Abstract
Purpose
Patients with moderate and severe slipped capital femoral epiphysis (SCFE) develop osteoarthritis earlier in life in association with mechanical impingement.
Methods
To correct deformity and diminish impingement, we performed epiphysiodesis combined with an Imhauser intertrochanteric osteotomy (ITO) in moderate and severe slipped capital femoral epiphysis. We downgraded the angle of the head relative to the acetabulum into an angle corresponding to a mild slip or even an anatomical position. Our hypothesis is that the avoidance of anterior impingement at an early stage can prevent the development of osteoarthritis.
Results
The results of 28 patients (32 hips) were evaluated. Outcome parameters were SF-36, Harris Hip Score, range of motion, Kellgren–Lawrence score, chondrolysis and avascular necrosis. After a median follow-up of 8 (range 2–25) years, the group was clinically, functionally and socially performing well. Radiologically, there was no sign of chondrolysis or avascular necrosis, and more than 80% of the patients did not show any signs of osteoarthritis.
Conclusions
Based on these results, we conclude that a one-stage Imhauser ITO combined with epiphysiodesis performed on patients with moderate and severe SFCE gives satisfactory results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
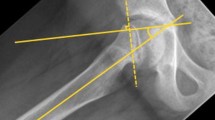
The long-term prognosis of slipped capital femoral epiphysis (SCFE) is largely influenced by the residual deformity, which in turn is related to the extent of slip. One of the methods for classifying the extent of slip is the Southwick classification [1, 2] which, based on lateral head shaft angle, places slip into one of three categories: mild (<30°), moderate (30–60°) and severe (>60°). The femoral head is mostly displaced medially and posteriorly. This displacement causes the metaphysis to move upward and laterally in relation to the femoral head, possibly resulting in anterior impingement with flexion of the hip [3] (Fig. 1a, b). It is thought that repetitive early mechanical abrasion of the prominent metaphysis against the anterior rim of the acetabular cartilage can trigger osteoarthritis [4, 5]. Patients with mild SCFE (<30°) have good prognoses, but patients with moderate and severe SCFE have an increased chance of developing osteoarthritis [6–8].
The primary objective of SCFE treatments is stopping further slippage, chondrolysis and avascular necrosis (AVN). The choice of treatment is also influenced by the stability of the slip, as described by Loder [9]. In cases of unstable SCFE, most surgeons perform an early gentle reduction of the head followed by epiphysiodesis; for stable slips, the standard approach is to stabilize the slip by in situ epiphysiodesis without reduction [10].
Various techniques have been described to correct the residual deformity. Some authors recommend performing an intertrochanteric osteotomy (ITO) as a secondary procedure after closure of the growth plate [11, 12]. In cases of severe chronic slips, many authors advice performing a subcapital osteotomy to correct the deformity completely; however, this procedure can have a high incidence of AVN and chondrolysis [13–18].
We hypothesized that an early ITO performed concurrently with the epiphysiodesis in patients with a moderate or severe slip of the femoral epiphysis would prevent the metaphysis from damaging the anterior part of the acetabulum and, thereby, diminish the incidence of osteoarthritis at a later stage. We also expected that the occurrence of chondrolysis and AVN would be low or absent with this procedure.
The aim of the study reported here was to investigate the outcomes of epiphysiodesis combined with an Imhauser ITO performed in one session in moderate and severe slips. The objective of this combined surgical approach is to improve the position of the head in relationship to the acetabulum in order to obtain better prognostic features.
Materials and methods
Subjects
This retrospective study assesses the results of a consecutive series of 28 patients who had moderate to severe SCFE in a total of 32 hips. These patients were treated with a combined epiphysiodesis and Imhauser ITO performed by the same surgeon at the AMC Amsterdam between 1978 and 2003. Patient data are presented in Table 1. A total of 13 patients had bilateral slips versus 15 who had unilateral slips. Of the 13 bilateral patients, four underwent bilateral ITO simultaneously. The other nine had a moderate to severe SCFE on one side only and a mild slip contralaterally and underwent only a K-wire transfixation on the controlateral side. A review of the medical histories of this patient cohort revealed that 13 patients had sustained a trauma. None of the patients had a deviant endocrinological history.
