Abstract
Purpose
The aim of this study is to assess mental health services utilization and expenditures associated with cancer history using a nationally representative sample in the US.
Methods
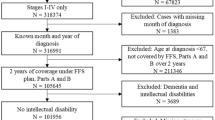
We used data from the 2008–2011 Medical Expenditure Panel Survey and multivariate regression models to assess mental health services use and expenditures among cancer survivors compared to individuals without a cancer history, stratified by age (18–64 and ≥65 years) and time since diagnosis (≤1 vs. >1 year).
Results
Among adults aged 18–64, compared with individuals without a cancer history, cancer survivors were more likely to screen positive for current psychological distress and depression regardless of time since diagnosis; survivors diagnosed >1 year ago were more likely to use mental health prescription drugs; those diagnosed within 1 year reported significantly lower annual per capita mental health drug expenditure and out-of-pocket mental health expenditure, while those diagnosed >1 year presented significantly higher annual per capita mental health expenditure. No significant differences in mental health expenditures were found among adults aged 65 or older.
Conclusions
Mental health problems presented higher health and economic burden among younger and longer-term survivors than individuals without a cancer history. This study provides data for monitoring the impact of initiatives to enhance coverage and access for mental health services at the national level.
Implications for cancer survivors
Early detection and appropriate treatment of mental health problems may help improve quality of cancer survivorship.
Similar content being viewed by others
References
Adler N, Page A, eds. Cancer Care for the Whole Patient: meeting Psychosocial Healthcare Needs. Washington DC: Institute of Medicine (IOM). 2008.
Hewitt M, Greenfield S, Stovell E, editors. From cancer patient to cancer survivor: lost in transition. Washington DC: National Academies Press; 2006.
Holland J, Weiss T. The new standard of quality cancer care: integrating the psychosocial aspects in routine cancer from diagnosis through survivorship. Cancer J. 2008;14:425–8.
Findley PA, Sambamoorthi U. Preventive health services and lifestyle practices in cancer survivors: a population health investigation. J Cancer Surviv. 2009;3:43–58.
Butler L, Downe-Wamboldt B, Melanson P, et al. Prevalence, correlates, and costs of patients with poor adjustment to mixed cancers. Cancer Nurs. 2006;29:9–16.
Lutgendorf SK, Sood AK, Antoni MH. Host factors and cancer progression: biobehavioral signaling pathways and interventions. J Clin Oncol. 2010. doi:10.1200/JCO.2009.26.9357.
Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: a meta-analysis. Cancer. 2009;115:5349–61.
Mols F, Husson O, Roukema JA, van de Poll-Franse LV. Depressive symptoms are a risk factor for all-cause mortality: results from a prospective population-based study among 3,080 cancer survivors from the PROFILES registry. J Cancer Surviv. 2013;7(3):484–92.
Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004;32:57–71.
Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160–74.
Earle CC, Neville BA, Fletcher R. Mental health service utilization among long-term cancer survivors. J Cancer Surviv. 2007;1:156–60.
Kaiser NC, Hartoonian N, Owen JE. Toward a cancer-specific model of psychological distress: population data from the 2003–2005 National Health Interview Surveys. J Cancer Surviv-Res Pract. 2010;4:291–302.
Siegel R, DeSantis C, Virgo K, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62:220–41.
Parry C, Kent EE, Mariotto AB, et al. Cancer survivors: a booming population. Cancer Epidemiol Biomarkers Prev. 2011;20:1996–2005.
Pincus HA, Tanielian TL, Marcus SC, et al. Prescribing trends in psychotropic medications: primary care, psychiatry, and other medical specialties. JAMA. 1998;279:526–31.
Zuvekas SH. Trends in mental health services use and spending, 1987–1996. Health Aff (Millwood). 2001;20:214–24.
Carlson LE, Bultz BD. Benefits of psychosocial oncology care: improved quality of life and medical cost offset. Health Qual Life Outcomes. 2003;1:8.
