Abstract
Purpose
To compare the patterns of mental health service utilisation between people with and without cancer.
Methods
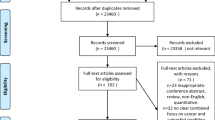
We performed a cross-sectional study using data of all respondents aged ≥ 25 years from the Australian National Study of Mental Health and Wellbeing 2020–2021 conducted during the COVID-19 pandemic. Comparisons were made between the two groups (cancer versus non-cancer) using logistic regression models.
Results
The study comprised 318 people with cancer (55% female) and 4628 people without cancer (54% female). Cancer survivors had a higher prevalence of reporting poor health (38% versus 16%) and mental distress (18% versus 14%) than people without cancer. There were no significant differences between people with and without cancer in the odds of consulting general practitioner, psychiatrist and other health professionals for mental health, although people with cancer were significantly more likely to consult a psychologist than people without cancer (adjusted odds ratio (aOR) = 1.64, 95%CI = 1.05–2.48). While the odds of being hospitalised for physical health was significantly higher in cancer survivors than people without cancer (aOR = 2.32, 95%CI = 1.78–3.01), there was only a negligible number of people reported being hospitalised for mental health between the two groups. Several factors were associated with higher odds of mental health service utilisation including younger age, unpartnered marital status and presence of a current mental condition.
Conclusions
Alarmingly, despite experiencing higher prevalence of poor health status and mental distress, cancer survivors did not utilise more mental health services than the general population. That is, there is a higher degree of untreated, or undertreated, distress in cancer than in the general population.
Implications for Cancer Survivors
Further research to identify optimal approaches of mental health care delivery for cancer survivors are urgently needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mental illness is highly prevalent among people diagnosed with cancer with rates ranging from 20 to 53% [1,2,3,4,5]. Despite multiple studies demonstrating the high disease burden of mental illness in cancer, psychosocial issues remain the most frequently reported unmet needs of cancer survivors, including fear of cancer recurrence; future uncertainty; worry about partners, families and friends; help to cope with stress and sexual changes [6]. This may in part be due to mental health stigma, workforce shortages, limited access and affordability of services and prioritisation of physical over mental health [7,8,9]. Screening and referral of cancer patients for mental distress are not conducted routinely by clinicians despite recommendations of clinical practice guidelines [10]. While several Australian studies have also examined screening [11, 12] and uptake of referrals for psychosocial care [13, 14] in cancer patients, the findings were limited by single-institution experience. Even when services are offered, prior studies have reported low utilisation of mental health services by people with cancer [11, 13, 15, 16]. Further, cancer patients with the highest needs for mental health services appeared to be least likely to be able to afford them [17]. However, given most of these studies were largely conducted in the United States, the generalisability of the findings to other healthcare systems remains to be explored.
We showed in our previous study that Australian cancer survivors utilised health services significantly more than the general population, including outpatient clinics, day admissions and emergency department presentations [18]. Cancer survivors were also more likely to be admitted to hospitals and to consult general practitioners, specialists, nurses and allied health professionals compared with the general population [18]. However, our analysis did not distinguish utilisation rates for mental health services. Mental disorders are frequently reported among people living with cancer in Australia ranging from 16 to 31% [3, 4, 19], but little is known about the patterns and the characteristics associated with healthcare utilisation for mental health in the cancer population. Further, mental well-being of the population as well as the access to health care has been affected by the COVID-19 pandemic [20, 21], but relatively limited data is available to inform the priority for mental health services during a pandemic outbreak.
The Australian National Study of Mental Health and Wellbeing (NSMHW), conducted by the Australian Bureau of Statistics, collected mental health-related information from representative samples of the Australian population to inform mental health policy and development [22]. In the present study, we analysed the most recent NSMHW data conducted during the COVID-19 pandemic to compare (a) patterns of mental health service utilisation and (b) the perceived need for mental health services, between people living with cancer and the general population without cancer. We also examined the characteristics associated with mental health service utilisation.
Methods
Data source
We utilised data from the NSMWH 2020–2021 [22]. The data was collected in the survey, which was conducted between December 2020 and July 2021, with 5554 fully responding participants aged 16–85 years living in private dwellings across all Australian states and territories (response rate: 57%) [22]. The de-identified individual-level data was accessed via the Australian Bureau of Statistics DataLab [23].
