Abstract
Background
Flap reconstruction with perforator, fasciocutaneous, muscular, and/or free microvascular flaps is utilized to cover wound defects and improve vascularization and antibiotic/nutrient delivery. Flap use in revision procedures for total knee arthroplasty has been explored previously; however, current data are limited and studies comparing healing and complication rates between different flap types are lacking.
Methods
A literature review was performed using PubMed on 13 January 2022. Studies were included if they reported healing and complication rates for either gastrocnemius, rectus abdominis, latissimus dorsi, fasciocutaneous, chimeric, or gracilis flaps in the setting of revision total knee arthroplasty (TKA).
Results
The final cohort included gastrocnemius (n = 421, healing rate 73.8%, complication rate 59.9%), gracilis (n = 9, healing rate 93%, complication rate 55.6%), latissimus dorsi (n = 41, healing rate 67%, complication rate 46.3%), rectus abdominis (n = 3, healing rate 100%, complication rate 0%), fasciocutaneous (n = 78, healing rate 70%, complication rate 19.2%), and chimeric flaps (n = 4, healing rate 100%, complication rate 25%). There was no significant difference when comparing healing rates across flap types (p = 0.39). There was a significant difference when comparing complication rates across flap types (p < 0.0001), with a significant difference being noted between gastrocnemius and fasciocutaneous complication rates (p < 0.0001). All other comparisons between flap types by complication rate were not significantly different.
Conclusions
Gastrocnemius flaps are the workhorse flap in the setting of revision TKA, as evidenced by this review. Healing rates did not vary significantly across flap types, which suggests that determining the appropriate flap for coverage of soft-tissue defects in revision TKA should be driven by defect size and location as well as physician experience and patient tolerance.
Similar content being viewed by others
Background
Total knee arthroplasty (TKA) provides excellent results for most patients, with literature estimating revision rates less than 5.0% over 10 years [1]. However, complications from TKA revision surgeries are high and include wound dehiscence, infection, aseptic loosening, and, in cases where the limb cannot be salvaged, above-knee amputation (in 0.1% of cases) [2, 3]. An exposed prosthetic implant after TKA poses substantial risk to patient morbidity and mortality. In the setting of either septic or aseptic soft tissue loss, flap reconstruction is a viable treatment option.
Thus, the indications for flap use in the setting of revision TKA include but are not limited to infection [4], implant exposure [5], disruption of the extensor mechanism (from patellar tendon tear/avulsion, patellar fracture, or quadriceps tendon tear) [6], soft-tissue coverage [7], and limb salvage [8]. In particular, the flap pattern provides a vascular supply for an overlying skin graft, which improves oxygen and nutrient delivery to the overlying skin graft and the underlying anatomic structures. Further, improved blood supply facilitates dissemination of systemic antibiotics to the surgical site, thereby decreasing nidus for future infections.
Flap use in revision procedures for TKA has been explored frequently, with various studies commenting on the operative technique and effectiveness. However, the current data reported on flap use in revision TKA are mainly outdated and limited to case reports, case series, technical tricks, and small sample size (Tables 1, 2, 3, 4, 5, 6, 7). Furthermore, studies comparing healing rates between different flap types are lacking [7, 9]. Therefore, the aim of this review is to provide a concise review of the current literature on this topic and to assess the healing and complication rates for each commonly used flap type in the setting of revision TKA.
Approach for flap reconstruction
The current accepted version of the reconstructive ladder was proposed by Gottlieb et al. [10], who proposed the concept of a “reconstructive elevator” as opposed to the “reconstructive ladder,” the main difference being that clinicians should opt for the most appropriate flap rather than the least complex [11] (Fig. 1). In the traditional model, to utilize a local and/or distant flap, clinicians were first advised to begin with primary closure followed by a skin graft. To attempt a more directed approach, especially in the setting of TKA, local (or rotational) and distant (or free) flaps may be attempted directly. Some primary considerations for flap choice include donor site morbidity and defect size. In the setting of TKA, while gastrocnemius flaps have been well described as the main workhorse flap, studies have suggested that superior geniculate artery perforator flaps in place of gastrocnemius flaps or anterolateral thigh flaps in place of rectus or latissimus dorsi flaps may result in less donor site morbidity [11]. It is the aim of this review that, by presenting updated data on healing and complication rates for various flap types, surgeons may be better informed when deciding on flap reconstruction techniques. Institutional review board approval was not required for this review.

