am Heart Assoc. 2020;9(22):e017915.
Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–14.
Souliotis K, Agapidaki E, Peppou LE, Tzavara C, Varvaras D, Buonomo OC, et al. Assessing patient organization participation in health policy: a comparative study in France and Italy. Int J Health Policy Manag. 2018;7(1):48–58.
Jones LK, McMinn M, Kann D, Lesko M, Sturm AC, Walters N, et al. Evaluation of a multidisciplinary lipid clinic to improve the care of individuals with severe lipid conditions: a RE-AIM framework analysis. Implement Sci Commun. 2021;2(1):32.
Alieva AS, Tokgözoğlu L, Ray KK, Catapano AL. Lipid Clinics Network. Rationale and design of the EAS global project. Atheroscler Suppl. 2020;42:e6–8.
Endo A. A historical perspective on the discovery of statins. Proc Japan Acad Series B, Phys Biol Sci. 2010;86(5):484–93.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Lamija Ferhatbegović reports payment or honoraria from KRKA FARMA d.o.o. Sarajevo, Bayer Pharma Sarajevo, Novartis Pharma Services Inc., and Servier. They also report support for attending meetings and/or travel from Farmavita Sarajevo and KRKA FARMA d.o.o. Sarajevo.
Denis Mršić reports payment or honoraria from Bosnalijek d.d Sarajevo.
Sabina Kušljugić has nothing to disclose.
Belma Pojskić reports payment or honoraria from KRKA FARMA d.o.o. Sarajevo, Lek d.d. Ljubljana, Novartis Pharma Services Inc., and Farmavita Sarajevo. They also report support for attending meetings and/or travel from Farmavita Sarajevo. And they report participation on a Data Safety Monitoring Board or Advisory Board for Novartis and Sanofi.
Human and Animal Rights and Informed Consent
This article is a review article in the field of low-density lipoprotein cholesterol and atherosclerotic cardiovascular disease. It contains previous publications based on human and animal studies.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Statin Drugs
Rights and permissions
About this article
Cite this article
Ferhatbegović, L., Mršić, D., Kušljugić, S. et al. LDL-C: The Only Causal Risk Factor for ASCVD. Why Is It Still Overlooked and Underestimated?. Curr Atheroscler Rep 24, 635–642 (2022). https://doi.org/10.1007/s11883-022-01037-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11883-022-01037-3