Approval of the medical ethical committee was obtained.
Surgery
Prior to surgery, patients were treated by bed rest on springs and slings for an average of 14 (range 0–28) days. During this time, we designed a time-schedule for operating on the patient. We did not perform gentle reduction on any of our patients. A cannulated screw epiphysiodesis was performed via an open procedure with the use of one 5.0-mm screw. During the same surgical session, following the epiphysiodesis, the Imhauser three-dimensional ITO was performed and fixed with a 90° blade plate [19] (Fig. 2a, b). Thus, the alignment of the head was changed in three directions relative to the acetabulum: flexion, varus and derotation. Peroperative fluoroscopy was performed to verify the position of the seating chisel and screws. All patients with an unilateral slipped hip were treated with a preventive K-wire fixation at the contralateral hip. Patients were not allowed to bear weight for 6 weeks.
Outcome assessments
Data are based on patients’ notes and the X-ray results. Patients were traced and asked to complete questionnaires [part of the Harris Hip Score (HHS) and Short-Form Health Survey (SF-36)] at home; they also were invited for a clinical and radiological evaluation.
The range of motion and body mass index (BMI) were determined during the clinical examination, and hip function was measured using the HHS [20]. The completed SF-36 questionnaire was used as a measure of the general health of the patients relative to the Dutch general population [21].
Osteoarthritis of the hip at follow-up was quantified from the X-rays using the Kellgren–Lawrence scale (0–4) [22, 23]. The presence of chondrolysis and avascular necrosis was also assessed from the X-rays. Of the six patients who were not able to come to the clinic, the most recent X-rays available were used instead.
Statistical analysis
Results were analyzed using SPSS ver. 12.0 software (SPSS, Chicago, IL). Due to skewed distributions, continuous data (HHS, SF36, range of motion) were described as medians and ranges. The outcomes were analyzed non-parametrically using Mann–Whitney U tests in for independent comparisons and Wilcoxon signed-rank tests for pre- and post-operative comparisons. Categorical variables were described as numbers and percentages and were compared using the chi-square test. A p value <0.05 was taken to be significant.
Results
Of the 28 patients, 24 responded to the questionnaires. Twenty-two patients were able to come to the clinic for re-assessment and radiographic evaluation. The median period of follow-up of all patients was 8.2 years (range 2.0–25.7).
Two early postoperative complications were seen. The first was a leaking wound without infection, and the second was a patient who developed calf thrombosis in the operated leg. Both complications were successfully treated. No long-term complications occurred.
All osteotomies healed uneventfully. Neither chondrolysis nor avascular necrosis were seen on the X-rays.
Of the 32 slips, 22 were classified moderate and ten as severe. From the 22 moderate slips, 21 were downgraded to a mild slip and one was still a moderate slip (from 52° to 35°). Of the ten severe slips, seven were downgraded to moderate slips and three were even downgraded to mild slips. The mean slip was significantly improved from 52° (range: 30–74°) to 22° (range 0–56°) (P < 0.01).
Compared to the preoperative examination, the range of motion was significantly improved 1 year after the operation and also at the last clinical examination (Table 2).
The HHS had an ‘excellent’ median score of 93 (range 49–100), with 17 (71%) patients scoring excellent/good and seven (29%) scoring fair/poor. The outcomes of the SF-36 were not significantly different from the those of the Dutch general population match for age [21] (Table 3).
The Kellgren–Lawrence score in our group was ≤1 in 80% on the anteroposterior X-ray and ≤1 in 100% on the false profile X-ray. Chondrolysis and AVN were not observed.
The preoperative lateral head shaft angle was not correlated with the outcome variables HHS, SF-36 and the Kellgren–Lawrence score. These outcome variables were also not correlated by the length of the follow-up.
Whereas normal values for BMI are between 19 and 25 kg/m2 [24], in our group the BMI was 26.1 (range 18.7–39.1) kg/m2 preoperatively and 28.5 (range 16.3–47.5) kg/m2 at the last follow-up. More than half of the patients were and continued to be overweight.
