Abstract
Background
Cardiovascular disease is a major cause of morbidity and mortality; however, the risks associated with this disease can be reduced by targeting circulating low-density lipoprotein cholesterol (LDL-C) with lipid-lowering drugs, as recommended in many treatment guidelines. Their effectiveness for hypercholesterolemia management depends on appropriate use in at-risk patients. Observational studies have shown varying adherence to national and international guidelines on reaching LDL-C treatment goals.
Methods
The Centralized Pan-Middle East Survey on the under-treatment of hypercholesterolemia (CEPHEUS) study observed the current management of hypercholesterolemia in patients on lipid-lowering drugs in seven Middle Eastern countries, and results from 1,043 patients in Egypt are presented here.
Results
Overall, less than 50% of patients achieved their LDL-C treatment goal, with patients at higher risk of a cardiovascular event being less likely to attain their target. Nearly, three-quarters of patients in this study were considered high or very high risk, with only 10% of high-risk patients reaching their treatment goal.
Conclusions
Management of hypercholesterolemia in Egypt is comparatively worse than the average for similar countries in the region, and many patients with high risk of CVD are not being effectively treated. Initiatives to improve physicians’ management of these patients and patient compliance to treatment are urgently needed.
Funding
AstraZeneca, Cairo, Egypt.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is the most common cause of death worldwide, accounting for an estimated 17.3 million deaths in 2008 and representing 30% of all global deaths [1]. The World Health Organization projects that CVD will remain the leading cause of death worldwide in future years, with deaths from CVD estimated to increase to 23.3 million by 2030 [1, 2].
Currently, over 80% of CVD deaths occur in low- and middle-income countries [1]. This has been attributed to the fact that people in these countries are typically exposed to more risk factors, such as tobacco and dyslipidemia [high apolipoprotein B (ApoB):apolipoprotein A1 (ApoA1) ratio] [3]. In addition, they are likely to have less access to early detection and prevention programs than patients in more developed countries [3]. These factors also contribute to the fact that the mean age [±standard deviation (SD)] of first presentation of acute myocardial infarction (AMI) has been observed to be 51.2 (±10.3) years in Middle Eastern countries, approximately 10 years younger than in other regions of the world [3, 4]. Furthermore, the Middle East has the highest proportion of first AMI in individuals aged 40 years or younger [4].
In Egypt, the age-standardized annual death rate from CVD is over 400 per 100,000 population, and this compares to rates of less than 150 per 100,000 population in some European countries [5]. The Egyptian National Hypertension Project, which surveyed over 6,700 subjects, reported the national incidence of coronary heart disease to be 8.3% [5]. The incidence was higher in women than men (8.9% versus 8.0%, respectively) and higher in urban populations than rural populations (8.8% versus 7.2%, respectively).
There is epidemiological evidence that elevated total serum cholesterol, specifically elevated levels of low-density lipoprotein cholesterol (LDL-C), is strongly correlated with the risk of coronary heart disease [6–10]. Thus, a principal intervention to reduce the risk of cardiovascular events in patients with CVD is to control the level of circulating lipids, particularly LDL-C [8, 11, 12]. Clinical intervention studies have shown that the impact of lipid-lowering treatment is primarily dependent on the individual’s baseline risk of a cardiovascular event, and that the reduction in risk of an event subsequently occurring is proportional to the degree of LDL-C lowering achieved by treatment [8, 11–13]. Therefore, since the late 1980s, guidelines for the prevention of CVD have recommended treatment goals based on reducing the baseline risk of the patient. The US National Cholesterol Education Program Adult Treatment Panel III guidelines (NCEP ATP III) on cholesterol management, originally produced in 2002 [10], were updated in 2004 [14] to reflect the findings of major clinical trials that confirmed the benefits of lipid-lowering therapy in high-risk, diabetic and elderly patients.
