Abstract
Wound coverage in the supra-patellar area presents a significant challenge for orthopaedic and reconstructive surgeons due to the need for preservation of knee joint function but the paucity of regional soft tissue flaps available. While many orthopaedic and reconstructive surgeons make use of the rotational gastrocnemius flap for coverage of peri-patellar defects, this flap has certain limitations. The goal of this study was to report a single-centre experience with the use of the distally based anterolateral thigh flap (ALT) and review the current literature on the use of the ALT for peri-patellar defects. In this report, both a single-centre experience using distally based anterolateral thigh (ALT) island flaps for supra-patellar wound coverage and the existing literature on this topic were reviewed. A systematic literature review was performed to assess the use of the ALT for peri-patellar wounds. Five patients with a mean age of 69 underwent a distally based ALT flap for coverage of peri-patellar defects. Four out of 5 flaps survived at the end of their respective follow-up. Based on this combined experience, the distally based reverse-flow anterolateral thigh island flap represents a useful but relatively underutilized option for appropriately selected supra-patellar wounds due to minimal donor site morbidity, multiple flap components, and predictable pedicle anatomy. The flap’s major weakness is its potentially unreliable venous drainage, requiring delay or secondary venous outflow anastomosis. Given the ALT flap’s favourable profile, the authors recommend consideration for its use when managing a peri-patellar coverage wound issue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peri-patellar wound coverage presents a significant challenge due to the paucity of regional soft tissue flaps and the need to preserve knee function. This is especially true for the superior half of the knee joint, where the gastrocnemius muscles do not typically extend. Whereas local tissue rearrangements and advancements have been reported to be effective for smaller defects, and free flaps have been used successfully to cover larger wounds, these methods have certain disadvantages for large wounds at or above the level at which the gastrocnemius reaches. The gastrocnemius flap has historically been the flap of choice for most orthopaedic and reconstructive surgeons for wounds at or below the level of the patella [1, 2]. The distally based, reverse-flow anterolateral thigh (ALT) island flap described in this report solves many of the problems left unaddressed by the gastrocnemius flap. It is an important treatment option that should be recognized by orthopaedic surgeons and included in the reconstructive surgeon’s armamentarium [3, 4].
Materials and methods
An Institutional Review Board (IRB)-approved retrospective review of prospectively acquired data from authors’ database was performed. Inclusion criteria were reconstructive procedures of peri-patellar wounds performed between 2011 and 2015 with distally based ALT flaps. Any cases where other types of distally based flaps were used were excluded. Over the length of the study period, approximately 40 flap surgeries were performed for peri-patellar wounds. Five consecutive patients, 4 females and 1 male, were identified. Patient ages ranged from 50 to 85, with a mean age of 69. Distally based anterolateral lateral thigh island flaps were used for coverage of soft tissue defects created after wide excision of sarcoma arising in the peri-patellar or lower thigh region in 2 cases, or skin and soft tissue defects resulting from dehisced total knee arthroplasty wounds in 3 cases (Table 1). Intraoperatively, irrigation and debridement, and antibiotic spacer exchange were initially performed by an orthopaedic surgeon prior to flap dissection. Post-operatively, patients were maintained in either a knee immobilizer or a hinged knee brace and were mobilized non-weight-bearing for 2–6 weeks, depending on wound characteristics. Subsequently, patients were encouraged to begin progressive weight bearing as tolerated along with an instructed physical therapy regimen. Follow-up ranged from 1 to 36 months, with mean follow-up of 19 months.
Surgical technique
The site of the peri-patellar defect was measured. A skin paddle was designed over the anterolateral thigh in the standard position of an ALT free flap. The axis was drawn between the anterior superior iliac spine (ASIS) and lateral border of patella, which identifies the septum between the rectus femoris and vastus lateralis muscles, with the descending branch of the lateral femoral cutaneous artery (dLFCA) contained within. The proximal dLFCA and descending branch of the lateral femoral cutaneous vein (dLFCV) were identified, and proximal perforators into the skin paddle were noted. The proximal dLFCA and dLFCV were clamped, and perfusion to the skin paddle was assessed. At that point, perfusion was assumed to be supplied via the distal perforator arising from the superolateral genicular artery and forming a natural anastomosis with the distal lateral cutaneous femoral artery. If the skin paddle appeared congested or if arterial inflow was questionable, near-infrared laser angiography (SPY, Novadaq, Toronto, CA) was employed to assess the arterial inflow and venous outflow to the flap. If arterial inflow was suboptimal with the proximal pedicle clamped, the use of the distally based flap was aborted. If the venous outflow was suboptimal and the flap was congested, the flap was delayed for a period of 2–3 weeks to allow for intra-flap adjustment of venous drainage. A slip of vastus lateralis, tensor fascia lata, or both was harvested depending on need for soft tissue coverage. The distal perforator was then identified, and the flap was islanded by incising the skin and subcutaneous tissue just distal to this perforator. Once islanded, the entire flap was either tunnelled into the wound beneath subcutaneous tissue or inlaid into the wound by incising the intervening soft tissues. The donor site was closed primarily without tension when possible, or loosely approximated and overlaid with a split thickness skin graft (STSG) and negative pressure wound vacuum-assisted closure device where primary closure was deemed inappropriate.