Adapted from Gottlieb et al. (Gottlieb LJ, Krieger LM (1994). From the reconstructive ladder to the reconstructive elevator. Plast Reconstr Surg 93:1503–1504)
Reconstructive elevator. This methodology encourages surgeons to pick the most appropriate flap type as opposed to addressing flap reconstruction in a sequential, least-complex method.
Methods
Literature search strategy
The methodology utilized in this systematic review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A comprehensive search of the PubMed electronic database was conducted on 13 January 2022. The following keywords were entered into the search engine: ("Surgical Flaps"[Mesh] OR (muscle flaps) OR flaps[tiab] OR "surgical flaps"[tiab] OR Gastrocnemius [tiab] OR "Anterolateral Thigh"[tiab] OR "Rectus Abdominis"[tiab] OR "Rectus Abdominis"[Mesh] OR "Latissimus Dorsi"[tiab] OR "Superficial Back Muscles"[Mesh] OR Fasciocutaneous[tiab] OR Chimeric[tiab] OR "Chimera"[Mesh] OR Gracilis[tiab] OR "Gracilis Muscle"[Mesh]) AND ("Arthroplasty, Replacement, Knee"[Mesh] OR ("Reconstructive Surgical Procedures"[Mesh] AND "Knee"[Mesh]) OR (total knee arthroplast*) OR TKA OR (total knee replacement) OR (revision total knee arthroplast*) OR (revision total knee replacement)).
Eligibility criteria
To meet inclusion criteria, articles needed to be (1) published in the English language, (2) have full-text information readily available online, (3) report flap coverage to treat exposed primary total knee arthroplasty (TKA) following infection using either gastrocnemius, rectus abdominis, latissimus dorsi, fasciocutaneous, chimeric, or gracilis flaps, (4) report clinical outcomes that include complications and survival or wound healing rates related to the flap, and (5) have a minimum follow-up of at least 1 year. Articles were excluded from our final analysis if they (1) did not meet inclusion criteria, (2) studied flap coverage in revision surgeries unrelated to an exposed TKA (e.g., arthrodesis, trauma of the native joint), (3) were in vitro studies (including biomechanical studies), review articles, systematic reviews, or letters to the editor, (3) reported nonclinical outcomes, or (4) reported treatment on any joint that is not the knee.
Study selection
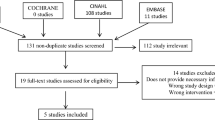
The initial systematic search generated a total of 385 studies. Two reviewers (A.A.C. and A.T.) independently screened each article for eligibility, extracted data on a separate spreadsheet, and evaluated the methodology and level of evidence for quality assurance. Any disagreement between the two reviewers was resolved through consultation with the senior author (R.S.Y.). Out of the 385 studies identified, only 66 studies were included for full-text review. Of the 66 full-text reviews, 28 studies were excluded while 38 studies were included for qualitative/quantitative analysis (Fig. 2).
Data extraction
Patients were then divided into different groups based on flap type: gastrocnemius, rectus abdominis, latissimus dorsi, fasciocutaneous, chimeric, or gracilis flaps. The primary outcome was flap survival/wound healing rates and complications compared between the different groups (Table 1).
Statistical analysis
Descriptive data are reported as counts (%). To compare data between each groups, continuous variables (i.e., demographic data) were analyzed using independent t-tests for parametric variables and Mann–Whitney U test for nonparametric variables, while categorical variables (i.e., wound healing and complications data) were analyzed using chi-squared tests. Statistical significance was set at p ≤ 0.05. All statistical analyses were performed using SPSS version 25 (IBM Corporation, Armonk, New York).
