Abstract
Background
As the number of breast cancer survivors increases, the long term consequences of breast cancer treatment are gaining attention. Sexual dysfunction is a common complaint amongst breast cancer survivors, and there are few evidence based recommendations and even fewer well designed clinical trials to establish what treatments are safe or effective in this patient population.
Design
We conducted a PubMed search for articles published between 1995–2009 containing the terms breast cancer, sexual dysfunction, libido, vaginal dryness, testosterone, and vaginal estrogen. We initially reviewed articles focusing exclusively on sexual issues in breast cancer patients. Given the paucity of clinical trials addressing sexual issues in breast cancer patients, we also included studies evaluating both hormone and non-hormone based interventions for sexual dysfunction in post-menopausal women in general.
Conclusions
Among breast cancer survivors, vaginal dryness and loss of libido represent some of the most challenging long term side effects of breast cancer treatment. In the general post-menopausal population, topical preparations of estrogens and testosterone both appear to improve sexual function; however there are conflicting reports about the efficacy and safety of these interventions in women with a history of breast cancer, and further research is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over 200,000 new cases of breast cancer are diagnosed each year in the United States. Many breast cancer patients receive multi-modality therapy including surgery, chemotherapy, and hormonal therapy which cure disease or prolong life, but the long term side effects of these treatments can significantly impact quality of life. As many women diagnosed with breast cancer today will be long-term survivors of their disease, the long-term impact of therapy on emotional and physical well-being has become a growing topic for research. Sexual dysfunction following breast cancer treatment has recently received more attention as a side effect of therapy requiring effective and safe intervention. This paper will focus on existing data regarding the causes and potential treatments of sexual adverse events that contribute to sexual dysfunction, including vaginal dryness, loss of libido, body image issues, and the use of antidepressants.
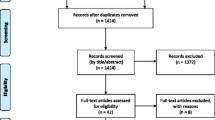
Systematic review methods
In this systematic review, we sought to answer the question “What is the available evidence to support the use of either hormone or non-hormone based therapies for the treatment of vaginal dryness, decreased libido, and other forms of sexual dysfunction in breast cancer patients?” We conducted a PubMed search for articles in humans published in English between 1995–2009 containing the term “breast cancer” along with any of the following terms: sexual dysfunction, vaginal dryness, libido, testosterone, and vaginal estrogen. Using this search strategy, we found a total over 1140 articles. We then searched within these articles to identify cohort and survey studies or clinical trials that addressed any component of sexual dysfunction in breast cancer patients. Given the paucity of clinical trials addressing sexual issues in breast cancer patients, we also included studies evaluating both hormone and non-hormone based interventions for sexual dysfunction in post-menopausal women in general.
Sexual dysfunction in breast cancer patients: effect of systemic therapy and antidepressants
There is a growing body of literature suggesting that sexual dysfunction is a common and distressing problem experienced by many breast cancer survivors. Sexual issues identified in breast cancer survivors include changes in body image associated with the loss of a breast or weight gain, decreased libido, vaginal dryness, and dyspareunia, difficulty with arousal and orgasm, and concern over fertility. Among sexually active and recurrence free breast cancer patients who had completed surgery, chemotherapy, and radiation therapy, 64% percent of the women reported an absence of sexual desire, 38% suffered from dyspareunia, and 42% experienced lubrication problems [1]. In another study of breast cancer survivors, sexual dysfunction occurred more frequently in women who had received chemotherapy and in younger women who were no longer menstruating [2]. Among breast cancer survivors who were an average of 4.4 years since diagnosis, sexual functioning was significantly poorer than that of published normal controls in all areas but desire [3]. In these patients, relationship distress was a significant variable affecting arousal, orgasm, lubrication, sexual satisfaction, and sexual pain. Depression was an important determinant of lower sexual desire, and survivors on antidepressants had greater problems with arousal and achieving orgasm. Burwell et al. examined features of sexual dysfunction in 209 sexually active breast cancer patients (≤ 50 years), and in a multivariate analyses, vaginal dryness and lower perceived sexual attractiveness were associated with greater overall sexual dysfunction. Women who became post-menopausal after chemotherapy reported more sexual problems than those without a menopausal transition [4].