Results
Musculofasciocutaneous flaps were used in all cases, with flap sizes ranging from 15 × 7 cm to 24 × 9 cm. Each flap contained at least two perforators. Four out of 5 flaps survived to the end of their respective follow-up. The necrosed flap occurred in a patient with persistent peri-prosthetic infection and subsequent arterial occlusion distal to the popliteal artery, which required above the knee amputation of the ipsilateral extremity 1 month after the index procedure. One flap was found to exhibit intraoperative venous congestion and its harvest was delayed initially, with successful delayed coverage 1 week later. In one case, the medial head of the gastrocnemius muscle was used to cover a soft tissue defect not corrected by the anterolateral thigh flap alone. All flaps developed partial skin necrosis to varying degrees post-operatively, which was treated with wound care, negative pressure vacuum-assisted therapy, serial irrigation and debridement, and additional split thickness skin grafts as appropriate (Table 1). At the end of follow-up, 3 patients had minimal residual knee pain, functional knee joint flexion, and ambulated either unassisted or with a cane. One patient developed persistent knee stiffness, limited knee flexion to 40 degrees, and ambulated with a cane.
Discussion
Peri-patellar and especially supra-patellar soft tissue defects represent a difficult reconstructive problem for orthopaedic and reconstructive surgeons due to paucity of soft tissue options in the region. Coverage of defects following oncological resection or salvage of infected knee prostheses requires healthy, well-vascularized soft tissue to maintain function and, ultimately, preserve the limb. In addition to restoring aesthetic appearance and skin integrity, orthopaedic and reconstructive surgeons must consider functional outcomes and the importance of restoration of the extensor mechanism of the knee joint. Local advancement and rotational flaps such as saphenous flaps or pedicled gastrocnemius flaps have been employed extensively for that role [5, 6]. However, drawbacks of these flaps include sensory deficits, possible need for STSG at the donor site, incomplete coverage for extensive tissue defects, decreased ipsilateral plantar flexion strength, and suboptimal overall functional outcomes [7,8,9]. These flaps are not well suited for subgroups of patients with loss of knee extensor mechanisms and need for tendon allograft. Alternatively, free flaps have been successfully used to address these shortcomings in coverage of complex peri-patellar defects; however, these flaps are associated with increased surgical time and require special facilities and microsurgical equipment [8]. The location of the recipient vessels represents an additional challenge for reconstructive surgeons intending to use a free flap for peri-patellar wound coverage.
First described by Song and Lou in 1984, the anterolateral thigh (ALT) flap quickly became a workhorse in myriad indications [10]. Available as free or pedicled flap, the ALT flap has been successfully used in the reconstruction of defects in various locations including lower/upper extremities, trunk, and head and neck [11, 12]. Advantages of the ALT flap include long pedicle, minimal donor site morbidity, its potential to be harvested using a 2-team approach, reliable flap anatomy, and multiple flap components (skin, fat, fascia, muscle, tendon, nerve), providing potential for tendon reconstruction and a neurovascular pedicle with sensate skin [13, 14].
The ALT is supplied by one to three perforators from the descending branch of the lateral circumflex femoral artery (LCFA) in more than 90% of cases. The descending branch was postulated to form a natural anastomosis with the lateral superior geniculate artery (LSGA) and/or profunda femoral artery [15]. Other anatomic variations might include a perforator arising from the deep femoral artery or a cutaneous perforator of the transverse branch of the LCFA. Shieh and Erba described at least four different types of perforator patterns arising from the main blood supply. Types I and III represent musculocutaneous and septocutaneous perforators, respectively, originating from the descending branch of the LCFA, whereas type II and IV perforators take route from the transverse branch of LCFA [16, 17]. The authors argued that type II and IV perforators preclude safe island flap harvest; however, subsequent reports have described successful island flaps using such perforators [18, 19]. Perforators differ in their course as well, and a hybrid musculoseptocutaneous perforator vessel has recently been reported as the most common vessel found radiographically, followed by strictly septocutaneous and musculocutaneous perforators [20].