Flap introduction and operative anatomy
Pedicled/local flaps
Gastrocnemius
The gastrocnemius muscle’s medial head originates from the posterior medial femoral condyle, while the lateral head extends from the posterior lateral femoral condyle; the two parts combine distal to the myotendinous junction and form an aponeurosis, which combines with the aponeurosis of the soleus muscle to become the Achilles tendon [12]. The gastrocnemius is supplied by the sural arteries (downstream of the popliteal artery) and is drained via the popliteal vein; the muscle mainly aids in plantar flexion and supination of the foot by coordination from the tibial nerve [13].
Walton et al. described the operative approach for completing a lateral gastrocnemius muscle flap [14]. In their description, the first incision is made 2 cm posterior to and parallel to the fibula beginning at the level of the fibular head and extending 10 cm above the distal fibula. Distally, the muscle is followed until the Achilles tendon and carefully resected; a portion of the Achilles tendon may also be taken to aid in reconstruction. The lateral flap is then rotated anteriorly over the fibula to cover soft-tissue defects.
For a medial gastrocnemius flap, an incision may be made from the medial tibia (posterior to the pes anserine tendons) and extended until the superficial posterior compartment until about 10 cm superior to the ankle; in particular, the sural artery should be identified early [14]. The neurovascular structures in the posterior compartment must be preserved to ensure proper growth of the flap. The gastrocnemius muscle can then be rotated over the anterior aspect of the knee to cover a soft-tissue defect either via a subcutaneous tunnel or by dividing the intervening skin bridge.
Gracilis
The gracilis muscle is a long and thin unipennate muscle in the medial compartment of the thigh that originates on the medial aspect of the ischiopubic ramus and joins with the sartorius and semitendinosus muscle tendons to form the pes anserine [15]. It is primarily supplied by the medial circumflex femoral artery and branches of the superior femoral artery with innervation from the anterior branch of the obturator nerve [7].
Rao et al. described the operative approach for completing a gracilis muscle flap [7, 16, 17]. For this procedure, the patient is placed supine and the thigh is abducted. The gracilis muscle may be located by palpating 2–3 cm posterior from a line connecting the pubic symphysis to the medial condyle. The vascular supply to the gracilis muscle may be palpated and confirmed with Doppler ultrasonography 8–10 cm inferior to the pubic tubercle. Rao et al. recommend the use of a 10–15 cm sagittal incision from the pubis to the medial anterior knee to blunt dissect the gracilis from the sartorius and the semimembranosus muscles [7]. The vascular pedicles may be found running superficial to the adductor magnus muscle, underneath the adductor longus. When retracting the adductor longus muscle, the artery may be traced to its origins off the medial circumflex femoral artery. The muscle should then be released from its superior attachment site, reversed 180°, and tunneled under the skin to reach the defect over the knee.
Free flaps
Latissimus dorsi
The latissimus dorsi (LD) muscle is one of the most used free flaps for patients undergoing TKA with infected knees and/or extensive soft-tissue defects such as an exposed prosthesis, followed by the rectus abdominis muscle [7, 18, 19]. It may be taken as either a muscle or myocutaneous flap with sufficient bulk to cover large volumes of dead space [17]. A major disadvantage of using an LD flap is its high rate of donor site complications, which includes wound dehiscence, seroma, and functional morbidity limiting overhead activities [7, 18, 19].
When harvesting the LD flap, the patient is placed in a lateral decubitus position. An oblique incision is made along the anterior aspect of the muscle. The flap is elevated off the posterior thorax from its broad origin, which extends from the thoracic spinous processes and posterior iliac crest and is excised in cephalad direction toward the axilla at its humeral insertion. Segmental perforating vessels are ligated sequentially if necessary, while care is taken to protect the dominant pedicle, which is primarily supplied by the thoracodorsal artery [7, 18,19,20,21,22].