Vaginal dryness and dyspareunia have been found to be prevalent in young breast cancer survivors [5], and studies have shown that vaginal dryness is one of the most important predictors of sexual functioning for women with breast cancer [6, 7]. In a study examining symptoms among a multi-ethnic breast cancer patient population, vaginal dryness was the symptom that rated as the highest unmet need [8]. Loss of libido and inability to become aroused and achieve orgasm are also common complaints among breast cancer patients [7, 9]. There are multiple reasons for these problems including changes in estrogen and androgen levels, preoccupation with and stress related to a breast cancer diagnosis, and use of medications that are associated with sexual dysfunction.
Antidepressants
Antidepressants, especially selective serotonin reuptake inhibitors (SSRIs) and venlafaxine, are frequently associated with sexual dysfunction. In a study of 610 women with previously normal sexual function, the overall incidence of sexual dysfunction was 56.9% among women being treated with antidepressants alone or with benzodiazepines [10]. Significant differences in the rates of sexual dysfunction among different antidepressants were noted, with the highest rates associated with the SSRIs including citalopram and paroxetine, and the lowest rates associated with monoamine oxidase inhibitors and atypical tricyclic antidepressants.
Many breast cancer patients use antidepressants not only for mood disturbances, but also at reduced doses for hot flashes. In a placebo controlled trial evaluating venlafaxine as a treatment for hot flashes in breast cancer patients, patients randomized to venlafaxine experienced an increase in libido as measured by a single item on the Beck depression inventory compared to patients randomized to placebo [11]. However, in a subsequent trial comparing a single intramuscular dose of medroxyprogesterone acetate to venlafaxine as treatment for hot flashes in post-menopausal patients with and without a history of breast cancer, treatment with venlafaxine was associated with increased difficulty with orgasm [12].
An interaction between tamoxifen and several SSRIs metabolized by the CYP2D6 enzyme pathway has been identified. Alterations in tamoxifen metabolism, either by certain CYP2D6 polymorphisms or concurrent use of certain antidepressants has been associated with differences in rates of vasomotor symptoms, and more importantly, breast cancer recurrence risk (See recent review [13]). In light of this information, and since many SSRIs are associated with decrease in sexual desire and interference with arousal and orgasm, selection of alternate antidepressants in breast cancer patients with sexual complaints may be warranted. Bupropion, an atypical antidepressant that acts as a norepinephrine and dopamine reuptake inhibitor, and as a nicotinic antagonist was investigated in 26 breast cancer patients [14]. Based on responses to the Arizona Sexual Experience Scale (ASEX), patients reported improvements in sexual function after 4 and 8 weeks of treatment. A randomized trial of bupropion vs. other antidepressants, both at standard and lower doses (similar to those used for hot flash management), would provide valuable information and offer options for breast cancer patients with both depression and sexual dysfunction.
Impact of specific hormonal therapies on gynecologic symptoms and sexual dysfunction
A number of studies have evaluated gynecologic symptoms in breast cancer patients receiving hormonal therapy. In a prospective study of 181 consecutive postmenopausal breast cancer patients starting endocrine treatment, dyspareunia was significantly increased with non-steroidal aromatase inhibitors (AIs) compared to baseline, and patients receiving tamoxifen experienced significant decrease in sexual interest [15]. The quality of life sub-study of the Arimidex, Tamoxifen, Alone or in Combination (ATAC) adjuvant breast cancer trial found that the incidence of vaginal dryness, dyspareunia, and loss of sexual interest in women taking AIs was significant. These symptoms were particularly bothersome in women who experienced acute chemotherapy induced menopause [16]. In the 5 year follow up of this sub-study, vaginal discharge was less frequently bothersome with anastrozole than tamoxifen (1.2% vs. 5.2%) but vaginal dryness (18.5% vs. 9.1%), dyspareunia (17.3% vs. 8.1%), and reduced libido (34.0% vs. 26.1%) were all more common with anastrozole compared with tamoxifen [17]. In the quality of life sub-study for the Intergroup Exemestane Study (IES), loss of libido was common and did not differ between groups receiving tamoxifen for 5 years compared to those patients who switched over to exemestane after 2–3 years of tamoxifen. There were no differences between the tamoxifen or exemestane groups for vaginal dryness, discomfort with intercourse, and vaginal irritation [18].
Even in patients without a diagnosis of breast cancer, hormonal therapies appear to have an impact on sexual function. Analysis of quality of life data from the Study of Raloxifene and Tamoxifen (STAR) prevention trial found that a higher percentage of women randomized to the tamoxifen arm remained sexually active compared to women in the raloxifene arm. Among sexually active participants, women randomized to the raloxifene group experienced significantly more dyspareunia, greater difficulties with sexual interest, sexual arousal, and sexual enjoyment, but no significant difference in the ability to experience an orgasm [19].