The distally based anterolateral thigh island flap as first described by Wong was found to be a viable alternative to a free flap for local defect coverage [13]. The distal perforator was found to provide enough perfusion for the flap in most cases, with studies showing up to 80% of flow velocity of the original blood flow [15]. Other studies also suggested adequate peri- and post-operative blood flow by measuring velocity and oxygen perfusion of perforator flaps [21]. Recent cadaveric and imaging studies have established a relatively consistent distal vascular supply pattern for the distally based island ALT flap, with the proximal and distal perforators localized within 4–6 cm of the initial incision midpoint [18, 20, 22]. Others have suggested that anatomy is rather variable [23,24,25,26]. As such, clamping of the proximal vascular pedicle with either testing of skin bleeding or intraoperative laser angiography to ensure adequate perfusion from the distal perforator is always advised before committing to flap transfer; additionally, preoperative vascular mapping might be a useful adjunct to intraoperative imaging modalities [15, 20, 23, 24, 27, 28]. Near-infrared laser angiography using indocyanine green allows for assessment of perforator zones of perfusion prior to, and during flap harvest. This supplemental tool is an improvement over computed tomographic angiography (CTA) in that it provides dynamic information about perfusion without the radiation risk imposed by CTA. Additionally, it is superior to a unidirectional Doppler in that it can quantify relative tissue perfusion where the Doppler may locate small perforators that may be unable to support the flap [29].
Likewise, venous congestion is a problem characteristic of all reverse-flow flaps. This potential complication is described for the reverse-flow ALT and has been attributed to the resistance from venous valves seen with retrograde flow, as well as the possible tensioning and kinking of vessels that occurs during flap insetting. Acute venous congestion can be dealt with by flap delay, venous augmentation, vein grafting for bypass, or conversion to a free flap. Insidious development of venous congestion necessitates close monitoring with possible need for irrigation and debridement, negative pressure vacuum-assisted therapy, or venous supercharging [30]. This potential complication has also been reported to be successfully identified and prevented with preservation of a subcutaneous strip ranging from distal flap end to upper knee [18]. Alternatively, antegrade venous drainage through the microsurgical anastomosis with the proximal dLCFV was reported to effectively resolve venous congestion in at least one case [19]. Preventative venous supercharging during initial harvest represents an additional technique for minimizing venous congestion [31, 32].
The use of distally based anterolateral thigh flap represents an attractive option for reconstruction of peri-patellar soft tissue defects and has been reported in a few case reports and case series to date. Despite the potential functional and aesthetic benefits afforded by the use of this flap, it remains an underutilized option for wound coverage. To date, there exists a paucity of published literature describing the results of this flap for peri-patellar soft tissue defects. Pertinent results for each case series included are presented and discussed in brief (Table 2).
Chen et al. reported one case of a distally based ALT, 18 × 10 cm in size, for coverage of a fourth-degree burn in a distal thigh location, with the patient able to ambulate independently at 3-month follow-up [28]. The authors used a splint for 1 week post-operatively, with an early rehabilitation programme initiated promptly after. Similarly, Heo et al. published a case report of peri-patellar defect coverage with a distally based ALT. Preoperative computed tomographic angiography (CTA) was used to identify perforators, and an 8 cm × 10 cm flap was isolated with excellent functional outcome and no reported complications at 2-month follow-up [23]. Erba et al. described three cases with distally based ALT for defect closure after radical excision of malignant sarcoma of the lateral knee [18]. Their protocol included the initiation of physical therapy at 2 weeks post-operatively, with two patients ambulating by 2 weeks and achieving full range of motion at 2-month follow-up. All flaps survived and follow-up at 2 years was without complication. Additionally, Liu et al. reported on three cases of ALT island flap elevation to repair knee defects resulting from crush injuries [33]. These knee defects ranged from 3 × 6 cm to 26 × 8 cm. The authors described a standard ALT flap elevation technique, with the pedicle pivot point 6–7 cm above the knee joint. All three flaps survived; however, small areas of necrosis requiring debridement were noted at the margins in two out of three cases. Each series demonstrates minimal donor site morbidity with good functional outcomes.
