Abstract
Background
Hypercholesterolaemia is an important modifiable risk factor for cardiovascular disease (CVD) which requires monitoring and management at a population level.
Aims
This study aims to describe the distribution of serum cholesterol in a community living population of older adults in Ireland and to examine the awareness, treatment and control of hypercholesterolaemia according to CVD risk status.
Method
This is a cross-sectional study in a nationally representative sample of adults aged 50–79 years (n = 5287). Hypercholesterolaemia was defined as low-density lipoprotein cholesterol (LDL-C) in excess of the recommended CVD risk category target and/or on lipid-lowering medication.
Results
This study reports a mean total cholesterol (TC) of 5.1 mmol/L (95% CI 5.0–5.1 mmol/L) and a mean LDL-C of 2.9 mmol/L (95% CI 2.8–2.9 mmol/L) in those aged 50–79 years. In a subgroup aged 50–64 years, 73% (95% CI 71.5–74.5%) were hypercholesterolaemic. LDL-C was controlled to the guideline target in 57% of those with CVD and 49% of those with diabetes. Lack of awareness of hypercholesterolaemia was high across the remainder of the population.
Conclusion
Despite a substantial reduction in population mean TC from a high of 6.0 mmol/L in the 1980s to 5.1 mmol/L, this study reports a failure to control hypercholesterolaemia to recommended risk-stratified targets in the Irish adult population. Recommendations for policy include continued monitoring of those at highest risk and CVD risk assessment in those perceived to be at low risk in order to inform shared decision making in relation to lifestyle modification and medication management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although cardiovascular disease is the leading cause of mortality globally [1] and the leading cause of mortality in Ireland accounting for almost a third of all deaths [2], nonetheless, between 1985 and 2006, coronary heart disease mortality decreased by 68% in men and 69% in women [3]. Almost half of the reduction was attributed to improvements in risk factor levels; 24% was attributed to a reduction in population cholesterol levels [3].
Raised serum cholesterol is an important modifiable risk factor for the development of cardiovascular disease. A reduction in total cholesterol of 1 mmol/L is associated with a 33% reduction in ischaemic heart disease mortality in those aged 50–69 years and a reduction of 17% in those aged 70–89 years [4]. At a population level, total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol (HDL-C) are assessed to characterise abnormal cholesterol levels [5, 6]. Globally mean TC declined by 0.1 mmol/L between 1980 and 2008 with higher income regions including western Europe declining by 0.2 mmol/L for both sexes [7]. Despite an overall downward trend, a reversal of this trend at population level has recently been observed in Sweden between 2008 and 2010 [8].
Reliable population based data are required in order to monitor the management of hypercholesterolaemia, provide evidence for policy and evaluate cardiovascular disease programmes at a national level. The Irish Longitudinal Study on Ageing (TILDA) provides the opportunity to bridge this information gap.
Clinical guidelines on cholesterol reduction are based on overall CVD risk and not on the absolute level of cholesterol with targets identified according to absolute risk status. The aim of this study is to document the distribution of serum cholesterol in a community living population of older adults aged 50–79 years in Ireland and apply clinical guideline targets [9] to examine the awareness, treatment and control of hypercholesterolaemia in a subgroup aged 50–64 years according to their absolute risk of CVD.
Methods
Sample design
The Irish Longitudinal Study on Ageing (TILDA) is an ongoing prospective cohort study representative of community living adults in Ireland aged 50 years and older. The sample was recruited based on a national directory of residential addresses using the RANSAM system [10]. Participants were invited to take part in a home-based interview followed by a health assessment conducted by a research nurse in a designated centre or at home. The study uses cross-sectional data from the baseline wave (October 2009 to July 2011). Analyses are based on those aged 50–79 years at baseline who participated in the health assessment and provided a blood sample (n = 5287).
