Abstract
Bacillary dysentery is a type of dysentery and a severe form of shigellosis. This dysentery is usually restricted to Shigella infection, but Salmonella enterica and enteroinvasive Escherichia coli strains are also known as this infection’s causative agents. The emergence of drug-resistant, bacillary dysentery-causing pathogens is a global burden, especially for developing countries with poor hygienic environments. This study aimed to isolate, identify, and determine the drug-resistant pattern of bacillary dysentery-causing pathogens from the stool samples of the Kushtia region in Bangladesh. Hence, biochemical tests, serotyping, molecular identification, and antibiotic profiling were performed to characterize the pathogens. Among one hundred fifty (150) stool samples, 18 enteric bacterial pathogens were isolated and identified, where 12 were Shigella strains, 5 were S. enterica sub spp. enterica strains and one was the E.coli strain. Among 12 Shigella isolates, 8 were Shigella flexneri 2a serotypes, and 4 were Shigella sonnei Phage-II serotypes. Except for three Salmonella strains, all isolated strains were drug-resistant (83%), whereas 50% were multidrug-resistant (MDR), an alarming issue for public health. In antibiotic-wise analysis, the isolated pathogens showed the highest resistance against nalidixic acid (77.78%), followed by tetracycline (38.89%), kanamycin (38.89%), amoxicillin (27.78%), streptomycin (27.78%), cefepime (22.22%), ceftriaxone (22.22%), ampicillin (16.67%), ciprofloxacin (16.67%), and chloramphenicol (16.67%). The existence of MDR organisms that cause bacillary dysentery in the Kushtia area would warn the public to be more health conscious, and physicians would administer medications cautiously. The gradual growth of MDR pathogenic microorganisms needs immediate attention, and the discovery of effective medications must take precedence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacillary dysentery, like shigellosis, is a leading cause of morbidity and mortality worldwide, particularly in children over five in low- and middle-income nations, including Bangladesh (Arnold 2021; Houpt et al. 2021; Ud-Din and Wahid 2014). Annually, bacillary dysentery causes 165 million reported or confirmed cases and 1.1 million fatalities worldwide, primarily in underdeveloped nations (Ali Nor et al. 2021; Anas et al. 2021; Duchen et al. 2021). This type of dysentery is associated with the species of bacteria from the Enterobacteriaceae family. A current estimate shows that shigellosis caused 164,300 and 270,000 deaths in 2015 and 2016, respectively (Barragán et al. 2021; Chua et al. 2021; Khalil et al. 2021; Khalil et al. 2018).
Shigellosis was responsible for nearly 122,000 deaths in 2010 (8.93% of all diarrheal deaths). In addition, more than 270,000 people died in 2016, accounting for 16.88% of all diarrheal deaths (Barragán et al. 2021; Chua et al. 2021; Khalil et al. 2021). In terms of non-typhoidal Salmonella infection, there were 93 million cases and 155,000 fatalities in 2010, with 3.4 million cases and 681,316 deaths observed in 2015 (Eng et al. 2015). Additionally, 95.1 million non-typhoidal Salmonella infections and 50,771 fatalities were recorded in 2017 (Gambino et al. 2021; Gargano et al. 2021; Wójcicki et al. 2021).
In 2016, across all age categories, enterotoxigenic Escherichia coli (ETEC) was the sixth leading cause of diarrhea mortality, accounting for 51,186 fatalities and roughly 3.2% (1.8–4.7) of all diarrhea deaths. ETEC was responsible for 4.2% (2.2–6.8) of diarrhea-related mortality in children under five years old ( Khalil et al. 2021, 2018). This sickness is closely linked to ingesting contaminated food and water. Infections with Shigella species cause around 600,000 fatalities in children under ten. Although S. dysenteries are associated with the most severe illness and have a high fatality rate during outbreaks, S. flexneri is the most common cause of the chronic form of the disease, which accounts for the majority of fatalities (Bazhenova et al. 2021; Excler et al. 2021; Khalil et al. 2021).
Understanding the worldwide public health dilemma of MDR dysentery-causing bacterial strains requires isolating the causal organisms. In addition to isolating bacterial agents, identifying such species using modern molecular biology methods is the most prevalent method. Finally, antibiotic profiling of these strains may offer a comprehensive insight into the antibiotic resistance situation of the identified causative agents. This study aimed to identify and profile antibiotic susceptibilities of different bacillary dysentery-causing pathogenic bacteria isolated from stool samples in the Kushtia region and characterize the isolated bacteria using biochemical, molecular, and genus/species-level identification techniques, if possible.