Nosrati et al. reported on their experience with 5 cases of ALT flaps for coverage of knee defects as part of a larger series of 48 free or pedicled ALT flaps utilized for lower extremity defects [34]. Three free flaps and two pedicled flaps were used, with one of the pedicled flaps performed as a reverse-flow myocutaneous flap and the other as reversed vastus lateralis muscle-only flap covered with a split thickness skin graft. Two complications occurred, a recipient site wound dehiscence and a donor site haematoma, with all but one patient returning to preoperative functional status. Demirseren et al. presented their results on 17 reverse-flow distally based ALT flaps for reconstruction of peri-patellar defects and upper third of ipsilateral leg [35]. All flaps survived, and only two flaps developed partial necrosis at the distal ends, which improved after debridement. These slightly larger series demonstrate the flexibility that the ALT affords for reconstructive options.
Lastly, the chimeric ALT flap as described by Zheng et al. in their series provides for maximal versatility in reconstructing complex, irregular soft tissue defects. This flap is harvested using multiple tissue components such as muscle, fascia, and skin each supplied by a separate perforator off of the descending branch of the LCFA, providing for multiple spatially independent components to reconstruct composite defects [36]. The five lower leg defects repaired from their series of 22 patients ranged from 12 × 18 cm to 35 × 43 cm with complete flap survival in 4 and partial skin graft loss in one. At mean follow-up of 24 months, all wounds healed well with good contour in the reconstructed areas, no donor site complications, and no functional limitations.
Limitations
While providing a significant soft tissue source for extensive coverage, ALT flap thickness can be a disadvantage, necessitating future debulking if the initial flap is thicker than the defect. Flap thickness has been extensively studied in Asian and Western populations, with greater thickness seen in the latter [20]. Although one-stage flap thinning techniques have been described, this carries additional risks of devitalizing the flap [37]. The subcutaneous fat thickness of the patients in this series was not such as to require thinning by either suction-assisted lipectomy or excisional techniques.
Additionally, the flap dissection can be laborious and complex with critical emphasis on the careful identification of a pivot point for the flap, as well as prevention of pedicle compression after transfer. The requirement for microsurgery is another potential limitation for this flap, as medical centres may lack the necessary equipment. Finally, the ALT has an uncommon but well-recognized possibility of anatomic variation that can provide for a difficult harvest in rare cases [22, 23, 35].
Conclusions
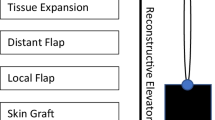
The distally based reverse-flow anterolateral thigh island flap is a useful option for the coverage of peri-patellar wounds. It has the advantages of minimal donor site morbidity, reliable flap-harvesting approach, and multiple flap components. Despite these benefits, there are fewer than 100 cases reported worldwide to date, representing a significant underuse of this flap. In our opinion, the ALT flap represents an essential component of an orthopaedic and reconstructive surgeon’s armamentarium for addressing peri-patellar and especially supra-patellar wounds and should be included as a reconstructive ladder option when considering coverage options.
References
Suda AJ, Cieslik A, Grützner PA, Münzberg M, Heppert V (2014) Flaps for closure of soft tissue defects in infected revision knee arthroplasty. Int Orthop 38(7):1387–1392. https://doi.org/10.1007/s00264-014-2316-z
Rao AJ, Kempton SJ, Erickson BJ, Levine BR, Rao VK (2016) Soft tissue reconstruction and flap coverage for revision total knee arthroplasty. J Arthroplast 31(7):1529–1538. https://doi.org/10.1016/j.arth.2015.12.054