With the introduction of more stringent guidelines and the widespread increased use of lipid-lowering therapy, there is a need to evaluate the current level of under-treatment of hypercholesterolemia. It is also important to understand why patients being actively treated with lipid-lowering drugs do not achieve their treatment goal. The Centralized Pan-Middle East survey on the under-treatment of hypercholesterolemia (CEPHEUS) assessed the current management of hypercholesterolemia in patients on lipid-lowering drugs in Middle Eastern countries [Bahrain, Egypt, Oman, Qatar, the United Arab Emirates (UAE), the Kingdom of Saudi Arabia (KSA) and Kuwait]. The primary aim of this study was to establish the proportion of patients on lipid-lowering pharmacological treatment who attained their LDL-C treatment goal, as defined by NCEP ATP III 2002 and 2004 guidelines. Secondary endpoints included: evaluation of the proportion of patients in pre-defined sub-populations achieving their LDL-C treatment goal, identification of determinants (patient and physician characteristics) for patients not reaching their treatment goal and physician characteristics associated with the allocation of different treatment regimens. The results reported here are for the Egyptian arm of this study, which was conducted in Cairo and Alexandria.
Methods
Study Design
This was a multicenter, observational study of patients receiving lipid-lowering pharmacological treatment in Cairo and Alexandria, Egypt, conducted in 2010 and 2011 as part of the CEPHEUS study (clinicaltrials.gov identifiers: NCT01604733, NIS-EG-CRE-2012/01). All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008, and are consistent with the International Conference on Harmonisation/Good Clinical Practice (ICH-GCP). Informed consent was obtained from all patients for being included in the study.
Study Objectives
The primary objective of the study was to establish the proportion of patients receiving lipid-lowering pharmacological treatment who reach their LDL-C goals, according to the NCEP ATP III/NCEP ATP III 2004 updated guidelines [10, 14]. These guidelines recommend a therapeutic LDL-C goal of <100 mg/dL for those at high risk of cardiovascular events (10-year risk >20% of coronary heart disease), with an option to further lower the goal to <70 mg/dL for individuals at very high risk (established coronary heart disease and multiple major risk factors, severe and persistent risk factors, metabolic syndrome or acute coronary syndrome). The recommended LDL-C goal for those at moderately high risk (two or more risk factors and a 10-year risk of 10–20%) is <130 mg/dL [14]. For patients considered at low risk, non-pharmacological intervention such as changes in diet, smoking cessation and an increase in exercise are generally recommended. For patients at a higher risk, lipid-lowering drugs, e.g., statins, fibrates or cholesterol absorption inhibitors, are recommended.
Key secondary objectives were to establish the proportion of patients achieving their treatment goals and the proportion of patients achieving their target goals in the following sub-populations: primary/secondary prevention patients and patients with metabolic syndrome (defined according to NCEP ATP III). Other secondary goals were: to establish the proportion of patients on lipid-lowering pharmacological treatment reaching the non-high-density lipoprotein cholesterol (HDL-C) goals according to the NCEP ATP III/NCEP ATP III 2004 updated guidelines (<130 mg/dL) in the sub-population of patients with fasting triglycerides >200 mg/dL; to identify determinants (e.g., patient and physician characteristics, country-specific guidelines or recommendations) for under-treatment of hypercholesterolemia; and to explore physician characteristics associated with the allocation of different treatment regimens. NCEP ATP III 2004 updated guidelines and goals were used to evaluate management efficacy because they were the most commonly used at the time of study.
Study Inclusion Criteria
Subjects fulfilling the following inclusion criteria were enrolled in the study: age ≥18 years; receiving lipid-lowering drug treatment for at least 3 months with no dose change for at least 6 weeks; and provision of written informed consent to participate in the study and comply with study procedures.
Study Procedures
The study planned to enroll 1,100 randomly selected patients being treated by 78 specialists and primary care physicians located in Cairo and Alexandria, Egypt. The required sample size was calculated to ensure that the primary and secondary endpoints could be estimated with sufficient precision to represent the heterogeneity of this population, and was based on an estimated 50% of participants being expected to achieve their treatment goal.