Carlson LE, Bultz BD. Efficacy and medical cost offset of psychosocial interventions in cancer care: making the case for economic analyses. Psychooncology. 2004;13:837–49. discussion 850–836.
Gordon LG, Beesley VL, Scuffham PA. Evidence on the economic value of psychosocial interventions to alleviate anxiety and depression among cancer survivors: a systematic review. Asia Pac J Clin Oncol. 2011;7:96–105.
Hewitt M, Rowland JH. Mental health service use among adult cancer survivors: analyses of the National Health Interview Survey. J Clin Oncol. 2002;20:4581–90.
Punekar RS, Short PF, Moran JR. Use of psychotropic medications by US cancer survivors. Psychooncology. 2011; 10:1002/pon.2039.
Zuvekas SH. Prescription drugs and the changing patterns of treatment for mental disorders, 1996–2001. Health Aff (Millwood). 2005;24:195–205.
Erikson C, Schulman S, Kosty M, et al. Oncology workforce: results of the ASCO 2007 Program Directors Survey. J Oncol Pract. 2009;5:62–5.
Mariotto AB, Yabroff KR, Shao Y, et al. Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst. 2011;103:117–28.
Short PF, Moran JR, Punekar R. Medical expenditures of adult cancer survivors aged <65 years in the United States. Cancer. 2011;117:2791–800.
Helf M, Mahon SM, Eden KD, et al. Screening for skin cancer. Am J Pub Health. 2001;20(Supp1):47–58.
Yabroff KR, Lawrence WF, Clauser S, et al. Burden of illness in cancer survivors: findings from a population-based national sample. J Natl Cancer Inst. 2004;96:1322–30.
Bradley CJ, Bednarek HL. Employment patterns of long-term cancer survivors. Psychooncology. 2002;11:188–98.
Hewitt M, Rowland JH, Yancik R. Cancer survivors in the United States: age, health, and disability. J Gerontol A Biol Sci Med Sci. 2003;58:82–91.
Brown ML, Riley GF, Schussler N, Etzioni R. Estimating health care costs related to cancer treatment from SEER-Medicare data. Med Care. 2002;40(8 Suppl):IV-104–17.
Bradley CJ, Neumark D, Luo Z, Schenk M. Employment and cancer: findings from a longitudinal study of breast and prostate cancer survivors. Cancer Invest. 2007;25:47–54.
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–92.
Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–76.
Manning, WG., Morris, CN, Newhouse, JP. A two-part model of the demand for medical care: preliminary results from the Health Insurance Study. In: van der Gaag, J., Perlman, M. (Eds.), Health, Economics, and Health Economics. North Holland, Amsterdam; 1981. p. 103–123.
Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24:465–88.
Graubard BI, Korn EL. Predective margins with survey data. Biometrics. 1999;55:652–9.
Hoffman KE, McCarthy EP, Recklitis CJ, et al. Psychological distress in long-term survivors of adult-onset cancer: results from a national survey. Arch Intern Med. 2009;169:1274–81.
National Comprehensive Cancer Network. NCCN practice guidelines in oncology: Distress management. v.1.2010. http://www.oralcancerfoundation.org/treatment/pdf/distress-2008.pdf. Accessed 04/28/14
Acknowledgments
No funding was obtained for this study. We appreciate the thoughtful comments from five anonymous reviewers. This manuscript has been presented as a poster at the Academy Health Annual Research Meeting in Orlando, FL 2012.
Disclaimer
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflict of interest
No potential conflicts exist. Chenghui Li is a paid consult for eMax Heath Systems on unrelated studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, C., Li, C., Forsythe, L. et al. Mental health services utilization and expenditures associated with cancer survivorship in the United States. J Cancer Surviv 9, 50–58 (2015). https://doi.org/10.1007/s11764-014-0392-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-014-0392-0