Study population
All respondents aged ≥ 25 years who reported having had a history of cancer (whether cancer is current or in remission to reflect the characteristics of the cancer survivorship journey) were identified as the study group of interest (i.e., cancer group refers to ‘people with cancer’), and the remaining participants without a history of cancer were included as the comparison group (i.e., the general population refers to ‘people without cancer’). As the needs for mental health services in adolescent and young adults with cancer (defined as 15–24 years in Australia) [24] are different from adults with cancer, we excluded respondents aged 24 years or younger from the analysis.
Assessment of services for mental health
Participants were asked whether they had access to any services for mental health. We analysed the type of mental health services accessed in the last 12 months before the interview and/or in their lifetime responded by all participants including: (i) consultations for mental health with any health professionals including general practitioner, psychiatrist, psychologist and other health professionals (mental health nurse, other mental health professionals (e.g., social workers and counsellors), specialist doctor or surgeon (e.g., urologists and cardiologist) and others (e.g., pharmacists and dieticians)); (ii) hospitalisation due to physical or mental health; (iii) digital service use over the phone or using digital technology for mental health including crisis support or counselling services, mental health support groups, forums or chat rooms and the use of treatment programs, training, assessments or other tools to improve mental health.
We also analysed the type of help received for mental health in the last 12 months before the interview including: (i) information about mental illness, its treatment and available services; (ii) medicines or tablets; (iii) counselling (e.g., psychotherapy, cognitive behavioural therapy or counselling); (iv) social interventions (e.g., sought help for housing or money problems or to meet other people for support or company) and (v) skills training (e.g., sought help to look after themselves or their home or to improve ability to work or to use time in other ways). Finally, we examined whether the participants’ perceived needs for mental health services were met for each type of help received for mental health in the last 12 months listed above, and we grouped their responses into two categories (not met/partially met versus met/no need).
Participants were also asked as a separate question, whether they had used any mental health or support services (including general practitioners, psychologist, psychiatrist or other mental health specialist, crisis support or counselling services, online mental health information or mental health apps) during COVID-19 pandemic which began in March 2020.
Sociodemographic, chronic health condition and self-assessed health/distress co-variables
We extracted the following information on sociodemographic including sex, age, marital status, country of birth, geographical location (measured by remoteness area using the Australian Statistical Geography Standard 2016 [25] and included major cities, inner regional, outer regional, remote and very remote Australia; we combined outer regional, remote and very remote Australia as ‘other areas’ due to small cell sizes), education level, employment status and socioeconomic status (measured by equivalised household weekly income).
Data on current mental health conditions including depression or anxiety reported by the participants as being told by a doctor or nurse that have lasted, or are expected to last, for 6 months or more was extracted. We also calculated the number of other current chronic health conditions including arthritis, osteoporosis, asthma, dementia, diabetes, heart disease, stroke, chronic kidney disease, bronchitis or emphysema and any other long-term health conditions reported by the participants.
Two measures of self-assessed health and distress were extracted for analysis. The first was self-assessed health status that measured perception of health and rated as excellent, very good, good, fair or poor by the participants; we grouped the measurement into two categories (poor health with a rating of fair/poor versus good health with a rating of excellent/very good/good)) [19]. The second was level of mental distress measured by the Kessler Psychological Distress Scale-10 based on a person’s emotional state in the 4 weeks before survey interview; we grouped the measurement into two categories (low–moderate distress level with a score of 10–21 versus high–very high distress level with a score of 22–50)) [19, 22].
Statistical analysis
The characteristics of the population were summarised using descriptive statistics. Health service utilisation for mental health, the types of help received and the perceived needs of people with and without cancer were compared using logistic regression. The logistic regression analyses were adjusted for sociodemographic characteristics including sex, age, marital status, country of birth, geographical location, education level, employment status and socioeconomic status as well as the number of other long-term chronic health conditions. We also constructed a separate multivariable analysis for the cancer and non-cancer groups to identify characteristics, including sex, age, marital status, country of birth, geographical location, education level, employment status, socioeconomic status, the number of other current long-term chronic health conditions, presence of a current mental health condition, self-assessed health status and level of mental distress, that may be associated with mental health service utilisation in each group. The findings were reported as adjusted odds ratio (aOR) with 95% confidence intervals (CI). Analysis was conducted using R version 4.2.1.