Rectus abdominis
The rectus abdominis serves as an excellent source for a free flap in the setting of revision knee arthroplasty as it provides a reliable anatomy with a large area for soft-tissue coverage when regional rotational flaps do not suffice [23]. It can be harvested with the patient supine with relatively low patient morbidity as a muscle-only, myofascial, or commonly as a myocutaneous flap without the need for any intraoperative position changes. When taken as a myocutaneous flap, the need for a separate split-thickness skin graft can be avoided depending on the size of the soft-tissue deficit.
The paired rectus abdominis muscles arise from the pubic symphysis and crest and insert onto the fifth, sixth, and seventh costal cartilages, providing truck flexion. The rectus abdominis is divided by fibrous tendinous intersections and is enclosed by an anterior and posterior sheath bound laterally by the linea semilunaris and medially by the linea alba. The investing rectus sheath is formed from contribution from the internal oblique, external oblique, and transverse abdominis fascia. The rectus abdominis is supplied by two dominant vascular pedicles: the deep superior and inferior epigastric vessels. The inferior epigastric artery, which enters the lateral border of the rectus muscle just beneath the arcuate line, is preferred for usage as a vascular pedicle [24,25,26].
During harvest, a longitudinal incision is made down to the level of the anterior rectus sheath with elevation of skin and subcutaneous tissue. The muscle can be freed from the posterior fascia and harvested separately when a muscle-only flap is used. Care is taken to identify and protect the inferior epigastric vessels as well as the integrity of the posterior sheath as the vessel runs deep to the muscle belly and superficial to the fascia.
Additional flap types
Fasciocutaneous
The use of local fasciocutaneous (FC) perforator flaps was first described in the leg by Pontén in 1981 and was later used by Lewis et al. to cover exposed knees [27, 28]. They consist of skin, subcutaneous tissue, and deep fascia, and offer great value in repairing soft-tissue defects around the knee with reduced functional morbidity at the donor site, resistance to infection, and an improved aesthetic result [18, 29]. The vascular supply comes from perforating arteries that enter the deep fascia either through an underlying muscle, within the intermuscular septum between adjacent muscles, or via a direct cutaneous branch [18, 29]. Commonly used FC flaps include the anterolateral thigh flap, sural artery flap, saphenous artery flap, genicular artery flaps, and anterior tibial artery flap [19].
Chimeric
Chimeric flaps are a more recent development in the realm of skin coverage for wound coverage. Chimeric flaps have been described for over 40 years, but their popularity has increased owing to their versatility as of late. Chimeric flaps are typically made up of at least one muscle perforator flap component and can be either perforator based or branch based [30]. Perforator-based chimeric flaps are composed of multiple independent flaps in which perforators arise from a common source vessel, whereas branch-based chimeric flaps are composed of multiple independent flaps that arise from independent subfascial branches of a common source vessel [30]. Because of this, there are often a number of different anatomical areas from which a chimeric flap may be derived [31,32,33,34,35,36,37]. However, chimeric flaps reported for TKA reconstruction have mainly used the gastrocnemius muscle–chimeric sural artery perforator flap or anterolateral thigh (ALT) perforator flap taken with vascularized fascia lata [30, 31, 37, 38].
The gastrocnemius muscle–chimeric sural artery perforator flap receives its source vessel from the medial or lateral sural artery and is taken with the medial or lateral gastrocnemius, respectively [30, 39]. To summarize, the medial and lateral sural arteries are the most common branches that arise from the popliteal artery. They traverse down their respective head of the gastrocnemius along the deep surface. Their course then pierces their respective muscle, as musculocutaneous perforators, continuing through the deep fascia and continuing to the subdermal plexus. The largest perforators, best for flap creation, are typically found in the distal half of the gastrocnemius muscles and more commonly come from the medial sural artery.