Methodology
Collection and maintenance of samples
During 2016–2018, 150 stool samples were obtained from dysentery patients at the Tofazzael Health Centre and a few other clinics in the town of Kushtia. Urgently, the stool samples were analyzed in the laboratory. In the case of samples from the distant location, the samples were first stored in a sterile screw-cap plastic tube, then placed in an icebox or refrigerator, and analyzed within 24 h. The collection of stool samples was based on the naked eye assessment. The physical characteristics of the feces, particularly its color and appearance, the patient’s medical history, and the patient’s important symptoms were taken into account while selecting screening samples for this investigation. Seventy (70) patients out of one hundred fifty (150) were under the age of five, twenty (20) patients were between the ages of five and eighteen (18), and the remaining sixty (60) patients were 18 years or older. Eighty-seven (87) of these one hundred fifty (150) patients were male, whereas sixty-three (63) were female.
Biochemical test
Biochemical tests were performed according to standard protocol (Bopp et al. 2003; Chen et al. 2021; WHO 1987, 1995). Briefly, the collected samples were diluted serially from 10− 2 to 10− 8 with autoclaved distilled water, and 100 µl of each dilution was evenly plated onto Salmonella-Shigella (SS) agar. Besides SS agar, two other selective media McConkey (MAC) and xylose lysine deoxycholate (XLD) agar, and one) screening media, triple sugar iron (TSI), were used. In addition, an oxidase test (with 1% NNNN- tetramethyl-p-phenylenediamine dihydrochloride) and a catalase test (with 3% hydrogen peroxide solution) were performed. For long-term storage, a 50% (v/v) glycerol stock of bacterial strains spp. was prepared and stored at − 80 °C.
Serological identification of Shigella spp.
A commercially available antisera kit (Denka Seiken Co., Ltd., Tokyo, Japan) specific for all types and group-factor antigens was used for the serotyping of Shigella isolates. The slide agglutination test observed serological reactions according to the manufacturer’s instructions. According to the manufacturer’s instructions, the polyvalent sera S. dysenteriae will show agglutination with Poly-A or Poly-A1, S. flexneri will show agglutination with Poly-B, S. boydii will show agglutination with Poly-C1, Poly-C2, or Poly C3, and S. sonnei will show agglutination with Poly-D. For the serotyping of S. flexneri, type-specific monovalent sera I, II, III, IV, V, and VI and group-specific monovalent sera 3(4), 6, 7(8) were used, while for S. sonnei type-specific monovalent sera Phage-I and Phage-II were used.
DNA extraction and 16 S rDNA sequencing analysis
The boiling method was used for bacterial DNA extraction, according to Sun et al. (2011). In brief, an overnight culture single colony (at 37 °C) from Luria-Bertani (LB) agar Petri dish was suspended in 30 µl of autoclaved distilled water. It was then boiled at 100 °C for 10 min. The culture was directly transferred into the ice and kept inside the ice for 5 min. It was then centrifuged at 13,000 rpm for 10 min, and the supernatant, containing DNA molecule, was used as the template for Polymerase Chain Reaction (PCR) amplification. The concentration of extracted DNA was measured through Nanodrop. The band of DNA was observed through Gel electrophoresis in 1% agarose gel. Two bacteria-specific primers, forward 27 F (AGAGTTTGATCCTGGCTCAG) and reverse R1391 (GACGGGCGGTGTGTRCA) (Lane 1991; Walker and Pace 2007), were used to amplify 16 S rDNA fragments. PCR recipe according to (Mahbubur Rahman et al. 2014), the reaction mixture for each PCR consisted of 2X PCR buffer 10 µl (containing dNTPs and MgCl2), Taq DNA polymerase 0.4 µl, 1.5 µl of each primer, 1 µl of template DNA in a final reaction volume of 20 µl. Thermal cycle, denaturing step 95 °C for 3 min, followed by 35 cycles of 95 °C for 30 s, annealing step 48 °C for 30 s, and extending step 72 °C for 90 s, with a final extension of 72 °C for 5 min in a thermocycler (G-Strom, UK).
The PCR products were sent to Apical Scientific, Malaysia, for 16 S rDNA sequencing. A partial sequence of 16 S ribosomal DNA was carried out by using Applied Biosystem 3130. (https://vlab.amrita.edu/?sub=3&brch=76&sim=1421&cnt=1). The sequence was analyzed through the NCBI (National Center for Biotechnology Information) BLAST (Basic Local Alignment Search Tool) (http://www.ncbi.nlm.nih.gov) program. The phylogenetic analysis was done through Megablast using the NCBI database from the microbial nucleotide sequences section (Rahman et al. 2017). The aligned sequences were then subjected to a phylogenetic tree construction by selecting the first twenty (20) sequences and clicking to distance tree results. The neighbor-joining evolution method inferred the evolutionary history (Dash et al. 2015). The maximum sequence differences were 0.75, and the sequences were labeled with taxonomic names (Sequence ID) (Wajda et al. 2018).