Discussion
We have evaluated the long-term results following the treatment of moderate and severe SCFE with an epiphysiodesis and an ITO in one session. By performing the osteotomy, we were able to downgrade the severe and moderate slips into moderate and mild slips and even, if possible, into an anatomical position to improve the position of the head relative to the acetabulum.
Previous cohort studies reported a relationship between the severity of the slip and the incidence of osteoarthritis. Carney and Weinstein [6] described a group of 28 patients (31 hips) with 41 years of follow-up. The 17 mild slips scored significantly better in terms of radiological grade assessment and Iowa Hip Rating than the 14 moderate and severe slips. Hansson et al. [7] claimed that mild slips can give excellent results as well; however, they stated that more long-term studies are needed to determine whether corrective osteotomies are required for slips >30°. Ordeberg et al. [8] also concluded, after reviewing the long-term results of 49 patients, that patients with pronounced slipping have the highest incidence of arthrosis.
The risk of osteoarthritis is thought to be associated with repetitive trauma between the femoral metaphysis and acetabulum during flexion. It has been shown that anterior impingement by the prominent metaphysis can damage the anterior part of the acetabulum [4, 25].
Although most slips have remodeling potential, there may not be enough to prevent osteoarthritis in moderate and severe slips. In their respective patient series with severe slips, Wong-Chung and Strong [26] reported the remodeling to be only 11.7° and Belleman et al., to be only 13.5° [27]. This is not nearly enough to remodel the severe slip to a mild slip.
To prevent damage to the anterior part of the acetabulum, an osteotomy can be performed to correct the lateral head shaft angle. Both subcapital and intertrochanteric osteotomies have been described. The anatomical position can be better regained with a subcapital osteotomy; however, this procedure can be associated with high rates of AVN and chondrolysis, varying from 4.5% up to 28.5% [15, 17]. Diab et al. [28] compared the ITO with the subcapital osteotomy and concluded that ITO is a safe, effective and reproducible realignment procedure. This conclusion supports our findings. No sign of chondrolysis and AVN was observed in any of our patients, and all osteotomies healed uneventfully. Jerre et al. [29] described a better short-term outcome of the ITO (11 patients) in comparison with the subcapital osteotomy (22 patients). However, their long-term results of the ITO were worse (see Table 4), which may have been caused by the fact that they used an older ITO technique (before the Southwick ITO was introduced).
The timing of performing the osteotomy relative to the epiphysiodesis is controversial. Performing the ITO at an early phase should be beneficial if damage by impingement plays a role in the aetiology of osteoarthritis. Other options are to perform the osteotomy at closure of the growth plate or with a decline in the range of motion [5, 11, 12]. Theoretically, the less the anterior acetabulum is exposed to abrasion from the prominent metaphysic, the better. For this reason, we advocate performing an ITO at the same time as the epiphysiodesis [30, 31]. This also eliminates the necessity of a second surgery, thereby reducing the burden for the patient. To date, we have not found indications of severe osteoarthritis based on the Kellgren–Lawrence scale. Nevertheless, Maussen et al. [32] showed in their cohort that patients with severe slips performed worse in later life, even after an intertrochanteric corrective osteotomy. In our study, we did not observe any relationship between preoperative lateral head shaft angle and the outcome parameters.
A number of studies have evaluated the outcome of the corrective ITO itself (Table 4). The use of different scoring systems of hip function and different methods of evaluating the radiographs makes it difficult to compare these studies. Unfortunately, in many previous studies, the timing of the ITO procedure relative to the epiphysiodesis was not reported. If the osteotomy is performed much later than the epiphysiodesis, damage may already have occurred to initiate a degenerative process. In general, the studies show that the outcome gets worse with the length of follow-up time. In our study, we were unable to detect a relation between follow-up time and outcome variables. However, a larger study population and a longer follow-up time may be needed to detect such a relationship.
