Abstract
Purpose
Mild slipped capital femoral epiphyses (SCFE) nevertheless show significant femoral head–neck deformities which may put cartilage and acetabular labrum at risk. Whether this deformity can be restored to normal has not yet been described in the literature.
Methods
In a prospective follow-up study, 14 patients with mild SCFE underwent in situ fixation with a single 6.5-mm cancellous, partially threaded screw. In 14 patients arthroscopic osteochondroplasty was performed, and in 13 patients pre- and postoperative measurements of the α-angle were made using antero-superior radial magnetic resonance imaging.
Results
After arthroscopic osteochondroplasty, the mean α-angle decreased from 57° (range 50°–74°) to 37° (range 32°–47°; p < 0.001). Six patients showed beginning degenerative intra-articular changes (four antero-superior cartilage and three antero-superior labrum lesions) at the time of hip arthroscopy. No intra-operative complications occurred. In one patient, arthroscopic debridement was necessary due to arthrofibrosis and persistent pain.
Conclusion
Arthroscopic osteochondroplasty can successfully correct the antero-superior α-angle in patients with mild SCFE to normal values. Clinical randomized controlled studies with long-term follow-up are required to find evidence of improved functional and radiographic mid- and long-term outcome compared to in situ fixation alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Slipped capital femoral epiphysis (SCFE) mainly occurs in young teenage boys, and is associated with overweight and endocrine disorders [1]. Its incidence is increasing, especially in younger children, and might even be under-reported due to its clinically silent course [1, 2]. SCFE is defined by a dorso-medial slippage of the proximal femoral epiphysis, leading to a change in the femoral head–neck axis, a femoro-acetabular pressure area and a consecutive femoral head–neck deformity antero-laterally. Goodman et al. [3] found a strong correlation between post-slip morphology (pistol-grip and femoral head tilt deformity) and osteoarthritis. He described “anterior flattening of the acetabulum, cystic degeneration in the anterior metaphyseal-epiphyseal region, and progression to global osteoarthritis”. This description corresponds to antero-superior femoro-acetabular impingement (FAI).
As described by Rab [4], the altered biomechanical femoro-acetabular contact area can lead to impaction-type or inclusion-type impingement. The latter is due to a prominence (bump) on the head–neck junction in mild SCFE [5] or to the remodelling process in higher grade SCFE resulting in a cam deformity. Impaction-type impingement is due to an abutment of the proximal metaphysis on the acetabular rim, which cannot enter the acetabulum as occurs in higher grade SCFE. Due to the hinge and lever effect on the acetabulum rim, increasing stress on the posterior acetabular cartilage is applied as well as direct antero-superior labral injuries [4]. Early degenerative changes with cartilaginous and labral injuries have been reported not only in moderate and severe but also in mild SCFE [3, 5–12].
Once mild SCFE is diagnosed, first-line therapy aims at decreasing further slippage without compromising epiphyseal vascularisation and chondrolysis [13] by in situ fixation with one or two cannulated, fully or long-threaded screws [14]. In moderate or severe SCFE open reduction and fixation may be indicated [15].
After in situ fixation of mild SCFE, cam deformity remains. We therefore conducted a prospective study of patients after in situ fixation suffering mild SCFE, and performed arthroscopic femoral neck osteochondroplasty. Our hypothesis was that by arthroscopic intervention, head–neck offset morphology could be restored to normal by comparing their pre- and postoperative α-angles on magnetic resonance imaging (MRI).
Methods
Between January 2011 and August 2013, 23 patients presented with SCFE to the local university orthopaedic division. Following the Southwick classification of SCFE [16], eight patients with moderate to severe SCFE (>30°) were allocated to open reduction and fixation, and 15 patients with mild SCFE were allocated to percutaneous in situ fixation using a 6.5-mm cannulated screw [17]. On the contralateral side, in situ fixation by an identical method was performed prophylactically. Primary surgery was performed by two experienced paediatric orthopaedic surgeons. After in situ fixation the patients were referred for arthroscopic osteochondroplasty to the department of hip surgery. In 14 patients informed consent was given by their legal guardian before taking part in this study; one patient refused to take part in this study.