Ethical consideration
We obtained ethics approval from the Flinders University Human Ethics Low Risk Panel (#6298).
Results
Cohort characteristics
The study comprised 318 people with cancer and 4628 people without cancer (Table 1). Relative to people without cancer, people with cancer were older (48% versus 18% aged ≥ 70 years), more likely to be born in Australia (74% versus 67%), live in inner regional/other areas (36% versus 26%), widowed/divorced/separated (38% versus 24%), unemployed (69% versus 36%), have a lower education level (33% versus 27% had no non-school qualification) and a lower socioeconomic status (31% versus 19% in the lowest household income level). Comorbidity was more common in people with cancer (76% versus 51% reported ≥ 1 other health conditions) compared with people without cancer. While the prevalence of mental health conditions was similar between the cancer and non-cancer groups (16% versus 15%), a higher proportion of people with cancer reported a poor health status (38% versus 16%) and a high level of distress (18% versus 14%) than people without cancer.
Health service utilisation for mental health
There were no significant differences between people with and without cancer in the odds of accessing the following services for mental health in the past 12 months: any health professionals, general practitioner, psychiatrist and other health professionals (Table 2). However, people with cancer were significantly more likely to consult a psychologist than people without cancer (aOR = 1.64, 95%CI 1.05–2.48). While the odds of being hospitalised for physical health was significantly higher in people with cancer than people without cancer (aOR=2.32, 95%CI 1.78–3.01), only a negligible number of people reported being hospitalised for mental illness between the two groups. There was also a negligible number of people that used any digital service over phone or digital technology for mental health between the two groups. Similar trends were observed for accessing mental health services in the last 12 months and in their lifetime. No significant differences emerged between people with and without cancer in accessing any mental health or support services during COVID-19 pandemic (aOR = 0.95, 95%CI 0.60–1.43).
Types of help received for mental health and the perceived needs
There were no significant differences between people with and without cancer in the odds of receiving information about mental illness, medicines or tablets, counselling, social interventions and skills training in the last 12 months (Table 3). There were also no significant differences in their perceived mental health needs between the two groups.
Factors associated with mental health service utilisation
Four factors were associated with significant differences in accessing services for mental health in the past 12 months (Table 4): age, marital status, education level and the presence of a current mental condition. People who were younger (versus those aged ≥ 70 years), unpartnered (i.e., being widowed/divorced/separated versus being married) and having a current mental condition (versus no current mental condition) were more likely to access health services for mental health than their respective counterparts in both the cancer and non-cancer groups. People with school-level qualification (versus those with a postgraduate qualification) were less likely to access mental health services in both the cancer and non-cancer group. While a higher level of distress (versus low–moderate distress) was also associated with a higher odds of accessing mental health services, these results reached significance for the non-cancer group only, possibly due to a larger sample size in the non-cancer group. Among the non-cancer group, males (versus females) and those who were born overseas (versus born in Australia) had lower odds of accessing mental health services.
Discussion
This Australian study provided an overview and comparison of the patterns of mental health service utilisation between cancer survivors and the general population. Of concern, despite a higher level of distress and a higher prevalence of poor health status in people with cancer than people without cancer, we found no significant differences in the mental healthcare utilisation for a range of services between the two groups, with the exception of consultation with a psychologist. This suggests relative underutilisation among people with cancer. The services examined included consultations with health professionals, hospitalisations and digital technology as well as help received for mental health covering information, medicines, counselling, social interventions and skills training. There were also no significant differences between people with and without cancer in their perceived needs for mental health services.