Management of urogenital atrophy in post menopausal women without breast cancer
In the setting of estrogen deprivation, the mucosal and stromal tissues of the vagina, urethra, and trigone of the bladder undergo atrophy, resulting in decreased tissue elasticity and fluid secretion. This may lead to symptomatic vaginal dryness and irritation as well as dyspareunia. Estrogen deprivation also leads to an elevation in vaginal pH which may increase the risk of vaginal and urinary tract infections. Review of the literature on management of vaginal symptoms in post-menopausal women (most without a history of breast cancer) identifies several therapies that appear to be effective in improving vaginal dryness and decreasing dyspareunia.
The twenty-five microgram 17 beta-estradiol vaginal tablet (Vagifem) was compared to 1.25-mg conjugated equine estrogen vaginal cream (Premarin Vaginal Cream) for the relief of atrophic vaginitis in post-menopausal women [20]. Both treatments provided equivalent relief of the symptoms of atrophic vaginitis based on composite scores of vaginal symptoms (dryness, soreness, and irritation). At weeks 2, 12, and 24, increases in serum estradiol concentrations and suppression of follicle-stimulating hormone (FSH) were observed in significantly more patients who were using the vaginal cream than in those who were using the vaginal tablets (p < 0.001). Vaginal tablet therapy resulted in greater patient acceptance and lower withdrawal rates compared with vaginal cream therapy. In a double-blind placebo-controlled, 1612 post-menopausal patients with urogenital complaints were randomized to receive the Vagifem insert or placebo tablet once a day over a period of 2 weeks, and then twice a week for a total of the 12 months [21]. The overall success rates of Vagifem vs. placebo on subjective and objective symptoms of vaginal atrophy were 85.5%, and 41.4%, respectively. A significant improvement of urinary atrophy symptoms was also seen in the Vagifem treated group as compared with the beginning of the study (51.9% vs. 15.5%, p = 0.001). Compared to baseline evaluations, therapy with the Vagifem insert did not raise serum 17β-estradiol levels or stimulate endometrial growth based on mean endometrial thickness.
A slow release estradiol vaginal ring (Estring) has been compared to a topical estriol cream (Synapause®) in a 12 week treatment study in postmenopausal women. The Estring was found to be well tolerated, produced equivalent results in reducing vaginal symptoms, and was preferred by patients as less messy and easier to use [22]. Clinical trials with Estring have shown that there is minimal systemic absorption of estradiol and the range of serum estradiol levels measured at various time points fell within the post-menopausal range [23]. A prospective randomized study compared the Estring to the Vagifem insert for relief of estrogen deficiency symptoms in post menopausal women over a period of 12 months [24]. The primary endpoint was endometrial safety based on the results of ultrasound measurement of endometrial thickness and the proportion of subjects who experienced vaginal bleeding or spotting after a progestogen challenge test. Efficacy was determined by changes in patient reported urogenital estrogen deficiency symptoms including vaginal dryness, vulvar pruritus, dyspareunia, dysuria, and urinary urgency and frequency. Evaluation of vaginal epithelial atrophy including pallor, petechiae, friability, and vaginal dryness was also performed by the investigators who graded each between 0 and 4. There was no statistical difference between the groups in the alleviation of symptoms and signs of urogenital estrogen deficiency, and after 48 weeks of treatment, there was no statistically significant difference in endometrial thickness between the two groups. Estradiol and total estrone serum levels increased during treatment in both groups but remained within the postmenopausal range.
Safety of vaginal estrogen preparations in breast cancer patients
While the intravaginal estrogen preparations (creams, tablet inserts, and rings) are all reasonably effective in many post-menopausal patients, the level of systemic estrogen absorption is variable. One small study has raised concerns about a rapid rise in serum estradiol levels with the use of the Vagifem insert in post-menopausal breast cancer patients on aromatase inhibitors [25]. Serum estradiol, follicle stimulating hormone (FSH), and luteinizing hormone (LH) levels were measured serially in seven postmenopausal women using the Vagifem insert while being treated with AIs for early stage breast cancer. Serum estradiol levels, as measured by an assay specifically developed for measuring low levels in postmenopausal women, rose from baseline levels ≤ 5 pmol/l to a mean 72 pmol/l at 2 weeks into Vagifem treatment. By 4 weeks estradiol levels had decreased to <35 pmol/l in the majority (median 16 pmol/l) although two women continued to have further rise in estradiol levels. The authors concluded that Vagifem significantly raises systemic estradiol levels, at least early in the course of treatment for vaginal atrophy. The authors also offered the opinion that this reversal of estradiol suppression is contraindicated in women being treated with AIs for breast cancer.