Ethical approval was obtained by the local ethical committee and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Hip arthroscopy
Hip arthroscopy was performed by two experienced orthopaedic hip surgeons. Standard antero-lateral and anterior portals were used for central assessment of labral and cartilaginous injuries and categorized with Beck’s classification [18]. An accessory distal mid-anterior portal was used to perform osteochondroplasty.
Radiological measurements
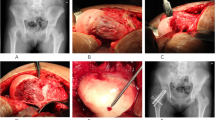
The head–shaft angle was measured as described by Southwick [16] on Lauenstein radiographs (Fig. 1). The α-angle was measured according to Nötzli et al. [8] on pre- and post-arthroscopic MRI (Fig. 2a). Radial reformatted MR images were used, since axial slices might underestimate the deformity [19, 20]. The largest α-angle between the anterior and superior position on the femoral neck was recorded and its position measured in degrees (the superior position being 0° and the anterior position 90°). The analysis of the α-angle was performed antero-superiorly, since this is the predominant localisation with the largest extent for femoral neck deformity in patients after SCFE [9, 19].
Measurement for head–shaft angle on conventional radiograph (patient no. 5) [16]
Statistics
Inter-rater reliability was performed with intra-class correlation for single measures. Comparisons of means of non-parametric continuous data were performed using the Mann–Whitney U test. Significance was accepted at p < 0.05.
Results
Fourteen patients (six female and eight male, 12.6 ± 1.1 years) were referred for arthroscopic osteochondroplasty: 13 with mild SCFE (mean head–shaft angle 16° ± 6°) and one patient with moderate SCFE, which was initially classified and referred as mild (Table 1). Arthroscopic osteochondroplasty was performed 3.7 weeks (range 0.7–14.1) after bilateral in situ fixation.
Measurements of α-angle were 25° ± 11° (range 5°–36°) on the clock model. Prior to arthroscopy, a mean α-angle of 57° ± 7° was found. A mean correction of 20° (range 8°–34°) at the antero-superior level could be achieved (Fig. 2), with all patients having a postoperative α-angle of less than 50° (Table 1). During arthroscopy, two grade I and two grade III cartilaginous injuries were found at the antero-superior level according to Beck’s classification. Antero-superior labral fraying was observed in three patients. None of these lesions required specific treatment except for slight debridement. No intra-operative complications occurred (Fig. 3). The patient with moderate SCFE requested arthroscopic debridement of arthrofibrosis 6 months after primary osteochondroplasty. No other complications occurred postoperatively, with a mean follow-up of 1.4 ± 0.7 years (0.9–3.4 years).
Inter-rater reliability of the Southwick angle (r = 0.97, p < 0.001), pre-operative α-angle (r = 0.96, p < 0.001) and postoperative α-angle (r = 0.86, p < 0.001) was excellent.
Discussion
Our results show that the pathological α-angle measured at the antero-superior aspect of the femoral neck in patients who suffer SCFE can reliably be corrected by hip arthroscopy by an average of 20°. All postoperative α-angles were below 50°, which is considered normal [8, 9, 20]. Similar reductions of α-angle in patients with FAI but without a history of SCFE were described previously on cross-table, frog-leg, and antero-posterior radiographs after arthroscopic treatment [21].
In our cohort, four out of 14 patients showed beginning degeneration of the antero-superior acetabular cartilage and three patients of the antero-superior labrum in arthroscopy, which is in accordance with the literature [7, 22–24]. These still-asymptomatic lesions in our patients might become clinically evident years later and require secondary surgical treatment [25, 26].
Most studies agree that each grade of SCFE is equally associated with progression to hip osteoarthritis [23, 26], therefore early preventive intervention is desirable. In a retrospective study by Castaneda et al. [27] all patients, regardless of the severity of the initial epiphyseal slip—measured by the head–shaft angle—showed radiographic signs of osteoarthritis after a 22.3-year follow-up period; two out of three patients experienced pain when sitting or riding a bicycle and almost 90 % with the positive impingement test. On the other hand, some patients show satisfactory long-term outcome in their hip function even after severe head–neck deformity after SCFE without any surgical treatment [28–30]. This might to some extent be due to partial spontaneous remodelling of the proximal femoral epiphysis [30–32]. Most interestingly, in situations of pre-slip or prophylactic in situ fixation, Dodds et al. found no clinical hip impingement, leading to the conclusion that only slip leads to femoro-acetabular impingement [26]. Whether early arthroscopic osteochondroplasty is superior to a more expectant approach to correcting femoral head–neck deformity when epiphyseal growth is finished is unknown.