Low access to mental health services among cancer survivors may be explained by several reasons including low perceived needs, affordability, mental health stigma, lack of care coordination and workforce shortage [8, 26]. A qualitative study conducted in Australia showed that although the majority of cancer survivors participated in an online survey were aware of the specific mental health treatment plan subsidised by the Australian Government, less than one in five reported having a mental health treatment plan due to low perceived needs for such services [8]. It is also possible that cancer survivors may prioritise their physical over mental health [27]. Our findings showed that while people with cancer were significantly more likely to be admitted to hospital for physical health conditions than people without cancer, only a negligible number of people reported being admitted for mental health issues in both the cancer and non-cancer groups. Other studies found the main reasons for hospital admissions in cancer patients were directly related to cancer diagnosis or due to symptoms or effects of cancer treatment [28,29,30,31,32]. Although cancer-related hospitalisations were common, representing about 11% of all hospitalisations in Australia in 2019–2020 [33], mental health–related hospitalisations were less frequent accounting for about 1% of all same day hospitalisations and 6% of all overnight hospitalisations [34].
The only service more frequently accessed by people with as opposed to without cancer was psychologists. Access and referrals to psychological support may be comparatively easier for those with cancer than the general public as a number of public psycho-oncology services are provided as part of the hospital services and the Cancer Council counselling services [35]. Clinical practice guidelines and pathways such as ‘clinical pathways for the screening, assessment and management of anxiety and depression in adult cancer patients’ [36] would also have a role; it is plausible that routine distress screening may happen more frequently in the cancer care than in other settings, thus generating more referrals, with psychologists being the standard first port-of-call. In contrast, our study found no differences in the odds of accessing other health professionals for mental health between the cancer and non-cancer groups. Development and implementation of clinical practice guidelines and pathways for referrals to other health professionals for management could be of value to improve access to allied mental health care services targeting people who need them most. In Australia, many of the mental health-related care provided by allied health professionals such as psychologists, social workers and occupational therapists were delivered privately and only partially subsidised by the Australian government [8, 18, 37, 38] such as through the Better Access to Mental Health Care initiative [39, 40], GP Mental Health Treatment Plan or Chronic Disease Management Plan and Team Care Arrangements [41]. Cost barriers may thus deter access to mental health services especially among people who are not eligible for the subsidised schemes.
Both public and self-stigma about mental health may also play a part which can impede engagement and access to mental health care [42]. Individuals may not disclose psychiatric and distress symptoms due to stigma surrounding mental illness. Although routine screening for mental distress among cancer patients is being undertaken in some health services in Australia, it is not done systematically [43]. At present, there is no national data available on the rate of mental health screening for distress in cancer patients in Australia [43]. Several barriers to the implementation of screening for distress in cancer care have been identified including workforce shortage, competing demands and lack of training and support on psychosocial issues [44, 45].
While digital service or technology offers the possibility of improving access to mental health services during the COVID-19 pandemic [46, 47], there were no differences in using any online services or program between people with and without cancer in our study. This may have been the reflection of the age structure of our study population as we excluded adolescent and young adults aged 15–24 who are the typical targeted population for digital health interventions [48]. Other possible explanation includes lack of awareness and adoption of digital health services, limited availability of tools, education and training to support the delivery of services, poor digital literacy and the preference for face-to-face services over digital health engagement [49]. Further research and evaluation are needed to understand how digital interventions can be integrated into the broader mental and health system to facilitate their implementation in the Australian setting [49]. While there were changes being made for eligible people to receive rebates for additional individual mental health sessions under the Better Access Pandemic Support measure [50], our study found no significant difference between people with and without cancer in accessing any mental health or support services during COVID-19 pandemic. It is possible that cancer patients may have experienced disruptions in care during pandemic [51, 52] and may choose to prioritise their safety and physical health by attending to required appointments only [53]. While the current Australian data showed an increased in mental health service use among the general population during pandemic [54], further studies to characterise the changes in mental health services use over time on specific patient populations are needed to provide insight into the impact of COVID-19 for planning and projecting future service needs.
Our study found no differences in various types of help received for mental health including medicines for mental health between the cancer and non-cancer groups and provided further data for cross-national comparisons. A systematic review and meta-analysis showed a considerable variation in the use of antidepressants among cancer patients across different settings and regions [55]. For example, studies conducted in the USA and Netherlands showed that cancer survivors were more likely to report taking psychotropic medicines compared with the general population [56, 57], while the use of antidepressants were less common in studies conducted in Asia [55].