European Society of Cardiology guidelines and CVD risk
The European Society of Cardiology guidelines current during the data collection period recommended TC and LDL-C targets based on absolute CVD risk [9]. The Systematic COronary Risk Estimation (SCORE) based on a European cohort, estimates the 10-year risk of first fatal atherosclerotic event in asymptomatic individuals up to the age of 64 years based on five risk factors: age, sex, systolic blood pressure, total cholesterol and smoking status [11]. Ireland was classified as a “low risk” country based on CVD and diabetes mortality in 2008, therefore the corresponding risk equations were applied to the TILDA data. Individuals in the sub group (50–64 years) already known to be at high risk for CVD i.e. those with known CVD or diabetes were not classified using SCORE. The remaining participants were classified into one of four CVD risk categories; Very high risk (SCORE ≥10%), High risk (SCORE ≥5 and <10%), moderate risk (SCORE ≥1 and <5%) and low risk (SCORE <1%).
Lipid measurements
Non fasting venous blood was drawn during the health assessment. The TILDA protocol for blood sample collection, processing and storage has been described previously [12]. Briefly, 5 mL of fresh whole blood was collected in Lithium heparin coated tubes and transported to a central processing laboratory in temperature-controlled shipping boxes which maintained the samples at 2–8 °C for up to 48 h. Plasma samples were then isolated in 1 ml aliquots and placed at 2–8 °C for up to 72 h prior to lipid profile analysis. Lipid concentrations were analysed using Siemans Dimension Xpand chemistry analyser.
Total cholesterol was measured using a single reagent, endpoint reaction method that is specific for cholesterol. The assay is optimised against the Centres for Disease Control and Prevention (CDC) and the National Institute of Standards and Technology (NIST) reference methods. The method is standardised against the Abell/Kendall method and isotope dilution/mass spectrometry. The assay met the 1992 National Institutes of Health goal for precision and bias. LDL-C was calculated using the Friedewald formula. LDL-C is underestimated at higher triglyceride concentrations, therefore LDL-C was only calculated on participants with triglyceride values <4.0 mmol/L [13]. A direct determination of high-density lipoprotein cholesterol (HDL-C) was performed using PEG-modified enzymes and dextran sulphate. The Roche HDL-C assay meets the 1998 National Institutes of Health/National Cholesterol Program (NCEP) for acceptable performance. The results of this method correlate with those obtained by precipitation-based methods and also by ultracentrifugation. The method has been standardised against the designated CDC reference method. The standardisation meets the requirements of the “HDL-Cholesterol Method Evaluation Protocol for Manufacturers” of the US National Reference System for Cholesterol, CRMLN (Cholesterol Reference Method Laboratory Network), 1994.
In the subgroup aged 50–64, hypercholesterolaemia was defined as a LDL-C in excess of the risk category target as outlined in the guidelines (Table 3) and/or on lipid-lowering medication. Control of hypercholesterolaemia was defined as LDL-C below the guideline target in conjunction with the use of lipid-lowering medication.
Measurements
Demographic and social characteristics considered in this analysis include age, sex and highest educational attainment (primary, secondary and tertiary). Lipid-lowering medication use was recorded during the home interview. Medication was classified according to the WHO anatomical therapeutic chemical classification system (ATC), all medications coded C10 were included. Good agreement has been demonstrated in this cohort between lipid-lowering medication recorded at interview and pharmacy dispensing records (k = 0.73, 95% CI 0.69–0.77) [14].
Cardiovascular disease (angina, myocardial infarction, heart failure, stroke, transient ischaemic attack, stent/vascular surgery), diabetes and high cholesterol were self-reported based on ever having a doctor’s diagnosis of these conditions. Respondents were also asked if they had ever had a blood test for cholesterol.
Physical activity was self-assessed using the International Physical Activity Questionnaire (IPAQ) short form and categorised into low, moderate or high levels of physical activity [15]. Blood pressure was measured twice during the health assessment and the mean systolic and diastolic blood pressure recorded. Smoking status was self-reported during the home interview. Three mutually exclusive medical insurance categories were used, these include those with (a) a medical card which provides free access to primary care and subsidised medication (b) private health insurance only and (c) no health insurance.