The chimeric flap utilizing a ALT perforator flap combined with fascia lata is prepared in the same fashion as described in an earlier section. In brief, the ALT is supplied by the lateral femoral circumflex artery (LCFA) and can be harvested as either an FC flap or as a myocutaneous flap, depending on the presence or absence of the septocutaneous perforator vessels that branch off the LCFA [40]. An additional step is taken to harvest a portion of the fascia lata as the ALT perforator flap is being harvested [31, 36].
Results
A total of six flap types were identified for inclusion in this review: (1) gastrocnemius (n = 421), (2) rectus abdominis (n = 3), (3) latissimus dorsi (n = 41), (4) fasciocutaneous (n = 78), (5) chimeric (n = 4), and (6) gracilis (n = 9) (Table 1).
Healing rates across flap types ranged from ~ 70% to 100%: (1) gastrocnemius (n = 311, 73.8%), (2) rectus abdominis (n = 3, 100%), (3) latissimus dorsi (n = 27, 67%), (4) fasciocutaneous (n = 55, 70%), (5) chimeric (n = 4, 100%), and (6) gracilis (n = 8, 93%) (Table 1). There was no significant difference when comparing healing rates across flap types (p = 0.39).
Complication rates across flap types ranged from ~ 20% to 60%: (1) gastrocnemius (n = 252, 59.9%), (2) rectus abdominis (n = 0, 0%), (3) latissimus dorsi (n = 19, 46.3%), (4) fasciocutaneous (n = 15, 19.2%), (5) chimeric (n = 1, 25%), and (6) gracilis (n = 5, 55.6%) (Table 1). There was a significant difference when comparing complication rates across flap types (p < 0.0001), with a significant difference being noted between gastrocnemius (59.9%) and fasciocutaneous (19.2%) complication rates (p < 0.0001). All other comparisons between flap types by complication rate were not significantly different.
Healing and complication rates by study and follow-up times were recorded for each individual study (Tables 2–7).
Discussion
In this review, gastrocnemius flaps were the most utilized in the setting of revision TKA. While there was a significant difference noted between the complication rates for gastrocnemius versus fasciocutaneous flaps (p < 0.0001), healing rates across flap types were not significantly different (p = 0.39). The significant difference in complication rates between gastrocnemius and FC flaps may be explained by gastrocnemius flaps being frequently utilized for large wound defects in clinically complex cases, whereas fasciocutaneous flaps may be reserved for smaller wound defects. These data suggest that all flap types are viable depending on the extent of the wound defect and demonstrate equivalent, moderate wound healing rates with a minimum 1-year follow-up.
Pedicled/local flaps
Gastrocnemius
In this review, we noted that the gastrocnemius flap was the most utilized flap type (n = 421), with a healing rate of 73.8% and complication rate of 59.9% (Table 1, 2). Many studies have confirmed the benefit and safety of rotational gastrocnemius flaps in TKA revision, noting that they produce greater results than primary closure alone [5, 6, 41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61]. Busfield et al. noted a 100% return in extensor function in a cohort of patients (n = 9) who underwent gastrocnemius muscle flap coverage [6]. They determined that medial gastrocnemius flap reconstruction could provide a successful salvage therapy in the setting of failed extensor mechanism allograft or an alternative for patients with poor soft-tissue coverage, infection, or debilitating medical conditions. Corten et al. noted a satisfactory result in 92% of patients (n = 24) who underwent gastrocnemius muscle flap coverage of infected TKA at a mean follow-up of 4.5 years (range 1–10 years) [3].