Several characteristics were associated with higher mental health service utilisation, including younger age, unpartnered marital status and the presence of a current mental condition in both cancer and non-cancer groups as observed in our study. The implementation of integrated mental health care model [58] especially for patients with a high need for mental health services [59,60,61] such as young adults, being widowed/divorce/separated and having a current mental condition and mental distress, may be of value for improving access to care and health outcomes not only in oncology but also in the general population. Our findings also provide further evidence to support the screening and interventions that target select group of patients who may be at risk of underutilising mental health services such as those with a low education level [60].
Our study has several limitations. The data collected in the survey was self-reported and may subject to recall or response bias. While our study population comprised cancer cases (regardless of whether the cancer is current or in remission) to reflect the journey of cancer survivorship, the sample size was modest and we were not able to differentiate the types or stages of cancer or time from cancer diagnosis as the information was not collected in the survey. The study population also restricted to those living in the private dwellings, excluding people residing in special dwellings such as institutions, nursing homes and boarding houses and the homelessness, which may underestimate the prevalence of mental disorders and health service utilisation for mental health. Nonetheless, our findings provide evidence to inform the development of mental health policy and highlight the need for targeted interventions aim at improving access to mental health services among the Australian population living with cancer.
Conclusion
Alarmingly, despite experiencing higher prevalence of poor health status and mental distress, cancer survivors did not utilise more mental health services than the general population. That is, there is a higher degree of untreated, or undertreated, distress in cancer than in the general population. Further research to identify optimal approaches of mental health care delivery for cancer survivors are urgently needed to overcome the access gap.
Data availability
The analysis was performed using the Australian National Study of Mental Health and Wellbeing detailed microdata. As we are not the data custodians, we are not authorised to make the data available. With the appropriate approvals, the data may be accessed through the Australian Bureau of Statistics.
References
Singer S, Das-Munshi J, Brähler E. Prevalence of mental health conditions in cancer patients in acute care--a meta-analysis. Ann Oncol. 2010;21(5):925–30. https://doi.org/10.1093/annonc/mdp515.
Caruso R, Breitbart W. Mental health care in oncology. Contemporary perspective on the psychosocial burden of cancer and evidence-based interventions. Epidemiol Psychiatr Sci. 2020;29:e86. https://doi.org/10.1017/s2045796019000866.
Ng HS, Roder D, Koczwara B, Vitry A. Comorbidity, physical and mental health among cancer patients and survivors: an Australian population-based study. Asia Pac J Clin Oncol. 2018;14(2):e181–e92. https://doi.org/10.1111/ajco.12677.
Ng HS, Koczwara B, Roder D, Vitry A. Changes in the prevalence of comorbidity in the Australian population with cancer, 2007–2014. Cancer Epidemiol. 2018;54:56–62. https://doi.org/10.1016/j.canep.2018.03.010.
Walker ZJ, Xue S, Jones MP, Ravindran AV. Depression, anxiety, and other mental disorders in patients with cancer in low- and lower-middle-income countries: a systematic review and meta-analysis. JCO Glob Oncol. 2021;7:1233–50. https://doi.org/10.1200/go.21.00056.
Lisy K, Langdon L, Piper A, Jefford M. Identifying the most prevalent unmet needs of cancer survivors in Australia: a systematic review. Asia Pac J Clin Oncol. 2019;15(5):e68–78. https://doi.org/10.1111/ajco.13176.
Purushotham A, Bains S, Lewison G, et al. Cancer and mental health--a clinical and research unmet need. Ann Oncol. 2013;24(9):2274–8. https://doi.org/10.1093/annonc/mdt214.
Gulliver A, Morse AR, Banfield M. Cancer survivors’ experiences of navigating the Australian health care system for physical and mental health care needs. Int J Environ Res Public Health. 2023;20(5):3988.
Carbonell Á, Navarro-Pérez JJ, Mestre MV. Challenges and barriers in mental healthcare systems and their impact on the family: a systematic integrative review. Health Soc Care Community. 2020;28(5):1366–79. https://doi.org/10.1111/hsc.12968.
McCarter K, Britton B, Baker AL, et al. Interventions to improve screening and appropriate referral of patients with cancer for psychosocial distress: systematic review. BMJ Open. 2018;8(1):e017959. https://doi.org/10.1136/bmjopen-2017-017959.