Statistical analysis
Descriptive statistics are presented at percentages, means and standard deviations. Statistical significance was calculated using t tests for continuous variables and Chi-squared tests for categorical variables and set at p < 0.05. Statistical weights were applied to the sample to adjust for selection bias and non-response to the health assessment component of the survey. Individual weights were calibrated against the age, sex and educational profile of the Irish population sourced from the Quarterly National Household Survey 2010 compiled by the Irish Central Statistics Office. The subgroup analysis is unweighted. Statistical analysis was performed using the TILDA wave 1 data file v1-7-8 and statistical software Stata/MP V.12.1
Results
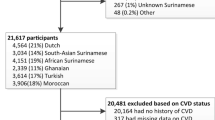
The household response rate to the baseline TILDA survey was 62%. Of the 8175 adults who participated in the TILDA study, 7537 were aged between 50 and 79 years. Of these, 70.1% (n = 5287) took part in the health assessment, had complete risk factor data available and were included in the analysis. The included participants were younger; more highly educated and displayed more favourable cardiovascular risk characteristics when compared to those not included in the analysis e.g. smoking (Table 1).
Total cholesterol, LDL cholesterol and HDL cholesterol
The weighted mean TC, LDL-C and HDL-C in the population aged 50–79 years are detailed in Table 2. Figure 1 graphically depicts the weighted mean TC, LDL-C and HDL-C according to sex and 5 year age group and shows a decline with advancing years more marked in men than in women for TC and LDL-C, whereas HDL-C remained unchanged with age.
LLM was used by 33.9% (95% CI 32.3–35.4%) of the sample. This proportion varied significantly across medical insurance categories. A higher proportion of those with a medical card (42.1%, 95% CI 39.7–44.5%) were on LLM compared to 28.4% (95% CI 26.3–30.4%) of those with private insurance only and 22.5% (95% CI 18.8–26.1%) of those with no medical insurance. This difference persisted after adjustment for age, sex and educational status. In those not taking LLM, the weighted mean TC was 5.3 mmol/L (95% CI 5.3–5.4), 5.1 mmol/L (95% CI 5.1–5.2) in men and 5.5 mmol/L (95% CI 5.5–5.6) in women (Table 2). In this group (not on LLM) the weighted mean TC and LDL-C peaked in men aged 55–59 years and in women aged 60–64 years (Fig. 2).
A high proportion of participants 88.9% (95% CI 87.8–89.9%) reported ever having a blood test for cholesterol. This proportion varied significantly with age from 82.6% (95% CI 80.1–85.1%) in the 50-54 year age group to 94.4% (95% CI 91.8–96.9%) in the 75–79 year age group. Equal proportions of men and women self-reported a blood test for cholesterol. In total, 41.1% (95% CI 39.6–42.7%) reported ever having a doctor’s diagnosis of high cholesterol.
Almost half of the population aged 50–79 years (44.8%, 95% CI 43.3–46.3%) had a TC <5 mmol/L and just over half (51.3%, 95% CI 49.8–52.8%) had an LDL-C <3 mmol/L. Only 22.3% (95% CI 21.1–23.5%) had a TC <5 mmol/L and were not on LLM, and 26.6% (95% CI 25.3–27.9%) had an LDL-C <3 mmol/L and were not on LLM.
Hypercholesterolaemia according to CVD risk status
A subgroup analysis was conducted on those aged 50–64 years, in whom absolute risk based on SCORE or morbidity status could reliably be calculated (n = 3227). This population were categorised into six groups: known CVD 4.8% (n = 155), know diabetes 4.2% (n = 135), very high SCORE risk 0.6% (n = 20), high SCORE risk 3.4% (n = 109), moderate SCORE risk 49.2% (n = 1587) and low SCORE risk 37.8% (n = 1221). The very high SCORE risk group and the high SCORE risk group were combined into a single group (n = 129) due to the small number in the very high risk group and the identical LDL-C targets for these two groups in the clinical guidelines.
Targets for LDL-C according to CVD risk are identified in Table 3, column one [9]. Hypercholesterolaemia prevalence (LDL-C above CVD risk category target and/or on LLM) was 73% (95% CI 71.5–74.5%) (n = 2357) overall with the prevalence ranging from 66.6% (95% CI 64.0–69.3%) in the low risk group to 90.9% (95% CI 86.4–95.5%) in those with known CVD.