Prior to assessing their first study participant, each investigator was required to complete a questionnaire on their experience and perception of the management of hypercholesterolemia observed in their patients. Consecutive patients who came for a regularly scheduled visit to the clinic were invited to participate in the survey. Each study participant was required to attend a single clinic visit, during which a fasting blood sample was obtained for analysis of total cholesterol, LDL-C, HDL-C, triglycerides, glucose, glycosylated hemoglobin (HbA1c) and calculation of the ratio of total cholesterol/HDL cholesterol. Three separate samples were collected from each patient and all samples were analyzed at the accredited central laboratory in Cairo. Participants also underwent a physical examination by the investigator to determine their height, weight, waist circumference and blood pressure. Following the visit, investigators received the laboratory results together with a copy of the NCEP ATP III 2004 updated guidelines [14]. These were supplied to the investigators for educational purposes to enable them to take any appropriate measures regarding the future treatment of the patient.
Prior to attendance at the clinic, participants were required to complete a questionnaire relating to their awareness of hypercholesterolemia, their current treatment schedule, treatment goals, satisfaction with treatment and their compliance to treatment. Investigators also completed a patient record form for each participant, detailing the patient’s demographics, known cardiovascular risk factors, cardiovascular medical history, current lipid-lowering drug treatment and rationale for their current treatment. Each subject had their risk category according to NCEP ATP III 2004 updated guidelines determined programmatically by an expert panel.
Statistical Analysis
The statistical analysis was of a descriptive nature. Continuous data are described by mean, SD, median, minimum and maximum values. Categorical data are described by the number and percentage of subjects in each category. Missing data were not included in the calculation of proportions. The association between achievement of LDL-C goals and patient/physician variables was analyzed by a multivariate logistic regression model.
Results
A total of 1,182 patients were enrolled in this study between 13 October 2010 and 7 June 2011. One hundred and thirty-nine patients were excluded from the analysis due to missing LDL-C data, resulting in data from 1,043 patients being included in the final analysis. The demographics and clinical characteristics of the study cohort are reported in Table 1. The mean age of participants was 54.73 years, and 50.30% were male. The main reason for pharmacological treatment was primary prevention (60.40%), and statins were the most frequent treatment of choice (94.20%). The mean laboratory blood values for all variables analyzed in the study are given in Table 2.
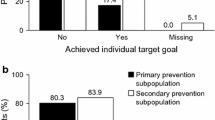
Overall, 32.5% of patients achieved their LDL-C treatment goal according to criteria outlined in the NCEP ATP III 2004 updated guidelines (Table 3). Patients considered to have a low or medium–low risk profile (as determined by NCEP ATP III 2004 updated guidelines criteria) had the highest rate of achieving their LDL-C treatment goal (Fig. 1; Table 3). Out of 187 subjects with fasting triglycerides >200 mg/dL (>2.26 mmol/L), 103 patients (55.10%) achieved their non-HDL-C treatment goal; it should be noted that information on other drugs that could have affected non-HDL-C levels is not available.
In patients with arterial hypertension, a family history of CVD or metabolic syndrome, 26.0, 30.0 and 26.1%, respectively, attained their LDL-C treatment goals, as defined by the NCEP ATP III 2004 updated guidelines (Table 4). The proportion of current smokers and patients with diabetes achieving their treatment goals was low at 17.3% and 20.6%, respectively.
Using the NCEP ATP III 2004 updated guidelines treatment goal criteria, the most effective statins were rosuvastatin, pravastatin and simvastatin, with 39.0, 37.5 and 33.8% of patients prescribed these medications achieving their LDL-C treatment goals, respectively (Table 3).
Results of the Investigators’ Questionnaire
Seventy-seven of the 78 participating investigators, covering a total of 122 sites, returned a completed questionnaire. Most of the investigators were male (92.2%) with a mean age of 50.5 years (SD 7.3). The majority of the investigators were cardiologists (55.8%); 10.4% were endocrinologists, 29.9% were other specialists and 3.9% were primary care physicians.
Most investigators (76.0%) stated that they used guidelines to establish the individual target cholesterol levels of patients, with over half of these using the NCEP ATP III 2004 updated guidelines. Additional data from the investigators’ questionnaire is presented in Table 5.