Clover KA, Mitchell AJ, Britton B, Carter G. Why do oncology outpatients who report emotional distress decline help? Psychooncology. 2015;24(7):812–8. https://doi.org/10.1002/pon.3729.
Linehan K, Fennell KM, Hughes DL, Wilson CJ. Use of the distress thermometer in a cancer helpline context: can it detect changes in distress, is it acceptable to nurses and callers, and do high scores lead to internal referrals? Eur J Oncol Nurs. 2017;26:49–55. https://doi.org/10.1016/j.ejon.2016.12.005.
Curry C, Cossich T, Matthews JP, et al. Uptake of psychosocial referrals in an outpatient cancer setting: improving service accessibility via the referral process. Support Care Cancer. 2002;10(7):549–55. https://doi.org/10.1007/s00520-002-0371-2.
Skaczkowski G, Sanderson P, Shand M, et al. Factors associated with referral offer and acceptance following supportive care problem identification in a comprehensive cancer service. Eur J Cancer Care (Engl). 2018;27(5):e12869. https://doi.org/10.1111/ecc.12869.
Salm S, Blaschke K, Ihle P, et al. Mental disorders and utilization of mental health services in newly diagnosed cancer patients: an analysis of German health insurance claims data. Psychooncology. 2021;30(3):312–20. https://doi.org/10.1002/pon.5579.
Kadan-Lottick NS, Vanderwerker LC, Block SD, et al. Psychiatric disorders and mental health service use in patients with advanced cancer: a report from the coping with cancer study. Cancer. 2005;104(12):2872–81. https://doi.org/10.1002/cncr.21532.
Arega MA, Dee EC, Muralidhar V, et al. Psychological distress and access to mental health services among cancer survivors: a National Health Interview Survey Analysis. J Gen Intern Med. 2021;36(10):3243–5. https://doi.org/10.1007/s11606-020-06204-3.
Ng HS, Koczwara B, Roder D, et al. Patterns of health service utilisation among the Australian population with cancer compared with the general population. Aust Health Rev. 2020;44(3):470–9. https://doi.org/10.1071/ah18184.
Ng HS, Woodman R, Koczwara B. Health status and mental distress in people with cancer and comorbid conditions: the Australian National Health Survey analysis. Cancer Med. 2023; https://doi.org/10.1002/cam4.6291.
van de Poll-Franse LV, de Rooij BH, Horevoorts NJE, et al. Perceived care and well-being of patients with cancer and matched norm participants in the COVID-19 crisis: results of a survey of participants in the Dutch PROFILES Registry. JAMA Oncol. 2021;7(2):279–84. https://doi.org/10.1001/jamaoncol.2020.6093.
Wang Y, Duan Z, Ma Z, et al. Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic. Transl Psychiatry. 2020;10(1):263. https://doi.org/10.1038/s41398-020-00950-y.
Australian Bureau of Statistics. National Study of Mental Health and Wellbeing methodology 2022. https://www.abs.gov.au/methodologies/national-study-mental-health-and-wellbeing-methodology/2020-21. Accessed 2 Jul 2023.
Australian Bureau of Statistics. DataLab 2023. https://www.abs.gov.au/statistics/microdata-tablebuilder/datalab. Accessed 3 Jul 2023.
Australian Institute of Health and Welfare. Cancer in adolescents and young adults in Australia 2018. https://www.aihw.gov.au/reports/cancer/cancer-adolescents-young-adults/summary. Accessed 3 Jul 2023.
Australian Bureau of Statistics. Remoteness structure australian statistical geography standard (ASGS) Edition 3 2021. https://www.abs.gov.au/statistics/standards/australian-statistical-geography-standard-asgs-edition-3/jul2021-jun2026/remoteness-structure. Accessed 12 Sept 2023.
Niazi S, Vargas E, Spaulding A, et al. Barriers to accepting mental health care in cancer patients with depression. Soc Work Health Care. 2020;59(6):351–64. https://doi.org/10.1080/00981389.2020.1769248.