Examination of those with hypercholesterolaemia (n = 2357) revealed a varied picture in relation to awareness, treatment and control of LDL-C depending on the absolute level of CVD risk of individual participants (Fig. 3). Over half of those with known CVD and close to half of those with known diabetes (49%) were treated and controlled to the recommended LDL-C target level. This contrasts with the small proportion (5%) treated and controlled to target in the very high/high SCORE risk group. Lack of awareness of hypercholesterolaemia was lowest in those with existing disease (CVD and Diabetes) and high across all SCORE risk groups.
Discussion
The study reports a weighted mean TC of 5.1, 4.8 mmol/L in men and 5.3 mmol/L in women and a weighted mean LDL-C of 2.9, 2.7 mmol/L in men and 3.0 mmol/L in women in a nationally representative sample of adults aged 50–79 years in the Irish population during the period 2009–2011. One-third of adults in the age group were on lipid-lowering medication. In a subgroup aged 50–64 years, the prevalence of hypercholesterolaemia was 73%. Despite European and National policy recommendations and guidelines regarding the risks associated with high cholesterol [9, 16], control of LDL-C in those at highest risk for a CVD event is lower than expected with 57% of those with known CVD and 49% of diabetics achieving guideline targets. Lack of awareness of hypercholesterolaemia was high across all primary prevention risk groups.
These results compare with findings from a nationally representative cohort of non-institutionalised adults aged 20 years and older in the National Health and Nutrition Examination Surveys (NHANES) in the United States which found an overall TC of 196 mg/dL (equivalent to 5.0 mmol/L) and LDL-C of 116 mg/dL (equivalent to 3.0 mmol/L) during the time period 2007–2010 [17]. The Health Survey for England 2011 conducted in a community living sample of adults aged 16 years and older found a mean TC of 5.1 mmol/L in men and 5.2 mmol/L in women [18]. Differences in the age profile of participants in other studies creates difficulty in making direct comparisons, however, certain patterns in the data are similar to those found elsewhere. Women had higher cholesterol levels than men at all ages beyond 50 years in our study. This is similar to other studies of younger cohorts which found that up to the age of 50 years men had higher cholesterol levels than women, however, once over the age of 50 years women have higher cholesterol levels [19]. The finding that cholesterol levels peak higher and later in women compared to men is consistent with findings from representative surveys of the French population in 2006/2007 [20] and the Health Survey for England 2011 [19]. This unique rise in cholesterol in peri-menopausal women is also documented in the Study of Women’s Health across the Nation (SWAN) in the United States which highlights the importance of monitoring lipids in older women [21].
Previously in Ireland, the Kilkenny health project conducted TC examinations at baseline on an intervention and reference group (aged 35–64 years) in 1985–1986. Mean total cholesterol in men was 6.0 mmol/L in the intervention and in the reference group and 6.0 mmol/L in women in the intervention group and 5.9 mmol/L in the reference group [22]. While our study examines TC in an older cohort (50–79 years) it identifies a substantial decline in TC of approximately 0.9 mmol/L in the population over a 25 year period and may reflect a survivorship effect. This decline exceeds the 0.2 mmol/L decline in TC per decade in the European region as outlined by Farzadfar et al. [7] and is similar to results from the northern Sweden MONICA study between 1994 and 2014, where cholesterol levels decreased by 0.7 mmol/L in the 20 year period [23]. Previous research on a sample of 1207 adults aged 45 years and older taken from a nationally representative sample of adults in Ireland found that 18% of the population had a TC <5 mmol/L and were not on lipid-lowering medication [24]. Our study found an increase in this proportion to 22%. This may be partly due to our larger sample size, slightly older age profile or an improvement in dietary and lifestyle factors in the population during the intervening time period.
The use of cholesterol-lowering medication in this cohort (33%) was slightly higher than that reported by the National Health and Nutrition Examination Survey (NHANES) during 2011–2012 when 28% of adults aged 40 years and older were reported using prescription cholesterol-lowering medication in the previous 30 days [25].