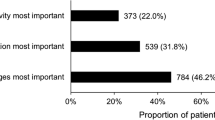
Results of the Patient Questionnaire
All of the 1,043 patients available for analysis returned the questionnaire with at least one question completed. Most patients had heard about, or been told about, LDL-C and HDL-C (78.0% and 70.7%, respectively). The majority (80.6%) had been informed of their cholesterol levels by their physician, and 76.0% had been given a target cholesterol level. Additional responses to the patients’ questionnaire are shown in Table 6.
Multivariate Analysis of Factors Associated with Achieving LDL-C Treatment Goal
The main patient and physician factors that were significantly associated with patients not attaining their NCEP ATP III 2004 updated LDL-C treatment goal were: forgetting to take tablets [odds ratio (OR) 3.3; 95% confidence interval (CI) 1.2–8.6]; being diabetic (OR 2.7; CI 2.0–3.6); smoking (OR 2.4; CI 1.6–3.9); and age <40 years (OR 1.8; CI 0.9–3.6).
Discussion
The primary aim of this study was to investigate the proportion of patients receiving lipid-lowering pharmacological treatment in Egypt who reach their LDL-C treatment goals. Study subjects had already been receiving lipid-lowering medications prior to their inclusion. Overall, this study found that the management of patients requiring lipid-lowering therapeutic intervention is moderate to poor in Egypt, with less than 50% of treated patients achieving the treatment goals stipulated in the NCEP ATP III 2004 updated guidelines. When looking at the success of treatment in patients categorized according to risk, those considered very high risk (who comprised 38% of the study population) were particularly poorly managed, with only 10% achieving their treatment goal. In contrast, over 65% of patients in the low or medium–low risk categories successfully attained their treatment goal, although it should be noted that these combined patient groups only accounted for a quarter of the study population; most study participants were in the very high and high-risk categories (72.4%).
These findings conflict with the result that most investigators (74%) stated that they used guidelines to establish individual target cholesterol levels for patients, most commonly the NCEP ATP III 2004 updated guidelines. The findings are also in contrast to the beliefs of the treating physicians, as more than 60% of investigators either agreed or strongly agreed with the statement that they felt a sufficient number of patients reached their target levels. However, the finding is more in line with patient perception, as only around 50% of patients stated that they were satisfied with their treatment.
Evaluation of sub-groups of patients with established risk factors for CVD showed that hypercholesterolemia was particularly poorly managed in patients who were current smokers (18.9% of participants) or were diabetic (48.5% of participants), whereas only 17.3% and 20.6% of patients, respectively, attained their NCEP ATP III 2004 updated LDL-C treatment goal. Patients with metabolic syndrome, arterial hypertension or a family history of CVD, 30% or less were successfully treated.
The majority of patients in this study (85.9%) were prescribed statins, which are well established as an effective treatment of dyslipidemia [15, 16]. The most commonly prescribed statins were atorvastatin and rosuvastatin, prescribed for 48.9% and 34.9%, respectively, of those patients receiving statins. The most effective statins according to this study were rosuvastatin, pravastatin and simvastatin, with 39.0, 37.5 and 33.8% of patients who were prescribed these medications achieving their LDL-C treatment goals, respectively. It should be remembered that the number of patients in the lower risk categories was low, and some of the most favorable results were observed in patients categorized according to the NCEP ATP III 2004 updated guidelines as medium or low risk who were treated with rosuvastatin. In these sub-groups of patients, >70% of patients were successfully treated.
Results of the patient questionnaire reported that most patients (>80%) had not changed their medication from their initial treatment recommendation at diagnosis, and less than 10% had received a dose increase. This finding could suggest that failure of treating physicians to adapt an individual’s response to treatment may be a factor in the overall failure of patients to be successfully managed for hypercholesterolemia.
Patient compliance to treatment is another factor that could influence treatment outcomes. In this study, 12% of patients admitted forgetting to take their prescribed medication more than once a week, and 16% stated that they forgot no more than once a month. Furthermore, in the multivariate analysis, forgetting to take tablets was strongly correlated with not attaining treatment goals.