Naughton MJ, Weaver KE. Physical and mental health among cancer survivors: considerations for long-term care and quality of life. N C Med J. 2014;75(4):283–6. https://doi.org/10.18043/ncm.75.4.283.
Numico G, Cristofano A, Mozzicafreddo A, et al. Hospital admission of cancer patients: avoidable practice or necessary care? PLos One. 2015;10(3):e0120827. https://doi.org/10.1371/journal.pone.0120827.
Numico G, Zanelli C, Ippoliti R, et al. The hospital care of patients with cancer: a retrospective analysis of the characteristics of their hospital stay in comparison with other medical conditions. Eur J Cancer. 2020;139:99–106. https://doi.org/10.1016/j.ejca.2020.08.023.
McKenzie H, Hayes L, White K, et al. Chemotherapy outpatients’ unplanned presentations to hospital: a retrospective study. Support Care Cancer. 2011;19(7):963–9. https://doi.org/10.1007/s00520-010-0913-y.
Feliciana Silva F, da Silva M, Bonfante G, Reis IA, et al. Hospitalizations and length of stay of cancer patients: a cohort study in the Brazilian Public Health System. PLoS One. 2020;15(5):e0233293. https://doi.org/10.1371/journal.pone.0233293.
Saxena A, Rubens M, Ramamoorthy V, et al. Hospitalization rates for complications due to systemic therapy in the United States. Sci Rep. 2021;11(1):7385. https://doi.org/10.1038/s41598-021-86911-x.
Australian Institute of Health and Welfare. Cancer 2022. https://www.aihw.gov.au/reports/australias-health/cancer. Accessed 3 Jul 2023.
Australian Institute of Health and Welfare. Mental health - admitted patients mental health-related care 2023. https://www.aihw.gov.au/mental-health/topic-areas/admitted-patients. Accessed 3 Jul 2023.
Butow P, Dhillon H, Shaw J, Price M. Psycho-oncology in Australia: a descriptive review. Biopsychosoc Med. 2017;11:15. https://doi.org/10.1186/s13030-017-0100-1.
Butow P, Price MA, Shaw JM, et al. Clinical pathway for the screening, assessment and management of anxiety and depression in adult cancer patients: Australian guidelines. Psychooncology. 2015;24(9):987–1001. https://doi.org/10.1002/pon.3920.
Australian Institute of Health and Welfare. Medicare-subsidised mental health-specific services 2023. https://www.aihw.gov.au/mental-health/topic-areas/medicare-subsisded-services. Accessed 3 Jul 2023.
Australian Government Services Australia. Mental health care and Medicare 2023. https://www.servicesaustralia.gov.au/mental-health-care-and-medicare?context=60092. Accessed 3 Jul 2023.
Australian Government Department of Health and Aged Care. Better Access initiative 2023. https://www.health.gov.au/our-work/better-access-initiative. Accessed 3 Jul 2023.
Australian Government Services Australia. Better access initiative - supporting mental health care 2023. https://www.servicesaustralia.gov.au/better-access-initiative-supporting-mental-health-care?context=20. Accessed 3 Jul 2023.
Australian Government Services Australia. Chronic disease GP Management Plans and Team Care Arrangements 2022. https://www.servicesaustralia.gov.au/chronic-disease-gp-management-plans-and-team-care-arrangements?context=20. Accessed 3 Jul 2023.
Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help seeking, and public health programs. Am J Public Health. 2013;103(5):777–80. https://doi.org/10.2105/ajph.2012.301056.
Cancer Australia. National Cancer Control Indicators: screening for distress 2023. https://ncci.canceraustralia.gov.au/psychosocial-care/screening-distress. Accessed 3 Jul 2023.
Rivest J, Desbeaumes Jodoin V, Fitch M, et al. Screening for distress in cancer care: How to overcome barriers after unsuccessful implementation? Palliat Support Care. 2022;20(1):1–3. https://doi.org/10.1017/s1478951521001759.
Knies AK, Jutagir DR, Ercolano E, et al. Barriers and facilitators to implementing the commission on cancer's distress screening program standard. Palliat Support Care. 2019;17(3):253–61. https://doi.org/10.1017/s1478951518000378.