Tibolone
Tibolone is a synthetic steroid that has been classified as a selective tissue estrogenic activity regulator (STEAR). It is currently approved in Europe and other countries outside the United States to treat menopausal symptoms and osteoporosis. Tibolone is converted into three metabolites which have varying effects in different tissues due to site-selective enzyme regulation and/or receptor binding and activation. Data suggests that tibolone does not stimulate the breast due to effects on local enzyme activity that inhibit formation of active estrogens [26]. Studies in cell lines suggest that tibolone decreases proliferation rate and increases differentiation and apoptosis [27].
Because of its preclinical biological behavior and safety profile, tibolone has been studied in a number of trials to alleviate post-menopausal symptoms. In an open-label non-randomized trial of 113 post-menopausal women, treatment with tibolone over a 6 year period reversed vaginal atrophy and relieved symptoms including vaginal dryness, dyspareunia, and urinary symptoms compared to no treatment in matched voluntary controls [28]. In the LIFT (Long term Intervention on Fractures with Tibolone ) trial , tibolone at a dose of 1.25 mg per day was compared to placebo in 4538 post-menopausal women with osteoporosis and without a history of cancer in the 5 years prior to enrollment [29]. This trial was closed early when the tibolone group, during 34 months of median follow up, was found to have increased risk of stroke compared to the placebo group. The tibolone group did experience a decreased risk of vertebral and non-vertebral fractures and interestingly also had a significantly decreased risk of invasive breast cancer and colon cancer.
A prospective randomized trial evaluated the safety of tibolone 2.5 mg/day (Livial®) compared to placebo in over 3100 breast cancer patients with vasomotor symptoms. At study entry, 67% of women were taking tamoxifen while only 6.5% women were taking aromatase inhibitors. In May 2007, the independent Data Safety Monitoring Board recommended early termination of the trial due to an excess of breast cancer recurrences in the tibolone arm [30]. After a median follow-up of 3.1 years, 15.2% women on tibolone experienced a cancer recurrence, compared with 10.7% on placebo (HR 1.40; p = 0.001) [31]. No difference was observed between tibolone and placebo in regard to other safety outcomes including mortality, cardiovascular events, or gynecological cancers. Vasomotor symptoms and bone-mineral density improved significantly with tibolone. Based on the results of this trial, tibolone does not appear to be a safe option for management of hot flashes or vaginal symptoms in breast cancer patients. It is intriguing, however, that the lower dose of tibolone tested in the LIFT trial resulted in a reduction in breast cancer risk among osteoporotic women without a recent history of cancer. Whether a lower dose tibolone might be safe in breast cancer patients is unknown.
Non-hormonal and educational interventions to improve vaginal dryness and sexual function in breast cancer patients
The non-hormonal polycarbophil-based vaginal moisturizer Replens was compared to a placebo lubricating agent in small double-blind, crossover, randomized clinical trial of breast cancer patients. Vaginal dryness and dyspareunia showed similar improvement in both the Replens and the placebo arms [32]. Studies comparing Replens to topical estrogen creams in postmenopausal patients without a breast cancer history demonstrated similar benefits in vaginal dryness and dyspareunia with Replens and vaginal estrogen creams [33, 34], but comparison of hormonal and non-hormonal agents have not been made in breast cancer patients.
A 6 week randomized psycho-educational group intervention was tested among breast cancer patients who reported persistent problems in body image, sexual function or partner communication 1–5 years after diagnosis [35]. Patients with severe depression or significant relationship issues were excluded. Patients randomized to the intervention were offered the opportunity to attend six 2 hour sessions aimed at improving satisfaction with sexual functioning and intimate relationships by providing information, enhancing communication skills and reducing anxiety in intimate situations. Control patients received a general pamphlet for breast cancer survivors. Patients randomized to the intervention group reported improvements in relationship adjustment and increased satisfaction with sex compared to controls.
Relationship between testosterone, breast cancer risk, and sexual function
In humans, the adrenal glands and the ovaries represent the main sources of circulating androgens in women. The adrenal steroid dehydroepiandrosterone (DHEA) represents the crucial precursor of human sex steroid biosynthesis. DHEA and its sulfate ester (DHEAS) are the most abundant steroids in the human circulation. DHEA of adrenal origin may be converted to testosterone within the postmenopausal ovary. Removal of the ovaries, even in a post-menopausal patient, may alter testosterone levels and have an impact on libido and other aspects of sexual function.