Antibiotic profiling of isolated bacterial strains
Following CLSI (Clinical and Laboratory Standards Institute) guidelines, the disc diffusion technique performed antibiotic profiling of the isolated bacterial strains (Patel 2016). In this experiment, ten (10) antibiotics, including ampicillin (5 g), amoxicillin (10 g), tetracycline(30 g), streptomycin (25 g), kanamycin(30 g), ciprofloxacin(5 g), cefepime (20 g), nalidixic acid (30 g), ceftriaxone(30 g), and chloramphenicol were used. Briefly, 100 µl of a broth culture of bacterial strains was swabbed evenly onto LB agar Petri plates, and antibiotic discs were carefully placed at a precise spacing and incubated at 37 °C overnight.
Results
Biochemical test
Table 1 displays the findings of biochemical testing in detail. After the initial culture on SS agar, eighteen (18) isolates were suspected of producing bacillary dysentery. On MAC agar, these eighteen (18) isolates emerged as convex, colorless colonies measuring between 1.5 and 3 millimeters in diameter. On XLD agar, colonies of twelve (12) isolates were clear pink or smooth red colonies (1 to 2 mm in diameter), while colonies of six (6) isolates were pink or red with a black core. In TSI) agar screening medium, all eighteen (18) isolates developed a red slant and yellow butt, but only six (6) of them produced black spores in the middle. All isolate strains were positive for the catalase test (produced bubbles) and negative for the oxidase test (no color change). Twelve (12) of the eighteen (18) isolates were suspected as Shigella, whereas six (6) were suspected of either Salmonella or E. coli.
Serotyping
In serotyping with polyvalent sera, S. dysenteriae showed agglutination with Poly-A or Poly-A1, S. flexneri showed agglutination with Poly-B, S. boydii showed agglutination with Poly-C1, Poly-C2 or Poly C3 and S. sonnei showed agglutination with Poly-D. Eight (8) isolates were detected as S. flexneri and four (4) as S. sonnei (Table 2). All Shigella flexneri isolates were confirmed as S. flexneri 2a, and all S. sonnei isolates were confirmed as S. sonnei phage-II (Tables 3 and 4).
Polymerase chain reaction and 16 S rDNA sequencing
Gel electrophoresis of PCR product confirmed the purity of bacterial strains (Fig. 1), and the obtained sequences of six (6) bacterial strains are given in Supplementary file-1.
Similarity test and phylogenetic analysis
Similarity test and phylogenetic analysis indicated that one isolate (S-4) showed 99.65% similarity with E. coli O157:H7 and appeared in a separate cluster in the phylogenetic tree, which implied that it could be a novel strain of E. coli. Besides, all five isolates showed similarity with S. enterica sub spp. enterica where isolates S-14 and S-17 showed 100% similarity and isolates S-8, S-10 and S-11 showed 99% similarity (Table 5; Figs. 2, 3 and 4).
Antibiotic profiling of identified bacterial strains
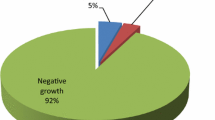
Antibiotic profiling test revealed that three (3) isolates were susceptible to all antibiotics (ten (10) antibiotics), where six (6) were drug-resistant, and nine (9) were multidrug-resistant, as shown in Table 6. Isolate S-10, identified as S. enterica, and S-12, identified as S. flexneri 2a, showed the highest resistance against seven (7) antibiotics out of ten (10). Isolate S-4 (E. coli), S-6 (S. flexneri 2a), S-8 (S. enterica), and S-9 (S. flexneri 2a) showed resistance against six (6) antibiotics out of 10. Isolates S-13(S. flexneri 2a) showed resistance against four (4) antibiotics, S-15 (S. sonnei) and S-16 (S. flexneri 2a) showed resistance against three (3) antibiotics, S-1(S. sonnei) showed resistance against two (2) antibiotics, S-2 (S. flexneri 2a), S-3 (S. flexneri 2a), S-5 (S. flexneri 2a), S-7(S. sonnei) and S-18 (S. sonnei) showed resistance against only one antibiotic out of ten (10) respectively. The drug resistance profile of eighteen (18) isolates illustrated in Fig. 5a. Three (3) isolates were responsive to all antibiotics (ten (10) antibiotics), whereas six (6) isolates were drug-resistant and nine (9) isolates were multidrug-resistant, as indicated in Table 6. Isolates S-10, identified as S. enterica, and S-12, identified as S. flexneri 2a, exhibited the greatest resistance to seven (7) out of ten antibiotics (10).S-4 (E. coli), S-6 (S. flexneri 2a), S-8 (S. enterica), and S-9 (S. flexneri 2a) were resistant to six (6) out of ten (10) antibiotics. Isolates S-13 (S. flexneri 2a) exhibited resistance to four (4) antibiotics, S-15 (S. sonnei) and S-16 (S. flexneri 2a) exhibited resistance to three (3) antibiotics, S-1 (S. sonnei) exhibited resistance to two (2) antibiotics, and isolates S-2 (S. flexneri 2a), S-3 (S. flexneri 2a), S-5 (S. flexneri 2a), S-7(S. sonnei) and S-18 (S. sonnei) showed resistance against only one antibiotic out of ten (10) respectively (Fig. 3A depicts the antibiotic resistance profiles of eighteen (18) isolates). In antibiotic-wise analysis, nalidixic acid showed the highest resistance against fourteen (14) strains out of eighteen (18), followed by tetracycline and kanamycin against seven (7) strains, amoxicillin, and streptomycin against five (5) strains, cefepime and ceftriaxone against four (4) strains, ampicillin, ciprofloxacin and chloramphenicol against three (3) strains. The percentages of resistant patterns are shown in Fig. 5b.