A report of the CEPHEUS study in six Middle Eastern countries (Bahrain, Oman, Qatar, UAE, KSA and Kuwait), concluded that hypercholesterolemia was sub-optimally managed across these countries, particularly in those with a high or very high risk of a cardiovascular event [17]. In the overall regional analysis, 52% of patients attained their LDL-C treatment goal, as defined by the NCEP ATP III 2004 updated guidelines. The results reported here of the Egyptian arm of the CEPHEUS study show that management of hypercholesterolemia in Egypt is comparatively worse than the average for other similar countries in the region. Results of other arms of the CEPHEUS study commonly report that hypercholesterolemia is successfully treated in only approximately 50% of cases (Table 7). The individual results for the proportion of patients achieving their NCEP ATP III 2004 updated guideline-defined treatment goal are: 52% for South Africa, 49% for Greece, 57% for combined western European countries and 49% for combined Asian countries [18–21]. These results are in contrast to other regions of the world, where studies have reported that the majority of patients actively treated for hypercholesterolemia achieve their treatment goals. For example, in Hong Kong, 83% of the participants in the CEPHEUS study achieved their treatment goal, and the Lipid treatment assessment project 2 (L-TAP2) study, conducted in nine countries in Europe, North America and Asia, found the attainment rate was 73% in these countries [22, 23]. Similarly, concerning findings were also reported for the INTERHEART study, conducted between 1999 and 2003, which found that less than 5% of patients admitted for their first AMI in the Middle East were taking any lipid-lowering medications (primary prevention), and this only increased to 50% upon discharge (secondary prevention) [3].
This study was an observational rather than interventional study, and as such it suffers from a number of limitations. There are likely to be differences in clinical practice between study sites, and this was not accounted for in the combined analysis of the data. Furthermore, the study population comprised only those patients being actively treated with lipid-lowering medication, and the proportion of eligible patients with risk factors for CVD being actively treated was not ascertained. In addition, data on lifestyle factors or socioeconomic status were not collected and, therefore, not considered in the analysis. These combined factors should be taken into consideration when evaluating the findings.
At the time of conducting the study (2010–2011), most physicians treated patients according to the NCEP ATP III 2004 updated guidelines. Since the end of the study, updated guidance from the American College of Cardiology and American Heart Association has concluded that there was insufficient evidence to support the continued use of LDL-C or non-HDL-C treatment targets, instead recommending different intensities of statin treatment for patients based on four statin benefit groups [24]. While it would be interesting to apply the updated guidance to the results of this study, due to the enrolment criterion of patients already receiving lipid-lowering drugs for at least 3 months there are no baseline measurements against which to compare. Additionally, resource limitations prevent us from re-classifying patients into the revised risk groups to perform re-analyses against the latest guidance, or from providing additional statistical analyses on comparisons between risk groups.
Conclusion
In conclusion, this study found that hypercholesterolemia is not being effectively managed in many at-risk patients in Egypt. The majority of patients enrolled in the study, all of whom were being actively treated with lipid-lowering medication, were considered at high risk of a cardiovascular event, and hypercholesterolemia was particularly poorly managed in this group. Initiatives to improve physicians’ management of these patients and patient compliance to treatment are urgently needed.
References
World Health Organization. Global status report on noncommunicable diseases 2010. Geneva: WHO; 2011. http://www.who.int/nmh/publications/ncd_report_full_en.pdf. Accessed Oct 30, 2014.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442.
Gehani AA, Al-Hinai AT, Zubaid M, INTERHEART Investigators in Middle East, et al. Association of risk factors with acute myocardial infarction in Middle Eastern countries: the INTERHEART Middle East study. Eur J Prev Cardiol. 2014;21:400–10.
Yusuf S, Hawken S, Ounpuu S, INTERHEART Study Investigators, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52.
Almahmeed W, Arnaout MS, Chettaoui R, et al. Coronary artery disease in Africa and the Middle East. Ther Clin Risk Manag. 2012;8:65–72.
Alberti KG, Zimmet P, Shaw J, IDF Epidemiology Task Force Consensus Group. The metabolic syndrome–a new worldwide definition. Lancet. 2005;366:1059–62.
Law MR, Wald NJ, Thompson SG. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ. 1994;308:367–72.
Law MR, Wald NJ, Rudnicka AR. Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis. BMJ. 2003;326:1423.