The findings in the subgroup aged 50–64 years present an opportunity to examine interventions aimed at lowering cholesterol according to an individual’s CVD risk profile. In individuals at high risk of future CVD events i.e. those with existing CVD or diabetes, opportunities are being missed to achieve LDL-C control as recommended in clinical guidelines. These findings corroborate those found in an observational cohort of Irish patients during the same time period which found persistent dyslipidaemia despite statin therapy [26]. Our findings also reveal a low level of treatment and control and lack of awareness in those classified as very high risk (SCORE ≥10%) or high risk (SCORE ≥5 and <10%). Providing risk information has been shown to change high risk patients perception of risk and physician's prescribing habits [27] yet recent research from Ireland found that only a third of general practitioners (GPs) frequently use a CVD risk assessment tool in practice [28]. Our data is limited in that we collected information on current medication use and therefore cannot ascertain prescription of lipid-lowering medication and the extent to which non adherence to treatment is a feature of our data. Individuals at lower absolute CVD risk are required to weigh up the smaller benefits to them individually of taking medication and the adoption of lifestyle modification in consultation with their general practitioner (GP). In one UK study following the widening of the risk threshold for offering statin therapy one in four patients took up the opportunity to discuss starting statins with their GP and only one in ten chose to start a statin [29]. Poor adherence to statins is reported in primary prevention populations with low perceived risk a strong predictor of poor adherence and many displaying a preference for dietary control [30]. Our findings reveal a lack of awareness of hypercholesterolaemia in the primary prevention population including those at low, moderate and high absolute risk. The largest number of future cases of CVD will arise in the moderate risk group due to its relative size. Our findings suggest that opportunities to promote dietary and lifestyle modification at a population level to reduce future CVD are being missed.
The strengths of this study include the large nationally representative sample which allows us to generalise our findings to the older adult population in Ireland. Additional strengths include the use of standardised protocols for the interviews, health assessments and laboratory methods. The TC and LDL-C levels reported may underestimate the cholesterol profile in this population as those included in the analysis had more favourable risk profiles than respondents who did not take part in the health assessment and thus were excluded from the analysis. This selection bias was addressed at the design stage by the inclusion of home and health centre based assessments and at the analysis stage by the utilisation of calibration weights. Information on cholesterol testing and awareness of hypercholesterolaemia was based on self-report which may be subject to misclassification. In this study we used the SCORE risk assessment tool and associated guideline LDL-C target thresholds. However, a large number of CVD risk assessment tools are in use in primary care [27, 31]. While most recommend prediction models based on simple risk factor data for decision making or further investigation and management, there is no consensus on the strategy for screening, recommended target populations, screening tests or treatment thresholds [31]. We acknowledge the uncertainty this creates in using a single risk assessment tool in our analysis.
Our findings show a decrease in TC and LDL-C in line with global trends which are likely driven by improvements in diet and pharmacological interventions which reduce cholesterol. Despite these improved results at a population level, our analysis of the levels of awareness, treatment and control of hypercholesterolaemia within CVD risk categories demonstrates an ongoing need for targeted interventions to reduce LDL-C especially in those at highest risk of CVD in the older Irish population.