Drug-resistant profile and antibiotic resistance patterns analysis (%) of the isolated bacteria. a Drug-resistant profile, above the red borderline, all are MDR; b Antibiotic-wise resistance patterns. Here, AML-ampicillin, AMP- amoxicillin, T-tetracycline, S-streptomycin, K-kanamycin, CIP-ciprofloxacin, FEP-cefepime, NA-nalidixic acid, CRO-ceftriaxone, C-chloramphenicol
Discussion
The worldwide occurrence of bacillary dysentery, especially in developing countries, is a widespread phenomenon. The death toll due to this disease is also alarming. Drug-resistant, as well as MDR dysentery-causing pathogens, have been reported all over the world for a few decades. This scenario is alarming as the development of a drug is not an easy task as it is time consuming, laborious, and costly (Sheam et al. 2020). Hence, the isolation and characterization of MDR bacillary dysentery-causing bacteria in the local area is very contemporary to support and contribute comprehensive research at the global level. However, 16 S rDNA sequencing is an established method to identify different types of bacteria, most of the Shigella spp. share > 80% nucleotide sequence similarities based on the study of DNA homology, and a similar result can be found on the sequence similarities between E. coli and Shigella spp. Cilia et al. (1996) confirmed this proximal relatedness where the 16 S rDNA sequence analysis failed to separate E. coli and Shigella into two separate clades, which indicates a higher degree of similarity. Van den Bled and Reubsaet (2012) suggested that Shigella spp. should be positioned within the E. coli species due to similarities between these two groups. For this reason, serotyping is the best way to detect Shigella spp. accurately.
In this study, after examining one hundred fifty (150) stool samples, eighteen (18) bacterial strains were suspected of dysentery-causing pathogens. Among the eighteen (18) isolates, twelve (12) were suspected as Shigella, and six (6) were suspected as either Salmonella or E. coli. Among the isolates, twelve (12) were Shigella strains, five (5) were Salmonella strains, and one was E.coli strain. Among twelve (12) Shigella isolates, eight (8) were S. flexneri 2a serotype, and four (4) were S. sonnei. All five (5) Salmonella strains were S. enterica sub spp. enterica.
Ud-Din and Wahid (2014) analyzed 10,827 Shigella isolates from patients between 2001 and 2011 to determine the prevalence and distribution of different Shigella spp. in Bangladesh, where S. flexneri was the predominant species. The prevalence of S. flexneri decreased from 65.7 to 47%, whereas S. sonnei increased from 7.2 to 25% (between 2001 and 2011) (Ud-Din and Wahid 2014). S. flexneri is generally the most common species in the region; however, S. sonnei has increased over the past few decades, recently accounting for 25% or more of isolates in Bangladesh (Houpt et al. 2021; Ud-Din & Wahid, 2014; Ud-Din et al. 2013). Among 2014 diarrheal stool samples from pediatric patients of Khyber Pakhtunkhwa, Pakistan, from January 2016 to May 2017, 7.9% of Shigella species were detected among the samples. In the isolated strains, the predominant Shigella spp. was S. flexneri (96.8%), followed by S. boydii (n = 5, 3.1%) (Nisa et al. 2020).
In another study by Pervin et al. (2019) in Bangladesh, out of two hundred seventeen (217) diarrhoeal stools, ninety-seven (97) bacterial isolates were isolated. Among ninety-seven (97) culture-positive cases, the percentages of E. coli, Shigella spp., and Salmonella spp. were 51-52.58, 15-15.46, and 8-8.25%, respectively. Salmonella enteritidis was the utmost common serotype in Europe, Latin America, and Asia, accounting for 87%, 31%, and 38% of the clinical isolates, respectively (Pervin et al. 2019). In another study, 126 Salmonella isolates dispersed among seven serotypes were shown to be multidrug-resistant, with high rates of AMR to lincomycin (100%), rifampicin (100%), sulfadiazine (93.7%), erythromycin (89.7%), ciprofloxacin (81.0%), and gentamicin (75.4%). (Guan et al. 2022)
In a recent study in Somalia, Shigellosis prevalence was 20.6%, where S. flexneri (70.3%) was the prominent species (Ali Nor et al. 2021). Our findings demonstrated that the isolated strains responsible for bacillary dysentery are dominated by S. flexneri and S. sonnei, and S. enterica sub spp. In a study, five Salmonella isolates were identified in diarrheagenic infants, where two (2) were Salmonella typhimurium, two (2) were S. enteritidis, and one (1) was unidentified (Yusuf et al. 2018). Furthermore, among fifty (50) samples, Salmonella spp. was found in 16% of samples (Yusuf et al. 2018), whereas in the present study, Salmonella spp. was detected in ~ 44% of isolated strains. In the case of E. coli, only one (1) species had been identified in this study, which comprised 5.5% of the total isolated strains (n = 18).