Kimata Y, Uchiyama K, Ebihara S et al (2000) Anterolateral thigh flap donor-site complications and morbidity. Plast Reconstr Surg 106(3):584–589. http://www.ncbi.nlm.nih.gov/pubmed/10987464. Accessed 31 Dec 2016
Kuo YR, Jeng SF, Kuo MH et al (2001) Free anterolateral thigh flap for extremity reconstruction: clinical experience and functional assessment of donor site. Plast Reconstr Surg 107(7):1766–1771. http://www.ncbi.nlm.nih.gov/pubmed/11391197. Accessed 31 Dec 2016
Healy C, Tiernan E, Lamberty BG, Campbell RC (1995) Rotation fasciocutaneous flap repair of lower limb defects. Plast Reconstr Surg 95(2):243–251. http://www.ncbi.nlm.nih.gov/pubmed/7824603. Accessed 31 Dec 2016
Gravvanis A, Kyriakopoulos A, Kateros K, Tsoutsos D (2014) Flap reconstruction of the knee: a review of current concepts and a proposed algorithm. World J Orthop 5(5):603–613. https://doi.org/10.5312/wjo.v5.i5.603
Gravvanis AI, Iconomou TG, Panayotou PN, Tsoutsos DA (2005) Medial gastrocnemius muscle flap versus distally based anterolateral thigh flap: conservative or modern approach to the exposed knee joint? Plast Reconstr Surg 116(3):932–934. https://doi.org/10.1097/01.prs.0000181662.94027.3c
Akhtar MS, Khan AH, Khurram MF, Ahmad I (2014) Inferiorly based thigh flap for reconstruction of defects around the knee joint. Indian J Plast Surg 47(2):221–226. https://doi.org/10.4103/0970-0358.138954
Daigeler A, Drücke D, Tatar K et al (2009) The pedicled gastrocnemius muscle flap: a review of 218 cases. Plast Reconstr Surg 123(1):250–257. https://doi.org/10.1097/PRS.0b013e3181904e2e
Song SH, Choi S, Kim YM, Lee SR, Choi YW, Oh SH (2013) The composite anterolateral thigh flap for knee extensor and skin reconstruction. Arch Orthop Trauma Surg 133(11):1517–1520. https://doi.org/10.1007/s00402-013-1833-3
Gravvanis A, Tsoutsos D, Karakitsos D et al (2006) Application of the pedicled anterolateral thigh flap to defects from the pelvis to the knee. Microsurgery 26(6):432–438. https://doi.org/10.1002/micr
Sadigh PL, Wu C-J, Shih H-S, Jeng S-F (2013) Reverse anterolateral thigh flap to revise a below-knee amputation stump at the mid-tibial level. Plast Reconstr Surg Glob Open 1(9):e88. https://doi.org/10.1097/GOX.0000000000000030
Wong C-H, Wei F-C (2010) Anterolateral thigh flap. Head Neck 32(4):529–540. https://doi.org/10.1002/hed.21204
Wong C-H, Goh T, Tan B-K, Ong YS (2012) The anterolateral thigh perforator flap for reconstruction of knee defects. Ann Plast Surg 70(3):1. https://doi.org/10.1097/SAP.0b013e318234e8e2
Pan S-C, Yu J-C, Shieh S-J, Lee J-W, Huang B-M, Chiu H-Y (2004) Distally based anterolateral thigh flap: an anatomic and clinical study. Plast Reconstr Surg 114(7):1768–1775. https://doi.org/10.1097/01.PRS.0000142416.91524.4C
Shieh SJ, Chiu HY, Yu JC, Pan SC, Tsai ST, Shen CL (2000) Free anterolateral thigh flap for reconstruction of head and neck defects following cancer ablation. Plast Reconstr Surg 105(7):2349–2357. https://doi.org/10.1097/00006534-200006000-00006
Koshima I (2000) Free anterolateral thigh flap for reconstruction of head and neck defects following cancer ablation. Plast Reconstr Surg 105(7):2358–2360. https://doi.org/10.1097/00006534-200006000-00006
Erba P, Raffoul W, Bauquis O (2012) Safe dissection of the distally based anterolateral thigh flap. J Reconstr Microsurg 28(6):405–411. https://doi.org/10.1055/s-0032-1315764
Lin RY-C, Chien W-H (2006) Experiences in harvesting type II distally based anterolateral thigh flaps. Plast Reconstr Surg 118(1):282–286. https://doi.org/10.1097/01.prs.0000222243.18349.52
Seth R, Manz RM, Dahan IJ et al (2011) Comprehensive analysis of the anterolateral thigh flap vascular anatomy. Arch Facial Plast Surg. 13(5):347–354. https://doi.org/10.1001/archfacial.2011.16
Gravvanis A, Tsoutsos D, Karakitsos D, Iconomou T, Papadopoulos O (2007) Blood perfusion of the free anterolateral thigh perforator flap: its beneficial effect in the reconstruction of infected wounds in the lower extremity. World J Surg 31(1):11–18. https://doi.org/10.1007/s00268-006-0298-8