Gastrocnemius flaps have also been reported to increase tissue delivery of antibiotics because of increased blood flow to surgical sites and its properties as a natural spacer and cover for prostheses [62]. Carlesimo et al. reported a clinical absence of reinfection postoperatively in TKA patients with rotation flap who underwent 6 weeks of antibiotic therapy (n = 8) [62]. When assessing long-term outcomes of gastrocnemius flap use in TKA, a study by Houdek et al. noted that, of 83 patients in whom a gastrocnemius flap had been used (n = 18 for primary procedure and n = 65 for revision procedure), the 10-year revision and amputation-free survival rates following gastrocnemius flap coverage were 68% and 79%, respectively.[63]
Gracilis
The gracilis muscle flap has been shown to be useful for knee resurfacing, especially in the treatment of suprapatellar defects, with negligible donor site morbidity [8, 16, 17, 64, 65]. Previous articles have demonstrated its utility as a substitute for or supplement to gastrocnemius muscle flaps in the treatment of suprapatellar defects with negligible donor site morbidity [16, 17]. Tiengo et al. studied the use of an extended reversed gracilis flap in three patients with severe soft-tissue defects following infected TKA with a mean follow-up of 23.3 months (range 22–24 months) and found that all three cases successfully healed without complication or evidence of infection at latest follow-up [17]. In another study, Jung et al. followed one patient, who previously underwent multiple TKA revisions due to recurrent infection, being treated with a reverse gracilis muscle flap and reported no complications during a 24-month follow-up period [22].
Last, Chim et al. demonstrated the role of the gracilis muscle as a supplementary flap in augmenting coverage provided by gastrocnemius muscle flaps in two patients with mid- and distal femur osteosarcoma, respectively [8]. Both flaps survived without complications with excellent wound healing, and their patients were able to ambulate independently in the postoperative period. The authors concluded that there is utility in using the gracilis muscle for additional coverage, especially in cases that necessitate a long femoral stem replacement.
These studies have produced findings in line with our current study results, which have shown a 93% healing rate with the use of the gracilis muscle flaps (n = 9). (Tables 1, 7).
Free flaps
Latissimus dorsi
In this review, LD flaps (n = 41) had a healing rate of 67% and complication rate of 46.3% (Table 1). Common complications for this flap type included recurrent infection, wound dehiscence, and flap failure (Tables 1, 4).
The use of an LD flap offers a reliable and durable option for wounds requiring extensive soft-tissue coverage and does not cause any functional restrictions in the knee joint [7, 66]. Early studies on treating and prophylactic LD flaps revealed promising limb salvage and healing rates, although not without complication [20, 21, 67]. In an early case series performed by Markovich et al., 12 patients undergoing TKA with muscle flap coverage were studied [22]. Five patients received LD free flaps either for prophylactic soft-tissue coverage done before definitive reconstruction (n = 2) or for treating muscle flap for infected prostheses with deficient soft-tissue coverage (n = 3). The wound was revascularized successfully in all knees with satisfactory healing of the muscle flap and subsequent healing of the implant. One patient treated with a prophylactic LD flap experienced late infection, though the authors attributed this to the use of a large tibial allograft to cover an additional bony defect. Two patients with chronic knee infection treated with LD muscle flaps experienced recurrent infection and subsequent second reimplantation and resection arthroplasty, respectively. Ultimately, the authors concluded that success in patients treated with muscle flaps is dependent on the reason for and the timing of the muscle flap. Thus, treating muscle flaps used for chronic knee infections had the worst outcomes, whereas prophylactic muscle flaps used for soft-tissue coverage for knees with adherent skin and scar tissue achieved greater success.
In another study, Cetrulo et al. studied the use of free tissue transfer on 11 patients with complex wounds and exposed prostheses, which included 6 cases of LD muscle flaps [20]. In their review, all of their free flaps were successful. The authors achieved limb salvage in all of their patients and prosthesis salvage in all but one patient who had their prosthesis removed at an outside hospital followed by knee arthrodesis. Hierner et al. reported the use of LD myocutaneous free flaps in 14 patients with insufficient soft tissue for prophylactic coverage in TKA [21]. Primary wound healing was achieved in eight patients, while skin breakdown occurred in five patients requiring secondary skin grafting, and fasciocutaneous flap in one patient.. There were three late recurrences of infection, with ultimate removal of the knee prosthesis followed by conversion to arthrodesis. Overall, the authors concluded that free myocutaneous LD flap transfer made TKA prosthesis implantation possible, prevented postoperative knee stiffness, and had a low rate of severe complications in patients with a high risk of wound-healing problems.