Antibiotic profiling of all eighteen (18) isolates demonstrated that 50% of the isolated strains are MDR, and 33% of isolated strains are drug-resistant. Antibiotic profiling reveals that three isolates, S-11, S-14, and S-17, were susceptible to all antibiotics. Isolate S-2 (S. flexneri 2a), S-3 (S. flexneri 2a), S-5 (S. flexneri 2a), S-7 (S. sonnei) and S-18 (S. sonnei) were drug resistant while isolate S-10 (S. flexneri 2a), S-4 (E. coli ), S-6 (S. flexneri 2a), S-8 (S. enterica) S-9 (S. flexneri 2a), S-13 (S. flexneri 2a), S-15 (S. sonnei), S-16 (S. flexneri 2a) and S-1 (S. sonnei) were multidrug resistant. The pooled prevalence rates of MDR and extended-spectrum beta-lactamase (ESBL)-producing Shigella bacteria were 68.7% and 23.9%, respectively, according to a comprehensive and systematic study done by Salleh et al. (2022). Ali Ali Nor et al. (2021) reported that all the serogroups were 100% resistant to ampicillin, trimethoprim-sulfamethoxazole, and tetracycline, where ceftriaxone resistance was the highest among S. sonnei (66.7%). In Somalia, MDR Shigella strains, including those resistant to ciprofloxacin and ceftriaxone, have emerged, posing a public health threat (Ali Nor et al. 2021). Dhaka city in Bangladesh has high rates of azithromycin-resistant Shigella, particularly among S. sonnei, and the treatment outcomes are poor in these individuals. (Houpt et al. 2021).
According to the Centers for Disease Control and Prevention (CDC), approximately 77,000 antibiotic-resistant Shigella infections occur annually in the United States (Mercante & Winchell, 2015). Recently, high frequency of trimethoprim/sulfamethoxazole (80%), ampicillin (85%), cefotaxime (63%), and nalidixic acid (47%) resistant Shigella spp. has been reported in Iran (Mahmoudi et al. 2017). Furthermore, three subsequent annual reports published by the National Salmonella, Shigella & Listeria Reference Laboratory, Ireland (NSSLRL) in 2014, 2015, and 2016 revealed that the percentages of MDR Shigella were 93%, 91%, and 82.5%, respectively. This organization reported fourteen (14) ciprofloxacin-resistant and eight (8) azithromycin-resistant Shigella strains in 2015, while seventeen (17) ciprofloxacin-resistant and six (6) azithromycin-resistant strains were reported in 2016 (Mahbubur Rahman et al. 2007). Puzari et al. (2018) recently noticed that Shigella had developed resistance against fluoroquinolones, cephalosporins, and azithromycin, but earlier, they were susceptible to ampicillin, chloramphenicol, cotrimoxazole, and nalidixic acid (Puzari et al. 2018). According to National Salmonella, Shigella & Listeria Reference Laboratory, Ireland (NSSLRL) (2017), 31.4% of Salmonella isolates (n = 122) were MDR (three or more different classes of antibiotics). Among the MDR isolates, 30.3% (n = 37) had the profile of resistance to ampicillin, sulphonamides, and tetracycline and were mainly monophasic S. typhimurium.
In the current study, kanamycin and tetracycline exhibited 38.89% antibiotic resistance (Fig. 3B). In Spain, one hundred fifty-four (154) tetracycline-resistant isolates of traveler’s diarrhea were recovered as confirmed causes, where 79.2% were more frequent isolates of S. sonnei strains and S. flexneri (Ranjbar and Farahani 2019). In another study, Al-Hajj et al. (2020) reported that, among eight isolated Shigella spp., three species were resistant to kanamycin and nitrofurantoin. In the current study, ampicillin and chloramphenicol showed 16.67% resistance (Al-Hajj et al. 2020). Antimicrobial susceptibility and resistance mechanisms were evaluated in one hundred nine (109) Shigella and forty (40) Salmonella isolates in southern Mozambique. It was found that 52% and 56% of Shigella isolates were resistant to chloramphenicol and ampicillin, respectively. Also, S. flexneri isolates were more resistant than S. sonnei to chloramphenicol and ampicillin. Besides, only 3% of Salmonella isolates were resistant to nalidixic acid (Mandomando et al. 2009). However, in the present study, 77.78% of isolated strains were resistant to nalidixic acid. The MDR pathogen poses an immediate danger to public health, necessitating prudent and justifiable responses. Effective antibiotic treatment techniques that may result in improved results for the control and treatment of shigellosis in Asia are necessary (Salleh et al. 2022).