Gao S-H, Feng S-M, Chen C, Jiao C, Sun L-Q, Zhang W-L (2012) A new recipient artery for reconstruction of soft-tissue defects in the lower limb with a free anterolateral thigh flap: the reversed descending branch of the lateral femoral circumflex artery. Plast Reconstr Surg 130(5):1059–1065. https://doi.org/10.1097/PRS.0b013e318267d3a3
Heo C, Eun S, Bae R, Minn K (2010) Distally based anterolateral-thigh (ALT) flap with the aid of multidetector computed tomography. J Plast Reconstr Aesthet Surg 63(5):e465–e468. https://doi.org/10.1016/j.bjps.2009.08.009
Cotrufo S, Hart A (2010) A note of caution on the use of the distally based anterolateral thigh flap: anatomical evidence. Plast Reconstr Surg 125(1):30e–31e. https://doi.org/10.1097/PRS.0b013e3181c2a40f
Yamada S, Okamoto H, Sekiya I et al (2014) Anatomical basis of distally based anterolateral thigh flap. J Plast Surg Hand Surg 48(3):197–200. https://doi.org/10.3109/2000656X.2013.859146
Lakhiani C, Lee MR, Saint-Cyr M (2012) Vascular anatomy of the anterolateral thigh flap: a systematic review. Plast Reconstr Surg 130(6):1254–1268. https://doi.org/10.1097/PRS.0b013e31826d1662
Zhou G, Zhang QX, Chen GY (2005) The earlier clinic experience of the reverse-flow anterolateral thigh island flap. Br J Plast Surg 58(2):160–164. https://doi.org/10.1016/j.bjps.2004.10.011
Chen C-Y, Hsieh C-H, Kuo Y-R, Jeng S-F (2007) An anterolateral thigh perforator flap from the ipsilateral thigh for soft-tissue reconstruction around the knee. Plast Reconstr Surg 120(2):470–473. https://doi.org/10.1097/01.prs.0000267432.03348.97
Sacks JM, Nguyen AT, Broyles JM (2012) Imaging for optimizing the design of the anterolateral thigh flap. Eplasty 12(30):278–285
Kim I, Kim T, Lee J, Kim Y, Park K (2012) The clinical course of reverse-flow anterolateral thigh flap: need to prepare for venous congestion and salvage operation. Arch Plast Surg 39(3):262–264
Lin C-H, Zelken J, Hsu C-C, Lin C-H, Wei F-C (2016) The distally based, venous supercharged anterolateral thigh flap. Microsurgery 36(1):20–28. https://doi.org/10.1002/micr.22380
Yeh HK, Hsu CC, Lin CH et al (2015) Reverse-flow anterolateral thigh flap without antegrade venous reconstruction for knee soft-tissue reconstruction. Formos J Surg 48(1):21–25. https://doi.org/10.1016/j.fjs.2014.07.002
Liu T-Y, Jeng S-F, Yang JC-S, Shih H-S, Chen C-C, Hsieh C-H (2010) Reconstruction of the skin defect of the knee using a reverse anterolateral thigh island flap: cases report. Ann Plast Surg 64(2):198–201. https://doi.org/10.1097/SAP.0b013e31819bd6f7
Nosrati N, Chao AH, Chang DW, Yu P (2012) Lower extremity reconstruction with the anterolateral thigh flap. J Reconstr Microsurg 28(4):227–233. https://doi.org/10.1055/s-0032-1306370
Demirseren ME, Efendioglu K, Demiralp CO, Kilicarslan K, Akkaya H (2011) Clinical experience with a reverse-flow anterolateral thigh perforator flap for the reconstruction of soft-tissue defects of the knee and proximal lower leg. J Plast Reconstr Aesthet Surg 64(12):1613–1620. https://doi.org/10.1016/j.bjps.2011.06.047
Zheng X, Zheng C, Wang B et al (2016) Reconstruction of complex soft-tissue defects in the extremities with chimeric anterolateral thigh perforator flap. Int J Surg 26:25–31. https://doi.org/10.1016/j.ijsu.2015.12.035
Ross GL, Dunn R, Kirkpatrick J et al (2003) To thin or not to thin: the use of the anterolateral thigh flap in the reconstruction of intraoral defects. Br J Plast Surg 56(4):409–413. https://doi.org/10.1016/S0007-1226(03)00126-7
Lu M, Sun G, Hu Q, Tang E, Wang Y (2015) Functional assessment: free thin anterolateral thigh flap versus free radial forearm reconstruction for hemiglossectomy defects. Med Oral Patol Oral Cir Bucal 20(6):e757–e762. https://doi.org/10.4317/medoral.20727
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
This study was approved by the institutional review board. Informed consent was waived for all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bekarev, M., Goch, A.M., Geller, D.S. et al. Distally based anterolateral thigh flap: an underutilized option for peri-patellar wound coverage. Strat Traum Limb Recon 13, 151–162 (2018). https://doi.org/10.1007/s11751-018-0319-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11751-018-0319-9