Lastly, a recent study conducted by Raymond et al. reviewed 18 consecutive patients with multiply revised TKA and LD free flap reconstruction [66]. Median follow-up time for their patients was 49 months (range 18–110 months). At latest follow-up, they found that 14 of 18 patients (77.8%) had maintained their implant. Seven of those patients were infection-free, while another seven were on suppressive antibiotics with the implant in situ and four had above-knee amputations. They reported a 5-year revision-free implant survival of 75% and found low functional outcome scores at latest follow-up. Thus, the authors concluded that LD free flap was a viable option for limb salvage, but that functional outcomes can be poor and there may be a significant risk of ongoing infection and amputation.
Rectus abdominis
Overall, our review found a 100% success rate in three patients reviewed with no complications reported (Tables 1, 3). Browne et al. were one of the first to recommend the utilization of the rectus abdominis flap as a salvage procedure for compromised soft tissue associated with total knee arthroplasty [68]. Here, they reported nine patients undergoing muscle flap for salvage of chronically infected total knee arthroplasty that required a two-stage revision. The study included seven patients undergoing local gastrocnemius flaps and two patients undergoing free flap for large soft-tissue defects: one latissimus dorsi and one rectus abdominis. Browne et al. reported 100% clearance of infection with successful reimplantation at 6 and 12 weeks respectively for the latissimus dorsi and rectus abdominis flaps without complications. Five of seven patients (71.4%) undergoing gastrocnemius flaps had successful reimplantation with additional complications of skin graft loss and loss of distal segment of the gastrocnemius flap.
Markovich et al. also utilized the rectus abdominis free flap as a salvage procedure for compromised tissues associated with total knee arthroplasty [67]. Here they described 12 patients who underwent muscle flaps for different indications and treatments goals: (1) prophylactic soft-tissue coverage, done before definitive reconstruction; (2) muscle flaps for treating infected prostheses with deficient soft tissue; and (3) salvage muscle flaps for wound dehiscence in the immediate postoperative period. Two of the 12 patients underwent rectus abdominis free flaps, the first for prophylactic coverage and the second for salvage for wound dehiscence. They overall reported a 100.0% successful revascularization rate at 4.1 years follow-up. Both patients treated with rectus abdominis flaps had successful clearance of infection and healed with limb salvage and improvements in arc of motion as compared with preoperatively, without complications.
Cetrulo et al. reported on 11 patients who underwent free tissue transfer in the setting of exposed hardware and complex wounds after total knee arthroplasty [20]. Six of these 11 patients underwent free rectus abdominis transfer, with the remaining 5 undergoing latissimus dorsi transfers. Despite 3 of the 11 patients having failed previous local rotational flaps, Certulo et al. achieved a 100% success rate and 100% limb salvage rate. One latissimus flap required explant and primary fusion owing to advanced bone loss and osteolysis, resulting in an overall 91% prosthetic retainment rate. No functional outcome scores were reported, but all patients remained ambulatory postoperatively.
While the rectus abdominis free flaps are a great option with high success rates in both limb and prosthesis salvage, their indications are more limited to larger defects in the often multiply revised patient. As compared with the more convenient and accessible local rotational flaps, rectus abdominis free flaps have been less reported in the literature but appear to have high successful healing rates with low complications reported.
Additional flap types
Fasciocutaneous
In this review, fasciocutaneous flaps had a healing rate of 70.0% and a complication rate of 19.2% (Table 1) Common causes of complications included amputation, arthrodesis, wound dehiscence, and revision procedures (Tables 1, 5).