Conclusion
The estimated annual mortality toll attributable to diarrheal illnesses is around two million. Diarrheal diseases rank third among infectious disease causes of death. Recent observations indicate that the bacteria causing bacillary dysentery are growing resistant to an increasing number of drugs. This is really frightening, and if the majority of antibiotics lose their sensitivity, we will be unable to stop it. It may progress from endemic to an epidemic and even pandemic status. Emerging antibiotic resistance among bacillary dysentery-causing bacteria is a global public health problem, particularly in underdeveloped nations. Bangladesh is not immune to the worldwide danger posed by bacillary dysentery. The paucity of alternative or new antibiotics in development and research has been regarded uneconomical owing to the short duration of antibiotics compared to medications used to treat chronic conditions. Therefore, it is of the utmost need to find a durable, effective, and drug-resistant alternative therapy for infectious diseases that safeguards drug-resistant organisms.
Abbreviations
- ETEC:
-
Enterotoxigenic Escherichia coli
- LB:
-
Luria-Bertani
- NCBI:
-
NCBI National Center for Biotechnology Information
- BLAST:
-
BLAST Basic Local Alignment Search Tool
- PCR:
-
Polymerase Chain Reaction
- MAC:
-
MacConkey
- MDR:
-
Multidrug-resistant
References
Al-Hajj EM, Mohamed MS, Abd Alfadil NA, Altayb HN, Idris AB et al (2020) Contamination of currency notes with Kanamycin Resistant Shigella flexneri. BioRxiv. https://doi.org/10.1101/2020.03.07.982017
Ali Nor BS, Menza NC, Musyoki AM (2021) Multidrug-resistant shigellosis among children aged below five years with diarrhea at Banadir Hospital in Mogadishu, Somalia. Can J Infect Dis Med Microbiol 2021. https://doi.org/10.1155/2021/6630272
Anas M, Sami MA, Siddiqui Z, Khatoon K, Zeyad MT et al (2021) Impact of climate change on the incidence and transfer of food-and water-borne diseases. Microbiomes and the global climate change, Springer, Berlin, pp 123–144. https://doi.org/10.1007/978-981-33-4508-9_9
Arnold SL (2021) Target product profile and development path for Shigellosis treatment with antibacterials. ACS Infect Dis 7:948–958. https://doi.org/10.1021/acsinfecdis.0c00889
Barragán JM, Cuesta LD, Susa MR (2021) Quantitative microbial risk assessment to estimate the public health risk from exposure to enterotoxigenic E. coli in drinking water in the rural area of Villapinzon. Colombia Microb Risk Anal 100173. https://doi.org/10.1016/j.mran.2021.100173
Bazhenova A, Gao F, Bolgiano B, Harding SE (2021) Glycoconjugate vaccines against Salmonella enterica serovars and Shigella species: existing and emerging methods for their analysis. Biophys Revs 1–26. https://doi.org/10.1007/s12551-021-00791-z
Bopp CA, Brenner FW, Fields PI, et al. Escherichia, Shigella, and Salmonella (2003) In: Murray PR, Baron EJ, Jorgensen JH, et al, Manual of clinical microbiology, 8th edition, Washington, DC: ASM Press 1:654–71
Chen S-H, Parker CH, Croley TR, McFarland MA (2021) Genus, species, and subspecies classification of Salmonella isolates by proteomics. Appl Sci 11:4264. https://doi.org/10.3390/app11094264
Chua PL, Huber V, Ng CFS, Seposo XT, Madaniyazi L et al (2021) Global projections of temperature-attributable mortality due to enteric infections: a modelling study. Lancet Planet Health 5:e436–e445. https://doi.org/10.1016/S2542-5196(21)00152-2
Cilia V, Lafay B, Christen R (1996) Sequence heterogeneities among 16S ribosomal RNA sequences, and their effect on phylogenetic analyses at the species level. Mol Biol Evol 13:451–461. https://doi.org/10.1093/oxfordjournals.molbev.a025606
Dash BK, Rahman MM, Sarker PK (2015) Molecular identification of a newly isolated Bacillus subtilis BI19 and optimization of production conditions for enhanced production of extracellular amylase. BioMed Res Int 2015. https://doi.org/10.1155/2015/859805
Duchen D, Haque R, Chen L, Wojcik G, Korpe P et al (2021) Host genome-wide association study of infant susceptibility to Shigella-associated diarrhea. Infect Immun 89:e00012-00021. https://doi.org/10.1128/IAI.00012-21