References
World Health Organization (2014) Global Health Estimates 2014 Summary Tables Deaths by Cause, Age and Sex, 2000–2012. World Health Organization. http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html. Accessed June 2014
Central Statistics Office (2013) Vital statistics and fourth quarter and yearly summary 2012. Central Statistics Office, Stationery Office, Dublin
Kabir Z, Perry I, Critchley J, O’Flaherty M, Capewell S, Bennett K (2013) Modelling coronary heart disease mortality declines in the Republic of Ireland 1985–2006. Int J Cardiol 168(3):2462–2467
Lewington S, Whitlock G, Clarke R, Sherliker P, Emberson J, Halsey J, Qizilbash N, Peto R, Collins R (2007) Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet 370(9602):1829–1839. doi:10.1016/s0140-6736(07)61778-4
Muntner P, Levitan EB, Brown TM, Sharma P, Zhao H, Bittner V, Glasser S, Kilgore M, Yun H, Woolley JM, Farkouh ME, Rosenson RS (2013) Trends in the prevalence, awareness, treatment and control of high low density lipoprotein-cholesterol among United States adults from 1999–2000 through 2009–2010. Am J Cardiol 112(5):664–670. doi:10.1016/j.amjcard.2013.04.041
Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH (2010) Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol 140(2):226–235. doi:10.1016/j.ijcard.2008.11.033
Farzadfar F, Finucane MM, Danaei G, Pelizzari PM, Cowan MJ, Paciorek CJ, Singh GM, Lin JK, Stevens GA, Riley LM, Ezzati M (2011) National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3.0 million participants. Lancet 377(9765):578–586. doi:10.1016/s0140-6736(10)62038-7
Ng N, Johnson O, Lindahl B, Norberg M (2012) A reversal of decreasing trends in population cholesterol levels in Vasterbotten County, Sweden. Glob Health Action 5:10367. doi:10.3402/gha.v5i0.10367
Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, Dallongeville J, De Backer G, Ebrahim S, Gjelsvik B, Herrmann-Lingen C, Hoes A, Humphries S, Knapton M, Perk J, Priori SG, Pyorala K, Reiner Z, Ruilope L, Sans-Menendez S, Op Reimer WS, Weissberg P, Wood D, Yarnell J, Zamorano JL, Walma E, Fitzgerald T, Cooney MT, Dudina A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Funck-Brentano C, Filippatos G, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Altiner A, Bonora E, Durrington PN, Fagard R, Giampaoli S, Hemingway H, Hakansson J, Kjeldsen SE, Larsen ML, Mancia G, Manolis AJ, Orth-Gomer K, Pedersen T, Rayner M, Ryden L, Sammut M, Schneiderman N, Stalenhoef AF, Tokgozoglu L, Wiklund O, Zampelas A (2007) European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil 14(Suppl 2):E1–40. doi:10.1097/01.hjr.0000277984.31558.c4
Whelan BJ (1979) RANSAM: a national random sampling design for Ireland. Econ Soc Rev 10(2):169–174
Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, De Bacquer D, Ducimetière P, Jousilahti P, Keil U, Njølstad I, Oganov RG, Thomsen T, Tunstall-Pedoe H, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Graham IM (2003) Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 24(11):987–1003. doi:10.1016/s0195-668x(03)00114-3
Kenny RA, Whelan B, Cronin H, Kamiya Y, Kearney P, O’Regan C (2010) The design of The Irish Longitudinal Study on Ageing. The Irish Longitudinal Study on Ageing, Trinity College, Dublin
Wang TY, Haddad M, Wang TS (2001) Low triglyceride levels affect calculation of low-density lipoprotein cholesterol values. Arch Pathol Lab Med 125(3):404–405. doi:10.1043/0003-9985(2001)125<0404:ltlaco>2.0.co;2
Richardson K, Kenny RA, Peklar J, Bennett K (2013) Agreement between patient interview data on prescription medication use and pharmacy records in those aged older than 50 years varied by therapeutic group and reporting of indicated health conditions. J Clin Epidemiol 66(11):1308–1316. doi:10.1016/j.jclinepi.2013.02.016
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund ULF, Yngve A, Sallis JF, Oja P (2003) International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395
Department of Health and Children (2010) Changing Cardiovascular Health National Cardiovascular Health Policy 2010–2019. Department of Health and Children, Dublin
Carroll MD, Kit BK, Lacher DA, Shero ST, Mussolino ME (2012) Trends in lipids and lipoproteins in US adults, 1988–2010. JAMA 308(15):1545–1554. doi:10.1001/jama.2012.13260