The occurrence of SCFE is known to be related to BMI [33–35]. As expected, the BMI in our group was high, with more than half of our patients being overweight. Based on the increasing obesity problem in children in Europe and the USA, it is likely that the incidence of SCFE will increase. An increase in SCFE has already been shown in Japan [36]. Based on current knowledge, the optimal treatment of SCFE cannot yet be established. Since most effects of SCFE only become apparent after many years, more long-term studies are needed in which treatment and outcome variables are standardized.
Conclusion
Based on the results of our study, we conclude that performing an ephysiodesis at the same time as an Imhauser ITO to prevent early impingement on the anterior acetabulum in moderate and severe SFCE gives early satisfactory results. After a follow-up period of 8 (range: 2–25) years, all of our patients in the study group are performing well clinically, functionally and socially. The X-rays showed no signs of chondrolysis or AVN, and more than 80% of the patients did not show any signs of osteoarthritis.
References
Uglow MG, Clarke NM (2004) The management of slipped capital femoral epiphysis. J Bone Joint Surg Br 86(5):631–635
Southwick WO (1967) Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J Bone Joint Surg Am 49(5):807–835
Abraham E, Gonzalez MH, Pratap S et al (2007) Clinical implications of anatomical wear characteristics in slipped capital femoral epiphysis and primary osteoarthritis. J Pediatr Orthop 27(7):788–795
Leunig M, Casillas MM, Hamlet M et al (2000) Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand 71(4):370–375
Tjoumakaris FP, Wallach DM, Davidson RS (2007) Subtrochanteric osteotomy effectively treats femoroacetabular impingement after slipped capital femoral epiphysis. Clin Orthop Relat Res 464:230–237
Carney BT, Weinstein SL (1996) Natural history of untreated chronic slipped capital femoral epiphysis. Clin Orthop Relat Res 322:43–47
Hansson G, Billing L, Hogstedt B, Jerre R, Wallin J (1998) Long-term results after nailing in situ of slipped upper femoral epiphysis. A 30-year follow-up of 59 hips. J Bone Joint Surg Br 80(1):70–77
Ordeberg G, Hansson LI, Sandstrom S (1984) Slipped capital femoral epiphysis in southern Sweden. Long-term result with no treatment or symptomatic primary treatment. Clin Orthop Relat Res 191:95–104
Loder RT, Richards BS, Shapiro PS, Reznick LR, Aronson DD (1993) Acute slipped capital femoral epiphysis: the importance of physeal stability. J Bone Joint Surg Am 75(8):1134–1140
Witbreuk M, Besselaar P, Eastwood D (2007) Current practice in the management of acute/unstable slipped capital femoral epiphyses in the United Kingdom and the Netherlands: results of a survey of the membership of the British Society of Children’s Orthopaedic Surgery and the Werkgroep Kinder Orthopaedie. J Pediatr Orthop B 16(2):79–83
Diab M, Daluvoy S, Snyder BD, Kasser JR (2006) Osteotomy does not improve early outcome after slipped capital femoral epiphysis. J Pediatr Orthop B 15(2):87–92
Kallitzas J, Braunsfurth A (1977) Should osteotomy after Imhauser be performed immediately or only following setting and healing of epiphysiolysis of the head of the femur? (author’s translation). Z Orthop Ihre Grenzgeb 115(6):848–850
Velasco R, Schai PA, Exner GU (1998) Slipped capital femoral epiphysis: a long-term follow-up study after open reduction of the femoral head combined with subcapital wedge resection. J Pediatr Orthop B 7(1):43–52
Biring GS, Hashemi-Nejad A, Catterall A (2006) Outcomes of subcapital cuneiform osteotomy for the treatment of severe slipped capital femoral epiphysis after skeletal maturity. J Bone Joint Surg Br 88(10):1379–1384
Gage JR, Sundberg AB, Nolan DR, Sletten RG, Winter RB (1978) Complications after cuneiform osteotomy for moderately or severely slipped capital femoral epiphysis. J Bone Joint Surg Am 60(2):157–165