Testosterone can be converted either to dihydrotestosterone (DHT) or it can be aromatized into estrogens. Therefore, an increase in the circulating testosterone pool may be associated with increased estrogen generation within peripheral target tissues of sex steroid action. However, the role of testosterone on breast tissue is not certain. Animal studies suggest that testosterone may serve as a natural, endogenous protector of the breast and limit mitogenic and cancer promoting effects of estrogen on mammary epithelium. In ovariectomized rhesus monkeys, testosterone was given in combination with 17beta estradiol (E2) for 3 days. Compared to E2 administration alone, testosterone reduced E2-induced proliferation by approximately 40% and entirely abolished E2-induced augmentation of estrogen receptor alpha expression [36].
An association between elevated endogenous testosterone levels and increased risk of breast cancer has been suggested in some case control studies [37, 38], but other studies have not found this association, particularly when testosterone levels are adjusted for estradiol levels [39, 40]. In a comprehensive review on this topic, methodological differences between these studies and the variability in assays used for measurement of free and total testosterone are identified as probably reasons for this inconsistent data [41]. Testosterone levels have also been evaluated as a risk factor for recurrence in breast cancer patients. In a nested case-control study from the randomized diet trial (Women’s Healthy Eating and Living Study), baseline serum concentrations of estradiol, testosterone, and sex hormone binding globulin were compared in women with breast cancer with and without recurrence with >7 years of follow up [42]. In 153 case-control pairs of perimenopausal and postmenopausal women in this analysis, total estradiol, bioavailable estradiol, and free estradiol concentrations were significantly associated with risk for recurrence, whereas testosterone and sex hormone binding globulin concentrations did not differ between cases and controls and were not associated with risk for recurrence.
Effect of testosterone replacement on sexual function
A large cross-sectional study found no evidence of a significant decrease in circulating androgens during the menopause transition [43]. During the natural menopausal transition, circulating androgen levels do not drop dramatically from the premenopausal state. However, oophorectomy and premature ovarian failure seem to result in a more profound decrease in circulating androgens [44, 45]. The currently available data suggests that women with near-total depletion of androgens (such as following a bilateral oophorectomy or with adrenal insufficiency) and concurrent complaints of impaired well-being and libido are the most likely to benefit from androgen replacement therapy [46]. Beneficial effects on libido and mood have been reported in studies on testosterone replacement in surgically menopausal women [47, 48]. In a study of seventy-five women who had undergone oophorectomy, patients received conjugated equine estrogens (at least 0.625 mg per day orally) and then were randomized to either placebo, 150 micrograms, or 300 micrograms of transdermal testosterone daily for 12 weeks [49]. The higher testosterone dose resulted in significant increases in scores for frequency of sexual activity and pleasure-orgasm compared to placebo. In a much larger and more recent study, 814 postmenopausal women with hypoactive sexual desire disorder who were not receiving estrogen therapy were randomized to a patch delivering 150 or 300 micrograms of testosterone per day or placebo [50]. At 24 weeks, a significant improvement in the 4-week frequency of satisfying sexual episodes was observed in the group receiving 300 micrograms of testosterone per day but not in the group receiving 150 micrograms per day. As compared with placebo, both doses of testosterone were associated with significant increases in desire and decreases in distress. The number of breast cancer cases was low overall (four women who received testosterone as compared with none who received placebo), so no conclusions can be drawn regarding increasing breast cancer risk as a result of this intervention.
Testosterone replacement in breast cancer patients
A small case series described improvements in sexual function and satisfaction in three patients with a history of breast cancer treated with a combination of testosterone supplementation and either vaginal estrogen tablets (Vagifem) or systemic estrogen replacement [51]. Each of the patients underwent a comprehensive gynecological and psychosexual evaluation and was advised of the lack of safety data on testosterone supplementation in breast cancer patients. These patients expressed understanding of the risks and opted to continue testosterone therapy. In this case series, as with most studies of testosterone replacement in patients without breast cancer, estrogen replacement was administered concurrently with androgens to help alleviate vaginal dryness. Little is known about the effect of testosterone replacement in women with breast cancer who are in an estrogen depleted state. A recent study evaluated the impact of transdermal testosterone on libido in postmenopausal female survivors of cancer [52]. One hundred and fifty women were randomized to 4 weeks of 2% testosterone in Vanicream or placebo in Vanicream, followed by a crossover to the alternate therapy for 4 additional weeks. The majority of women were taking either tamoxifen (46%) or AIs (30%). Despite significant increases in free and bioavailable testosterone levels (and no increase in estradiol levels), there was no significant improvement in sexual desire for women taking transdermal testosterone. Taken together, these data suggest that testosterone replacement is most likely to improve libido in women who are also receiving supplemental estrogen, a situation not recommended to most breast cancer survivors.