Eng S-K, Pusparajah P, Ab Mutalib N-S, Ser H-L, Chan K-G et al (2015) Salmonella: a review on pathogenesis, epidemiology and antibiotic resistance. Front Life Sci 8:284–293. https://doi.org/10.1080/21553769.2015.1051243
Excler J-L, Privor-Dumm L, Kim JH (2021) Supply and delivery of vaccines for global health. Curr Opin Immunol 71:13–20. https://doi.org/10.1016/j.coi.2021.03.009
Gambino D, Sciortino S, Migliore S, Galuppo L, Puleio R et al (2021) Preliminary results on the prevalence of Salmonella spp. in marine animals stranded in sicilian coasts: antibiotic susceptibility profile and ARGs detection in the isolated strains. Pathogens 10:930. https://doi.org/10.3390/pathogens10080930
Gargano V, Sciortino S, Gambino D, Costa A, Agozzino V et al (2021) Antibiotic susceptibility profile and tetracycline resistance genes detection in Salmonella spp strains isolated from animals and food. Antibiotics 10:809. https://doi.org/10.3390/antibiotics10070809
Guan Y, Li Y, Li J, Yang Z, Zhu D, Jia R, Liu M, Wang M, Chen S, Yang Q, Wu Y, Zhang S, Gao Q, Ou X, Mao S, Huang J, Sun D, Tian B, Cheng A, Zhao X (2022) Phenotypic and genotypic characterization of antimicrobial resistance profiles in Salmonella isolated from waterfowl in 2002–2005 and 2018–2020 in Sichuan, China. Front Microbiol 13:987613. https://doi.org/10.3389/fmicb.2022.987613
Houpt ER, Ferdous T, Ara R, Ibrahim M, Alam MM et al (2021) Clinical outcomes of drug-resistant shigellosis treated with azithromycin in Bangladesh. Clin Infect Dis 72:1793–1798. https://doi.org/10.1093/cid/ciaa363
Khalil I, Walker R, Porter CK, Muhib F, Chilengi R et al (2021) Enterotoxigenic Escherichia coli (ETEC) vaccines: Priority activities to enable product development, licensure, and global access. Vaccine 39(31):4266–4277. https://doi.org/10.1016/j.vaccine.2021.04.018
Khalil IA, Troeger C, Blacker BF, Rao PC, Brown A et al (2018) Morbidity and mortality due to Shigella and enterotoxigenic Escherichia coli diarrhoea: the global burden of disease study 1990–2016. Lancet Infect Dis 18:1229–1240. https://doi.org/10.1016/S1473-3099(18)30475-4
Lane DJ (1991) 16S/23S rRNA sequencing. Nucleic Acid Techniques in Bacterial Systematics. Edited by: Stackebrandt E, Goodfellow M., Wiley, Chichester, UK, pp 115–175
Mahbubur Rahman M, Shoma S, Rashid H, Arifeen SE, Baqui A et al (2007) Increasing spectrum in antimicrobial resistance of Shigella isolates in Bangladesh: resistance to azithromycin and ceftriaxone and decreased susceptibility to ciprofloxacin. J Health Popul Nutr 25(2):158
Mahmoudi S, Pourakbari B, Moradzadeh M, Eshaghi H, Ramezani A et al (2017) Prevalence and antimicrobial susceptibility of Salmonella and Shigella spp. among children with gastroenteritis in an iranian referral hospital. Microb Pathog 109:45–48. https://doi.org/10.1016/j.micpath.2017.05.023
Mandomando I, Jaintilal D, Pons MJ, Vallès X, Espasa M et al (2009) Antimicrobial susceptibility and mechanisms of resistance in Shigella and Salmonella isolates from children under five years of age with diarrhea in rural Mozambique. Antimicrob Agents Chemother 53:2450–2454. https://doi.org/10.1128/AAC.01282-08
Mercante JW, Winchell JM (2015) Current and emerging Legionella diagnostics for laboratory and outbreak investigations. Clin Microbiol Rev 28:95–133. https://doi.org/10.1128/CMR.00029-14
Nisa I, Qasim M, Driessen A, Nijland J, Bari F et al (2020) Molecular epidemiology of Shigella flexneri isolated from pediatrics in a diarrhea-endemic area of Khyber Pakhtunkhwa. Pakistan Eur J Clin Microbiol Infect Dis 39:971–985. https://doi.org/10.1007/s10096-020-03811-0
Patel J (2016) Approved guideline, M-02 and M-07. Clinical and Laboratory Standards Institute (CLSI) performance standards for antimicrobial susceptibility testing M100–S26
Pervin MK, Jhora ST, Paul S, Naher A (2019) Antibiotic sensitivity pattern of diarrhoeal pathogens in under five children. Bangladesh Med J Khulna 52:35–39. https://doi.org/10.3329/bmjk.v52i1-2.46148
Puzari M, Sharma M, Chetia P (2018) Emergence of antibiotic resistant Shigella species: A matter of concern. J Infect Public Health 11.4(2018):451–454. https://doi.org/10.1016/j.jiph.2017.09.025