Since the most pronounced deformity is found at the antero-superior and superior level [9], corrective osteochondroplasty is easily accessible by arthroscopy using standard portals (Fig. 4), [9, 33]. Except for one arthroscopic re-intervention due to arthrofibrosis 6 months after osteochondroplasty, no complications occurred. It can be assumed that an additional arthroscopic remodelling of the femoral neck after in situ fixation in patients with mild SCFE is a safe procedure, at least in the short term, that can restore the α-angle. Hence it might have the potential, as in patients with hip impingement, to reduce the early onset of symptoms and improve hip function and functional activity [9, 34, 35]. Whether one- or two-stage surgery should be favoured is unknown [24].
Restoring the α-angle in patients with moderate SCFE might also be possible, as shown for patient 13 (Table 1). The number of patients, however, is too small to state whether arthroscopic osteochondroplasty in patients with a head–shaft angle of more than 30° is contraindicated. In moderate and severe SCFE, an open surgical approach such as the (modified) Dunn osteotomy is indicated, with only low incidence of avascular necrosis of the femoral head [15, 36–38], or other inter- or subtrochanteric osteotomies [39].
It has been reported in the literature that patients with SCFE seem to have a higher incidence of acetabular and femoral retroversion, coxa profunda and reduced femoral head–neck offset [40, 41]. Hence, femoral head–neck deformity due to SCFE may only be a co-factor in such patients, resulting in symptomatic FAI [5]. Osteochondroplasty might therefore not be sufficient to prevent further acetabular cartilage and labral injury in all patients and additional interventions might be indicated [42]. Further studies need to be performed.
In conclusion, cam impingement deformity is found in patients with mild SCFE and, as in our cohort, is associated with antero-superior cartilage and labral injury. These lesions might be prevented if early osteochondroplasty is performed. Arthroscopic trimming is a safe and efficient surgical option for treating mild SCFE-related FAI, and can restore the α-angle to normal. Whether combined arthroscopic osteochondroplasty with in situ fixation improves long-term hip function and prevents progression of osteoarthritis after SCFE is unknown, and needs to be proven in prospective studies with long-term outcomes. However, in our understanding of FAI and its implications for osteoarthritis, early treatment, especially in patients with SCFE, is crucial to reduce the incidence of labral and acetabular degenerative lesions, and can be performed as two-stage or concomitant surgery after in situ fixation.
References
Novais EN, Millis MB (2012) Slipped capital femoral epiphysis: prevalence, pathogenesis, and natural history. Clin Orthop Relat Res 470(12):3432–3438. doi:10.1007/s11999-012-2452-y
Wabitsch M, Horn M, Esch U, Mayer H, Moss A, Gunther KP, Nelitz M (2012) Silent slipped capital femoral epiphysis in overweight and obese children and adolescents. Eur J Pediatr 171(10):1461–1465. doi:10.1007/s00431-012-1743-3
Goodman DA, Feighan JE, Smith AD, Latimer B, Buly RL, Cooperman DR (1997) Subclinical slipped capital femoral epiphysis. Relationship to osteoarthrosis of the hip. J Bone Joint Surg Am 79(10):1489–1497
Rab GT (1999) The geometry of slipped capital femoral epiphysis: implications for movement, impingement, and corrective osteotomy. J Pediatr Orthop 19(4):419–424
Hosalkar HS, Pandya NK, Bomar JD, Wenger DR (2012) Hip impingement in slipped capital femoral epiphysis: a changing perspective. J Child Orthop 6:161–172
Beck M, Kalhor M, Leunig M, Ganz R (2005) Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 87(7):1012–1018
Leunig M, Casillas MM, Hamlet M, Hersche O, Nötzli H, Slongo T, Ganz R (2000) Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand 71(4):370–375
Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J (2002) The contour of the femoral head–neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 84(4):556–560
Miese FR, Zilkens C, Holstein A, Bittersohl B, Kropil P, Jager M, Mamisch TC, Krauspe R, Modder U, Furst G (2010) MRI morphometry, cartilage damage and impaired function in the follow-up after slipped capital femoral epiphysis. Skeletal Radiol 39(6):533–541. doi:10.1007/s00256-010-0903-7
Fraitzl CR, Kafer W, Nelitz M, Reichel H (2007) Radiological evidence of femoroacetabular impingement in mild slipped capital femoral epiphysis: a mean follow-up of 14.4 years after pinning in situ. J Bone Joint Surg Br 89(12):1592–1596. doi:10.1302/0301-620X.89B12.19637
Fraitzl CR, Käfer W, Nelitz M, Reichel H (2007) Radiological evidence of femoroacetabular impingement in mild slipped capital femoral epiphysis: a mean follow-up of 14.4 years after pinning in situ. J Bone Joint Surg Br 89(12):1592–1596
Fraitzl CR, Nelitz M, Cakir B, Käfer W, Reichel H (2009) Transfixation in slipped capital femoral epiphysis: long-term evidence for femoro-acetabular impingement. Z Orthop Unfall 147(3):334–340
Morakis E, Sink EL (2013) Advances in hip preservation after slipped capital femoral epiphysis. Instr Course Lect 62:415–428
Dragoni M, Heiner AD, Costa S, Gabrielli A, Weinstein SL (2012) Biomechanical study of 16-mm threaded, 32-mm threaded, and fully threaded SCFE screw fixation. J Pediatr Orthop 32(1):70–74. doi:10.1097/BPO.0b013e31823b18dd
Huber H, Dora C, Ramseier LE, Buck F, Dierauer S (2011) Adolescent slipped capital femoral epiphysis treated by a modified Dunn osteotomy with surgical hip dislocation. J Bone Joint Surg Br 93:833–838
Southwick WO (1967) Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J Bone Joint Surg Am 49(5):807–835
Vlachopoulos L, Huber H, Dierauer S, Ramseier LE (2013) Persisting growth after prophylactic single-screw epiphysiodesis in upper femoral epiphysis. J Pediatr Orthop. doi:10.1097/BPO.0000000000000098
Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R (2004) Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res 418:67–73
Pfirrmann CW, Mengiardi B, Dora C, Kalberer F, Zanetti M, Hodler J (2006) Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology 240(3):778–785. doi:10.1148/radiol.2403050767
Beaule PE, Zaragoza E, Motamedi K, Copelan N, Dorey FJ (2005) Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res 23(6):1286–1292
Clohisy JC, Zebala LP, Nepple JJ, Pashos G (2010) Combined hip arthroscopy and limited open osteochondroplasty for anterior femoroacetabular impingement. J Bone Joint Surg Am 92(8):1697–1706. doi:10.2106/JBJS.I.00326
Abraham E, Gonzalez MH, Pratap S, Amirouche F, Atluri P, Simon P (2007) Clinical implications of anatomical wear characteristics in slipped capital femoral epiphysis and primary osteoarthritis. J Pediatr Orthop 27(7):788–795. doi:10.1097/BPO.0b013e3181558c94
Sink EL, Zaltz I, Heare T, Dayton M (2010) Acetabular cartilage and labral damage observed during surgical hip dislocation for stable slipped capital femoral epiphysis. J Pediatr Orthop 30:26–30
Leunig M, Horowitz K, Manner H, Ganz R (2010) In situ pinning with arthroscopic osteoplasty for mild SCFE: a preliminary technical report. Clin Orthop Relat Res 468(12):3160–3167. doi:10.1007/s11999-010-1408-3
Larson AN, Sierra RJ, Yu EM, Trousdale RT, Stans AA (2012) Outcomes of slipped capital femoral epiphysis treated with in situ pinning. J Pediatr Orthop 32(2):125–130. doi:10.1097/BPO.0b013e318246efcb
Dodds MK, McCormack D, Mulhall KJ (2009) Femoroacetabular impingement after slipped capital femoral epiphysis: does slip severity predict clinical symptoms? J Pediatr Orthop 29(6):535–539. doi:10.1097/BPO.0b013e3181b2b3a3