Ongoing trials
The University of California San Francisco (UCSF) is conducting a pilot trial evaluating the safety and tolerability of the ESTRING or 1% testosterone cream administered vaginally for 12 weeks as treatment for vaginal dryness and/or decreased libido in post-menopausal women receiving an AI for Stage I-III breast cancer [53]. The primary objective is to evaluate safety by determining whether an unacceptable number of patients receiving either of these treatments experience an elevation of serum estradiol level outside of the post-menopausal range at several time points. This study will also objectively evaluate changes in vaginal epithelium over the 12 week treatment period and will explore whether either of these treatments are effective in improving gynecologic or sexual quality of life in this patient population.
The North Central Cancer Treatment Group (NCCTG) is currently conducting a randomized placebo controlled phase III trial to evaluate the efficacy and toxicities associated with pilocarpine, a non-selective muscarinic receptor agonist in the parasympathetic nervous system, as treatment for vaginal dryness in post-menopausal women either with a history of breast cancer or who do not want to take vaginal estrogen for a fear of increased risk of breast cancer [54].
Table 1 summarizes the spectrum of pharmacologic interventions studied for female sexual dysfunction and identifies studies that have included breast cancer patients.
Conclusion
In summary, sexual dysfunction has a significant impact on quality of life in breast cancer survivors. Symptoms of sexual dysfunction, including vaginal dryness and decreased libido are prevalent among breast cancer survivors, particularly in patients treated with AIs, and may lead to non-compliance or discontinuation of hormonal therapy in some patients. Further research, including special attention to the safety of hormone based interventions, is necessary to manage this complication of breast cancer treatment.
References
Barni S, Mondin R. Sexual dysfunction in treated breast cancer patients. Ann Oncol. 1997;8:149–53.
Ganz PA, Rowland JH, Desmond K, Meyerowitz BE, Wyatt GE. Life after breast cancer: understanding women’s health-related quality of life and sexual functioning. J Clin Oncol. 1998;16:501–14.
Speer JJ, Hillenberg B, Sugrue DP, et al. Study of sexual functioning determinants in breast cancer survivors. Breast J. 2005;11:440–7.
Burwell SR, Case LD, Kaelin C, Avis NE. Sexual problems in younger women after breast cancer surgery. J Clin Oncol. 2006;24:2815–21.
Ganz PA, Greendale GA, Petersen L, Kahn B, Bower JE. Breast cancer in younger women: reproductive and late health effects of treatment. J Clin Oncol. 2003;21:4184–93.
Ganz PA, Desmond KA, Leedham B, Rowland JH, Meyerowitz BE, Belin TR. Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. J Natl Cancer Inst. 2002;94:39–49.
Broeckel JA, Thors CL, Jacobsen PB, Small M, Cox CE. Sexual functioning in long-term breast cancer survivors treated with adjuvant chemotherapy. Breast Cancer Res Treat. 2002;75:241–8.
Yoon J, Malin JL, Tisnado DM, et al. Symptom management after breast cancer treatment: is it influenced by patient characteristics? Breast Cancer Res Treat 2007.
Young-McCaughan S. Sexual functioning in women with breast cancer after treatment with adjuvant therapy. Cancer Nurs. 1996;19:308–19.
Montejo AL, Llorca G, Izquierdo JA, Rico-Villademoros F. Incidence of sexual dysfunction associated with antidepressant agents: a prospective multicenter study of 1022 outpatients. Spanish Working Group for the Study of Psychotropic-Related Sexual Dysfunction. J Clin Psychiatry. 2001;62 Suppl 3:10–21.
Loprinzi CL, Kugler JW, Sloan JA, et al. Venlafaxine in management of hot flashes in survivors of breast cancer: a randomised controlled trial. Lancet. 2000;356:2059–63.
Loprinzi CL, Levitt R, Barton D, et al. Phase III comparison of depomedroxyprogesterone acetate to venlafaxine for managing hot flashes: North Central Cancer Treatment Group Trial N99C7. J Clin Oncol. 2006;24:1409–14.