Dunn DM (1964) The treatment of adolescent slipping of the upper femoral epiphysis. J Bone Joint Surg Br 46:621–629
Fish JB (1994) Cuneiform osteotomy of the femoral neck in the treatment of slipped capital femoral epiphysis. A follow-up note. J Bone Joint Surg Am 76(1):46–59
Hagglund G, Hansson LI, Ordeberg G, Sandstrom S (1986) Slipped capital femoral epiphysis in southern Sweden. Long-term results after femoral neck osteotomy. Clin Orthop Relat Res 210:152–159
Imhauser G (1966) Imhauser’s osteotomy in the florid gliding process. Observations on the corresponding work of B.G. Weber. Z Orthop Ihre Grenzgeb 102(2):327–329
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51(4):737–755
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–483
Reijman M, Hazes JM, Pols HA et al (2005) Role of radiography in predicting progression of osteoarthritis of the hip: prospective cohort study. Br Med J 330(7501):1183
Altman R, Alarcon G, Appelrouth D et al (1991) The American college of rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum 34(5):505–514
Bulik CM, Wade TD, Heath AC et al (2001) Relating body mass index to figural stimuli: population-based normative data for Caucasians. Int J Obes Relat Metab Disord 25(10):1517–1524
Rab GT (1999) The geometry of slipped capital femoral epiphysis: implications for movement, impingement, and corrective osteotomy. J Pediatr Orthop 19(4):419–424
Wong-Chung J, Strong ML (1991) Physeal remodeling after internal fixation of slipped capital femoral epiphyses. J Pediatr Orthop 11(1):2–5
Bellemans J, Fabry G, Molenaers G, Lammens J, Moens P (1996) Slipped capital femoral epiphysis: a long-term follow-up, with special emphasis on the capacities for remodeling. J Pediatr Orthop B 5(3):151–157
Diab M, Hresko MT, Millis MB (2004) Intertrochanteric versus subcapital osteotomy in slipped capital femoral epiphysis. Clin Orthop Relat Res 427:204–212
Jerne R, Hansson G, Wallin J, Karlsson J (1996) Long-term results after realignment operations for slipped upper femoral epiphysis. J Bone Joint Surg Br 78(5):745–750
Schai PA, Exner GU, Hansch O (1996) Prevention of secondary coxarthrosis in slipped capital femoral epiphysis: a long-term follow-up study after corrective intertrochanteric osteotomy. J Pediatr Orthop B 5(3):135–143
Ireland J, Newman PH (1978) Triplane osteotomy for severely slipped upper femoral epiphysis. J Bone Joint Surg Br 60-B((3):390–393
Maussen JP, Rozing PM, Obermann WR (1990) Intertrochanteric corrective osteotomy in slipped capital femoral epiphysis. A long-term follow-up study of 26 patients. Clin Orthop Relat Res 259:100–110
Manoff EM, Banffy MB, Winell JJ (2005) Relationship between body mass index and slipped capital femoral epiphysis. J Pediatr Orthop 25(6):744–746
Poussa M, Schlenzka D, Yrjonen T (2003) Body mass index and slipped capital femoral epiphysis. J Pediatr Orthop B 12(6):369–371
Loder RT (1996) The demographics of slipped capital femoral epiphysis. An international multicenter study. Clin Orthop Relat Res 322:8–27
Noguchi Y, Sakamaki T (2002) Epidemiology and demographics of slipped capital femoral epiphysis in Japan: a multicenter study by the Japanese paediatric orthopaedic association. J Orthop Sci 7(6):610–617
Parsch K, Zehender H, Buhl T, Weller S (1999) Intertrochanteric corrective osteotomy for moderate and severe chronic slipped capital femoral epiphysis. J Pediatr Orthop B 8(3):223–230
Kartenbender K, Cordier W, Katthagen BD (2000) Long-term follow-up study after corrective Imhauser osteotomy for severe slipped capital femoral epiphysis. J Pediatr Orthop 20(6):749–756
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Witbreuk, M.M.E.H., Bolkenbaas, M., Mullender, M.G. et al. The results of downgrading moderate and severe slipped capital femoral epiphysis by an early Imhauser femur osteotomy. J Child Orthop 3, 405–410 (2009). https://doi.org/10.1007/s11832-009-0204-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-009-0204-7