Castaneda P, Ponce C, Villareal G, Vidal C (2013) The natural history of osteoarthritis after a slipped capital femoral epiphysis/the pistol grip deformity. J Pediatr Orthop 33(Suppl 1):S76–S82. doi:10.1097/BPO.0b013e318277174c
Zilkens C, Bittersohl B, Jager M, Miese F, Schultz J, Kircher J, Westhoff B, Krauspe R (2011) Significance of clinical and radiographic findings in young adults after slipped capital femoral epiphysis. Int Orthop 35(9):1295–1301. doi:10.1007/s00264-010-1106-5
Boyer DW, Mickelson MR, Ponseti IV (1981) Slipped capital femoral epiphysis. Long-term follow-up study of one hundred and twenty-one patients. J Bone Joint Surg Am 63(1):85–95
Bellemans J, Fabry G, Molenaers G, Lammens J, Moens P (1996) Slipped capital femoral epiphysis: a long-term follow-up, with special emphasis on the capacities for remodeling. J Pediatr Orthop B 5(3):151–157
Dawes B, Jaremko JL, Balakumar J (2011) Radiographic assessment of bone remodelling in slipped upper femoral epiphyses using Klein’s line and the alpha angle of femoral-acetabular impingement: a retrospective review. J Pediatr Orthop 31(2):153–158. doi:10.1097/BPO.0b013e3182093dc7
Kallio PE, Lequesne GW, Paterson DC, Foster BK, Jones JR (1991) Ultrasonography in slipped capital femoral epiphysis. Diagnosis and assessment of severity. J Bone Joint Surg Br 73(6):884–889
Bedi A, Zaltz I, De La Torre K, Kelly BT (2011) Radiographic comparison of surgical hip dislocation and hip arthroscopy for treatment of cam deformity in femoroacetabular impingement. Am J Sports Med 39(Suppl):20S–28S. doi:10.1177/0363546511412734
de Sa D, Urquhart N, Philippon M, Ye JE, Simunovic N, Ayeni OR (2013) Alpha angle correction in femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2678-6
Brunner A, Horisberger M, Herzog RF (2009) Sports and recreation activity of patients with femoroacetabular impingement before and after arthroscopic osteoplasty. Am J Sports Med 37(5):917–922. doi:10.1177/0363546508330144
Ziebarth K, Zilkens C, Spencer S, Leunig M, Ganz R, Kim YJ (2009) Capital realignment for moderate and severe SCFE using a modified Dunn procedure. Clin Orthop Relat Res 467(3):704–716. doi:10.1007/s11999-008-0687-4
Sankar WN, Vanderhave KL, Matheney T, Herrera-Soto JA, Karlen JW (2013) The modified Dunn procedure for unstable slipped capital femoral epiphysis: a multicenter perspective. J Bone Joint Surg Am 95(7):585–591. doi:10.2106/JBJS.L.00203
Slongo T, Kakaty D, Krause F, Ziebarth K (2010) Treatment of slipped capital femoral epiphysis with a modified Dunn procedure. J Bone Joint Surg Am 92(18):2898–2908. doi:10.2106/JBJS.I.01385
Wiemann JM, Herrera-Soto JA (2013) Can we alter the natural history of osteoarthritis after SCFE with early realignment? J Pediatr Orthop 33(1):83–87
Millis MB, Novais EN (2011) In situ fixation for slipped capital femoral epiphysis: perspectives in 2011. J Bone Joint Surg Am 93(Suppl 2):46–51. doi:10.2106/JBJS.K.00040
Sankar WN, Brighton BK, Kim YJ, Millis MB (2011) Acetabular morphology in slipped capital femoral epiphysis. J Pediatr Orthop 31(3):254–258
Azegami S, Kosuge D, Ramachandran M (2013) Surgical treatment of femoroacetabular impingement in patients with slipped capital femoral epiphysis: a review of current surgical techniques. Bone Joint J 95(4):445–451. doi:10.1302/0301-620X.95B4.30245
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. All authors declare no conflict of interest. Ethical approval was obtained by the local ethical committee and all procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants and their legal guardians to be included in the study.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Tscholl, P.M., Zingg, P.O., Dora, C. et al. Arthroscopic osteochondroplasty in patients with mild slipped capital femoral epiphysis after in situ fixation. J Child Orthop 10, 25–30 (2016). https://doi.org/10.1007/s11832-015-0707-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-015-0707-3