NHS The information centre for health and social care (2011) Health Survey for England 2011 Health, social care and lifestyles, Summary of key findings. Department of Health, London
Oyebode O (2012) Health Survey for Engand-2011, Health, social care and lifestyles. Chapter 2: cardiovascular disease. The Information Centre for Health and Social Care, NHS, London
Ferrieres J, Bongard V, Dallongeville J, Arveiler D, Cottel D, Haas B, Wagner A, Amouyel P, Ruidavets JB (2009) Trends in plasma lipids, lipoproteins and dyslipidaemias in French adults, 1996–2007. Arch Cardiovasc Dis 102(4):293–301. doi:10.1016/j.acvd.2009.02.002
Matthews KA, Crawford SL, Chae CU, Everson-Rose SA, Sowers MF, Sternfeld B, Sutton-Tyrrell K (2009) Are changes in cardiovascular disease risk factors in midlife women due to chronological aging or to the menopausal transition? J Am Coll Cardiol 54(25):2366–2373. doi:10.1016/j.jacc.2009.10.009
Shelley E, Daly L, Collins C, Christie M, Conroy R, Gibney M, Hickey N, Kelleher C, Kilcoyne D, Lee P, Mulcahy R, Murray P, O’Dwyer T, Radic A, Graham I (1995) Cardiovascular risk factor changes in the Kilkenny Health Project: a community health promotion programme. Eur Heart J 16(6):752–760
Eriksson M, Forslund AS, Jansson JH, Soderberg S, Wennberg M, Eliasson M (2016) Greater decreases in cholesterol levels among individuals with high cardiovascular risk than among the general population: the northern Sweden MONICA study 1994 to 2014. Eur Heart J 37(25):1985–1992. doi:10.1093/eurheartj/ehw052
Morgan K, McGee H, Watson D, Perry I, Barry M, Shelley E, Harrington J, Molcho M, Layte R, Tully N, van Lente E, Ward M, Lutmski J, Conroy R, Brugha R (2007) SLÁN 2007: survey of lifestyle, attitudes & nutrition in Ireland. Main report. Department of Health and Children, Dublin
Gu Q, Paulose-Ram R, Burt VL, Kit B (2014) Prescription cholesterol-lowering medication use in adults aged 40 and over: United States, 2003–2012. NCHS Data Brief No 177
Horgan S, Crowley J, Feely J, McAdam B, Shanahan E, Vaughan C (2011) Prevalence of dyslipidaemia in statin-treated patients in Ireland: Irish results of the DYSlipidaemia International Study (DYSIS). Ir J Med Sci 180(2):343–349. doi:10.1007/s11845-011-0702-8
Usher-Smith JA, Silarova B, Schuit E, Moons KG, Griffin SJ (2015) Impact of provision of cardiovascular disease risk estimates to healthcare professionals and patients: a systematic review. BMJ Open 5(10). doi:10.1136/bmjopen-2015-008717
Byrne D, O’Connor L, Jennings S, Bennett K, Murphy AW (2015) A survey of GPs awareness and use of risk assessment tools and cardiovascular disease prevention guidelines. Ir Med J 108(7):204–207
Usher-Smith JA, Pritchard J, Poole S, Griffin SJ (2015) Offering statins to a population attending health checks with a 10-year cardiovascular disease risk between 10% and 20%. Int J Clin Pract 69(12):1457–1464. doi:10.1111/ijcp.12742
Mann DM, Allegrante JP, Natarajan S, Halm EA, Charlson M (2007) Predictors of adherence to statins for primary prevention. Cardiovasc Drugs Ther 21(4):311–316. doi:10.1007/s10557-007-6040-4
Khanji MY, Bicalho VS, van Waardhuizen CN, Ferket BS, Petersen SE, Hunink M (2016) Cardiovascular risk assessment: a systematic review of guidelines. Ann Intern Med. doi:10.7326/M16-1110
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Ethical approval for this study was received by the Trinity College Dublin Research Ethics Committee. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Data sharing
Researchers interested in using TILDA data may access the data for free from the following sites: Irish Social Science Data Archive (ISSDA) at University College Dublin http://www.ucd.ie/issda/data/tilda/; Interuniversity Consortium for Political and Social Research (ICPSR) at the University of Michigan http://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/34315.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Murphy, C., Shelley, E., O’Halloran, A.M. et al. Failure to control hypercholesterolaemia in the Irish adult population: cross-sectional analysis of the baseline wave of The Irish Longitudinal Study on Ageing (TILDA). Ir J Med Sci 186, 1009–1017 (2017). https://doi.org/10.1007/s11845-017-1590-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-017-1590-3