Rahman MM, Basaglia M, Vendramin E, Boz B, Fontana F et al (2014) Bacterial diversity of a wooded riparian strip soil specifically designed for enhancing the denitrification process. Biol Fertil Soils 50:25–35. https://doi.org/10.1007/s00374-013-0828-0
Rahman MM, Sultana T, Ali MY, Rahman MM, Al-Reza SM et al (2017) Chemical composition and antibacterial activity of the essential oil and various extracts from Cassia sophera L. against Bacillus sp. from soil. Arab J Chem 10:S2132–S2137
Ranjbar R, Farahani A (2019) Shigella: antibiotic-resistance mechanisms and new horizons for treatment. Infect Drug Resist 12:3137. https://doi.org/10.2147/IDR.S219755
Salleh MZ, Nik Zuraina NMN, Hajissa K, Ilias MI, Banga Singh KK, Deris ZZ (2022) Prevalence of multidrug-resistant and extended-spectrum beta-lactamase-producing Shigella Species in Asia: a systematic review and meta-analysis. Antibiotics 11:1653. https://doi.org/10.3390/antibiotics11111653
Sheam MM, Syed S, Bin, Nain Z, Tang SS, Paul DK, Ahmed KR, Biswas SK (2020) Community-acquired pneumonia: aetiology, antibiotic resistance and prospects of phage therapy. J Chemother. https://doi.org/10.1080/1120009X.2020.1807231
Sun Q, Lan R, Wang Y, Zhao A, Zhang S et al (2011) Development of a multiplex PCR assay targeting O-antigen modification genes for molecular serotyping of Shigella flexneri. J Clin Microbiol 49:3766–3770. https://doi.org/10.1128/JCM.01259-11
Ud-Din A, Wahid S (2014) Relationship among Shigella spp. and enteroinvasive Escherichia coli (EIEC) and their differentiation. Braz J Microbiol 45:1131–1138. https://doi.org/10.1590/S1517-83822014000400002
Ud-Din AI, Wahid SU, Latif HA, Shahnaij M, Akter M et al (2013) Changing trends in the prevalence of Shigella species: emergence of multi-drug resistant Shigella sonnei biotype g in Bangladesh. PLoS ONE 8:e82601. https://doi.org/10.1371/journal.pone.0082601
Van den Beld M, Reubsaet F (2012) Differentiation between Shigella, enteroinvasive Escherichia coli (EIEC) and noninvasive Escherichia coli Eur J Clin Microbiol Infect Dis 31:899–904. https://doi.org/10.1007/s10096-011-1395-7
Wajda Ł, Wyderka M, Polak Z, Duda-Chodak A, Makarewicz M (2018) Examination of novel Aureobasidium pullulans isolates dominating apple microflora and assessing their potential for apple juice spoilage. World J Microbiol Biotechnol 34:1–11. https://doi.org/10.1007/s11274-018-2497-5
WHO (1987) Manual for the laboratory investigations of acute enteric infections. WHO/CDD/83.3 rev 1. World Health Organization, Geneva
WHO (1995) Guidelines for the control of epidemics due to Shigella dysenteriae type 1 (WHO/CDR/95.4). World Health Organization, Geneva, Switzerland. WHO (2014). Antimicrobial resistance: global report on surveillance. WHO Press, Genf
Walker JJ, Pace NR (2007) Phylogenetic composition of rocky mountain endolithic microbial ecosystems. Appl Environ Microbiol 73:3497–3504. https://doi.org/10.1128/AEM.02656-06
Wójcicki M, Świder O, Daniluk KJ, Średnicka P, Akimowicz M et al (2021) Transcriptional regulation of the multiple resistance mechanisms in Salmonella—A. Rev Pathogens 10:801. https://doi.org/10.3390/pathogens10070801
Yusuf M, Kalgo ZM, Aliyu B, Adesina MA (2018) Comparative evaluation of stool, urine and blood culture for isolation of Salmonella spp. from patients with clinical evidence of salmonellosis. World J Microbiol 4(1):133–138. https://doi.org/10.3390/pathogens10070801
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study has been approved by the ethical committee of the faculty of Biological Sciences, Islamic University, Kushtia-7003, Bangladesh, dated 10-01-2022 (IU/Bio/Fac/2022/7, dated 10-01-2022). Written informed consent was taken.
Consent to participate
Consent was taken from all participants.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 120 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huq, A.F.M.A., Biswas, S.K., Sheam, M.M. et al. Identification and antibiotic pattern analysis of bacillary dysentery causing bacteria isolated from stool samples of infected patients. Biologia 78, 873–885 (2023). https://doi.org/10.1007/s11756-022-01299-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11756-022-01299-x