Desmarais JE, Looper KJ. Interactions between tamoxifen and antidepressants via cytochrome P450 2D6. J Clin Psychiatry. 2009;70:1688–97.
Mathias C, Cardeal Mendes CM, Ponde de Sena E, et al. An open-label, fixed-dose study of bupropion effect on sexual function scores in women treated for breast cancer. Ann Oncol. 2006;17:1792–6.
Morales L, Neven P, Timmerman D, et al. Acute effects of tamoxifen and third-generation aromatase inhibitors on menopausal symptoms of breast cancer patients. Anticancer Drugs. 2004;15:753–60.
Fallowfield L, Cella D, Cuzick J, Francis S, Locker G, Howell A. Quality of life of postmenopausal women in the Arimidex, Tamoxifen, Alone or in Combination (ATAC) Adjuvant Breast Cancer Trial. J Clin Oncol. 2004;22:4261–71.
Cella D, Fallowfield L, Barker P, Cuzick J, Locker G, Howell A. Quality of life of postmenopausal women in the ATAC (“Arimidex”, tamoxifen, alone or in combination) trial after completion of 5 years’ adjuvant treatment for early breast cancer. Breast Cancer Res Treat. 2006;100:273–84.
Fallowfield LJ, Bliss JM, Porter LS, et al. Quality of life in the intergroup exemestane study: a randomized trial of exemestane versus continued tamoxifen after 2 to 3 years of tamoxifen in postmenopausal women with primary breast cancer. J Clin Oncol. 2006;24:910–7.
Land SR, Wickerham DL, Costantino JP, et al. Patient-reported symptoms and quality of life during treatment with tamoxifen or raloxifene for breast cancer prevention: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. Jama. 2006;295:2742–51.
Rioux JE, Devlin C, Gelfand MM, Steinberg WM, Hepburn DS. 17beta-estradiol vaginal tablet versus conjugated equine estrogen vaginal cream to relieve menopausal atrophic vaginitis. Menopause (New York, NY). 2000;7:156–61.
Simunic V, Banovic I, Ciglar S, Jeren L, Pavicic Baldani D, Sprem M. Local estrogen treatment in patients with urogenital symptoms. Int J Gynaecol Obstet. 2003;82:187–97.
Barentsen R, van de Weijer PH, Schram JH. Continuous low dose estradiol released from a vaginal ring versus estriol vaginal cream for urogenital atrophy. Eur J Obstet Gynecol Reprod Biol. 1997;71:73–80.
Sarkar NN. Low-dose intravaginal estradiol delivery using a Silastic vaginal ring for estrogen replacement therapy in postmenopausal women: a review. Eur J Contracept Reprod Health Care. 2003;8:217–24.
Weisberg E, Ayton R, Darling G, et al. Endometrial and vaginal effects of low-dose estradiol delivered by vaginal ring or vaginal tablet. Climacteric. 2005;8:83–92.
Kendall A, Dowsett M, Folkerd E, Smith I. Caution: vaginal estradiol appears to be contraindicated in postmenopausal women on adjuvant aromatase inhibitors. Ann Oncol. 2006;17:584–7.
Kloosterboer HJ. Tissue-selective effects of tibolone on the breast. Maturitas. 2004;49:S5–S15.
Gompel A, Siromachkova M, Lombet A, Kloosterboer HJ, Rostene W. Tibolone actions on normal and breast cancer cells. Eur J Cancer. 2000;36 Suppl 4:S76–7.
Morris EP, Wilson PO, Robinson J, Rymer JM. Long term effects of tibolone on the genital tract in postmenopausal women. Br J Obstet Gynaecol. 1999;106:954–9.
Cummings SR, Ettinger B, Delmas PD, et al. The effects of tibolone in older postmenopausal women. N Engl J Med. 2008;359:697–708.
Tibolone study in breast cancer patients to close ahead of schedule. 2007 [cited 2007 October 6]; Press Release]. Available from:
Kenemans P, Bundred NJ, Foidart JM, et al. Safety and efficacy of tibolone in breast-cancer patients with vasomotor symptoms: a double-blind, randomised, non-inferiority trial. Lancet Oncol. 2009;10:135–46.
Loprinzi CL, Abu-Ghazaleh S, Sloan JA, et al. Phase III randomized double-blind study to evaluate the efficacy of a polycarbophil-based vaginal moisturizer in women with breast cancer. J Clin Oncol. 1997;15:969–73.