Law MR, Wald NJ. An ecological study of serum cholesterol and ischaemic heart disease between 1950 and 1990. Eur J Clin Nutr. 1994;48:305–25.
Program National Cholesterol Education (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III): final report. Circulation. 2002;106:3143–421.
The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339:1349–57.
LaRosa JC, He J, Vupputuri S. Effect of statins on risk of coronary disease: a meta-analysis of randomized controlled trials. JAMA. 1999;282:2340–6.
Alter DA, Manuel DG, Gunraj N, Anderson G, Naylor CD, Laupacis A. Age, risk-benefit trade-offs, and the projected effects of evidence-based therapies. Am J Med. 2004;116:540–5.
Grundy SM, Cleeman JI, Merz CN, National Heart, Lung, and Blood Institute; American College of Cardiology Foundation; American Heart Association, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–39.
The Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4,444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;344:1383–9.
Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279:1615–22.
Arafah M, Al-Hinai AT, Mahmeed WA, et al. Centralized Pan-Middle East survey on the undertreatment of hypercholesterolemia: results from the CEPHEUS study in Arabian Gulf countries. Angiology. 2014;65:919–26.
Raal F, Schamroth C, Blom D, et al. CEPHEUS SA: a South African survey on the under-treatment of hypercholesterolaemia. Cardiovasc J Afr. 2011;22:234–40.
Elisaf MS, Nikas N. Centralized Pan-European survey on the undertreatment of hypercholesterolemia in patients using lipid lowering drugs—the CEPHEUS-Greece survey. Angiology. 2010;61:465–74.
Hermans MP, Castro Cabezas M, Strandberg T, et al. Centralized Pan-European survey on the under-treatment of hypercholesterolaemia (CEPHEUS): overall findings from eight countries. Curr Med Res Opin. 2010;26:445–54.
Park JE, Chiang CE, Munawar M, et al. Lipid-lowering treatment in hypercholesterolaemic patients: the CEPHEUS Pan-Asian survey. Eur J Prev Cardiol. 2012;19:781–94.
Chan RH, Chan PH, Chan KK, et al. The CEPHEUS Pan-Asian survey: high low-density lipoprotein cholesterol goal attainment rate among hypercholesterolaemic patients undergoing lipid-lowering treatment in a Hong Kong regional centre. Hong Kong Med J. 2012;18:395–406.
Waters DD, Brotons C, Chiang CW, Lipid Treatment Assessment Project 2 Investigators, et al. Lipid treatment assessment project 2: a multinational survey to evaluate the proportion of patients achieving low-density lipoprotein cholesterol goals. Circulation. 2009;120:28–34.
Stone NJ, Robinson JG, Lechtenstein AH, American College of Cardiology/American Heart Association Task Force on Practice Guidelines, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults. J Am Coll Cardiol. 2014;63:2889–934.
Acknowledgments
Sponsorship for this study and article processing charges were provided by an unrestricted research grant from AstraZeneca, Cairo, Egypt. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis. Editorial assistance for the development of the manuscript was provided by Dr Debra Scates and Dr Toby Galbraith of IMC Healthcare Communication, London, UK, supported by AstraZeneca Egypt. All named authors meet the ICMJE criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole and have given final approval for the version to be published.
Conflict of interest
A. Reda, A. A. Abdel-Rehim, A. Etman and O. S. A. Afifi declare no conflict of interest.
Compliance with ethics guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008. Informed consent was obtained from all patients for being included in the study.
Author contributions
A. Reda is the principal investigator of this study and provided data interpretation and critical revision of article. A. A. Abdel-Rehim provided the study concept and design, and analyzed the data for diabetic sub-groups. A. Etman provided study concept, design and data interpretation. O. S. A. Afifi provided data interpretation and critical revision of article.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial registration: ClinicalTrials.gov Identifier: NCT01604733, NIS-EG-CRE-2012/01.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Reda, A., Abdel-Rehim, A.A., Etman, A. et al. Centralized Pan-Middle East Survey on the Under-Treatment of Hypercholesterolemia: Results from the CEPHEUS Study in Egypt. Cardiol Ther 3, 27–40 (2014). https://doi.org/10.1007/s40119-014-0031-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-014-0031-x