Scott S, Knott V, Finlay-Jones AL, Mancini VO. Australian psychologists experiences with digital mental health: a qualitative investigation. J Technol Behav Sci. 2022:1–11. https://doi.org/10.1007/s41347-022-00271-5.
Lattie EG, Stiles-Shields C, Graham AK. An overview of and recommendations for more accessible digital mental health services. Nat Rev Psychol. 2022;1(2):87–100. https://doi.org/10.1038/s44159-021-00003-1.
Garrido S, Millington C, Cheers D, et al. What works and what doesn’t work? A systematic review of digital mental health interventions for depression and anxiety in young people. Front Psychiatry. 2019;10:759. https://doi.org/10.3389/fpsyt.2019.00759.
Australian Government Department of Health and Aged Care. Scoping and development of a National Digital Mental Health Framework - final report 2021. https://www.health.gov.au/resources/publications/scoping-and-development-of-a-national-digital-mental-health-framework-final-report. Accessed 3 Jul 2023.
Australian Government Department of Health. MBS factsheet for Practitioners 2022. http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/content/240DC3AF97EEAF79CA2585BC00827909/$File/Factsheet-additional-10-Practitioners.v4.30.06.22.pdf. Accessed 3 Jul 2023.
Treiman K, Kranzler EC, Moultrie R, et al. Patients’ experiences with cancer care: impact of the COVID-19 pandemic. J Patient Exp. 2022;9:23743735221092567. https://doi.org/10.1177/23743735221092567.
Patt D, Gordan L, Diaz M, et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform. 2020;4:1059–71. https://doi.org/10.1200/CCI.20.00134.
Milch V, Wang R, Der Vartanian C, et al. Cancer Australia consensus statement on COVID-19 and cancer care: embedding high value changes in practice. Med J Aust. 2021;215(10):479–84. https://doi.org/10.5694/mja2.51304.
Australian Institute of Health and Welfare. Mental health services activity monitoring quarterly data 2023. https://www.aihw.gov.au/mental-health/monitoring/mental-health-services-activity-monitoring. Accessed 12 Sept 2023.
Sanjida S, Janda M, Kissane D, et al. A systematic review and meta-analysis of prescribing practices of antidepressants in cancer patients. Psychooncology. 2016;25(9):1002–16. https://doi.org/10.1002/pon.4048.
Hawkins NA, Soman A, Buchanan Lunsford N, et al. Use of medications for treating anxiety and depression in cancer survivors in the United States. J Clin Oncol. 2017;35(1):78–85. https://doi.org/10.1200/jco.2016.67.7690.
Ng CG, Boks MP, Smeets HM, et al. Prescription patterns for psychotropic drugs in cancer patients; a large population study in the Netherlands. Psychooncology. 2013;22(4):762–7. https://doi.org/10.1002/pon.3056.
Deshields T, Asvat Y. The case for accelerating integrated mental health care in the cancer setting. JCO Oncol Pract. 2023;19(5):231–3. https://doi.org/10.1200/op.22.00840.
DiNapoli EA, Cully JA, Wayde E, et al. Age as a predictive factor of mental health service use among adults with depression and/or anxiety disorder receiving care through the Veterans Health Administration. Int J Geriatr Psychiatry. 2016;31(6):575–82. https://doi.org/10.1002/gps.4362.
Rana RH, Alam K, Gow J, Ralph N. Predictors of health care use in Australian cancer patients. Cancer Manag Res. 2019;11:6941–57. https://doi.org/10.2147/cmar.S193615.
Hsu T-L, Barrett AE. The association between marital status and psychological well-being: variation across negative and positive dimensions. J Fam Issues. 2020;41(11):2179–202. https://doi.org/10.1177/0192513x20910184.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data analysis was performed by Huah Shin Ng. The first draft of the manuscript was written by Huah Shin Ng and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
We obtained ethics approval from the Flinders University Human Ethics Low Risk Panel (#6298).
Competing interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ng, H.S., Koczwara, B. & Beatty, L. Patterns of mental health service utilisation in people with cancer compared with people without cancer: analysis of the Australian National Study of Mental Health and Wellbeing. J Cancer Surviv (2023). https://doi.org/10.1007/s11764-023-01472-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11764-023-01472-4