Bygdeman M, Swahn ML. Replens versus dienoestrol cream in the symptomatic treatment of vaginal atrophy in postmenopausal women. Maturitas. 1996;23:259–63.
Nachtigall LE. Comparative study: replens versus local estrogen in menopausal women. Fertil Steril. 1994;61:178–80.
Rowland JH, Meyerowitz BE, Crespi CM, et al. Addressing intimacy and partner communication after breast cancer: a randomized controlled group intervention. Breast Cancer Res Treat. 2009;118:99–111.
Zhou J, Ng S, Adesanya-Famuiya O, Anderson K, Bondy CA. Testosterone inhibits estrogen-induced mammary epithelial proliferation and suppresses estrogen receptor expression. FASEB J. 2000;14:1725–30.
Berrino F, Muti P, Micheli A, et al. Serum sex hormone levels after menopause and subsequent breast cancer. J Natl Cancer Inst. 1996;88:291–6.
Yu H, Shu XO, Shi R, et al. Plasma sex steroid hormones and breast cancer risk in Chinese women. Int J Cancer. 2003;105:92–7.
Hankinson SE, Willett WC, Manson JE, et al. Plasma sex steroid hormone levels and risk of breast cancer in postmenopausal women. J Natl Cancer Inst. 1998;90:1292–9.
Zeleniuch-Jacquotte A, Bruning PF, Bonfrer JM, et al. Relation of serum levels of testosterone and dehydroepiandrosterone sulfate to risk of breast cancer in postmenopausal women. Am J Epidemiol. 1997;145:1030–8.
Somboonporn W, Davis SR. Postmenopausal testosterone therapy and breast cancer risk. Maturitas. 2004;49:267–75.
Rock CL, Flatt SW, Laughlin GA, et al. Reproductive steroid hormones and recurrence-free survival in women with a history of breast cancer. Cancer Epidemiol Biomark Prev. 2008;17:614–20.
Davison SL, Bell R, Donath S, Montalto JG, Davis SR. Androgen levels in adult females: changes with age, menopause, and oophorectomy. J Clin Endocrinol Metab. 2005;90:3847–53.
Laughlin GA, Barrett-Connor E, Kritz-Silverstein D, von Muhlen D. Hysterectomy, oophorectomy, and endogenous sex hormone levels in older women: the Rancho Bernardo Study. J Clin Endocrinol Metab. 2000;85:645–51.
Burger HG. Androgen production in women. Fertil Steril. 2002;77 Suppl 4:S3–5.
Arlt W. Androgen therapy in women. Eur J Endocrinol. 2006;154:1–11.
Braunstein GD, Sundwall DA, Katz M, et al. Safety and efficacy of a testosterone patch for the treatment of hypoactive sexual desire disorder in surgically menopausal women: a randomized, placebo-controlled trial. Arch Intern Med. 2005;165:1582–9.
Buster JE, Kingsberg SA, Aguirre O, et al. Testosterone patch for low sexual desire in surgically menopausal women: a randomized trial. Obstet Gynecol. 2005;105:944–52.
Shifren JL, Braunstein GD, Simon JA, et al. Transdermal testosterone treatment in women with impaired sexual function after oophorectomy. N Engl J Med. 2000;343:682–8.
Davis SR, Moreau M, Kroll R, et al. Testosterone for low libido in postmenopausal women not taking estrogen. N Engl J Med. 2008;359:2005–17.
Krychman ML, Stelling CJ, Carter J, Hudis CA. A case series of androgen use in breast cancer survivors with sexual dysfunction. J Sex Med 2007.
Barton DL, Wender DB, Sloan JA, et al. Randomized controlled trial to evaluate transdermal testosterone in female cancer survivors with decreased libido; North Central Cancer Treatment Group protocol N02C3. J Natl Cancer Inst. 2007;99:672–9.
http://clinicaltrials.gov/ct2/show/study/NCT00698035?view=results. Vaginal testosterone cream vs ESTRING for vaginal dryness or decreased libido in early stage breast cancer patients (E-String). 2009 February 23, 2009 [cited; Available from:
http://clinicaltrials.gov/ct2/show/NCT00343382?term=pilocarpine&rank=4. Pilocarpine in treating vaginal dryness in patients with breast cancer. 2009 May 21, 2009 [cited; Available from:
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Melisko, M.E., Goldman, M. & Rugo, H.S. Amelioration of sexual adverse effects in the early breast cancer patient. J Cancer Surviv 4, 247–255 (2010). https://doi.org/10.1007/s11764-010-0130-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-010-0130-1