Historically, FC flaps have been used to preserve cutaneous innervation and manage incisional skin necrosis after TKA in patients without underlying deep infection or large defects such as an exposed prosthesis [19, 56, 58, 61, 64, 69,70,71,72]. In a case series of 17 patients performed by Menderes et al. in which 7 TKA patients received a FC flap for wound coverage, the authors found modest success with limb salvage and complication rate [19]. Three of the seven patients required a revision procedure with a medial gastrocnemius myocutaneous flap in place of the failed FC flap. The secondary surgical procedures of these three patients would go on to heal without complication. Therefore, the authors concluded that FC flaps are preferred when the soft defect is small, without exposure of the prosthesis. Adam et al. retrospectively studied 25 TKA cases using 9 FC flaps and 16 muscle flaps over a mean follow-up time of 5.4 years (range 1–10 years) and found that all of their patients with FC flaps healed successfully compared with 10 out of 16 muscle flaps [5]. However, the authors noted that this may be attributed to the fact that they used FC flaps for small defects whereas muscle flaps were used for major wound dehiscence. Conversely, Vaienti et al. studied the use of island neurofasciocutaneous sural flaps in 15 patients with exposed TKA prostheses over a mean follow-up period of 18 months and reported great success in limb salvage [73]. All of their flaps survived, and only two cases of hematoma and one case of recurrent aseptic fistula occurred. Siim et al. reviewed 18 cases (10 local FC flaps) with an average follow-up of 7 years (range 1–17 years), and noted that FC flap use may result in successful outcomes with early reconstructive surgery in TKA patients with sufficient soft-tissue coverage; however, long-term outcomes are variable [74].
The use of unilateral or bilateral local FC flaps in a V–Y pattern has also been shown to reliably cover soft-tissue defects more than 2 cm wide following TKA and obviate the need for secondary skin grafting [72]. Misra and Niranjan conducted a retrospective series following 15 patients who used local FC flaps for patellar and peripatellar defects, with 8 of their 15 study patients receiving a V–Y flap design [75]. They found healing success in 100% of their patients with minimal complications as only one patient experienced wound dehiscence. All patients achieved a “good” outcome with a mean follow-up of 13 months (range 3–24 months).
Chimeric
Chimeric flaps were one of the least reported flap types in the setting of TKA revision. In this review, we noted a 100% (n = 4) healing rate for the gastrocnemius muscle–chimeric sural artery perforator flap and ALT perforator flap combined with fascia lata as reported by a few case studies (Tables 1, 6) [30, 31, 37, 38]. Hallock et al. studied two patients being treated with the gastrocnemius muscle–chimeric sural artery perforator flap for wound coverage, one of who underwent TKA revision with a medial gastrocnemius muscle and medial sural artery perforator flap [30]. They experienced a minor complication due to iatrogenic causes caused by their orthopedic service, which led to devascularization of the chimeric flap during reimplantation that necessitated revision with a lateral gastrocnemius muscle and lateral sural artery perforator. The flap went on to heal uneventfully 1 year out. Their case highlights the importance of interdisciplinary collaboration between orthopedic surgeons and plastic surgeons to optimize patient outcomes, especially those undergoing revision TKA requiring a flap for soft-tissue coverage.
Han et al. also reported the use of a medial gastrocnemius muscle and medial sural artery perforator flap in two patients undergoing TKA revision and did not observe any postoperative complications [37]. In another study, Cho et al. followed six patients, one of who received a chimeric flap consisting of medial gastrocnemius muscle component and a medial sural artery adipofascial component, for soft-tissue coverage due to infection following TKA. At 36-month follow-up, their patient had full range of motion and no gait disturbance [38]. Lastly, Fu et al. studied the use of the chimeric ALT perforator flap with fascia lata in one patient who had skin necrosis following TKA and found no complications after a 12-month follow-up period [31].
Overall, the lack of literature reporting these flaps suggests that chimeric flaps may not be utilized as frequently, possibly because of their extensive surgical exposure and lack of available data on long-term outcomes. However, as the small sample shows, chimeric flaps do have promise in the setting of TKA revision surgery, with minimal donor site morbidity and functional impairment.
Study limitations
There are limitations to this review worth reporting. First, the decision-making process utilized by operating surgeons when deciding on which flap type to utilize for their patient cohorts was not readily known. Second, not all studies uniformly reported healing and complication rates, requiring authors to extrapolate this information from descriptive results, figures, and supplemental files within the studies; this limitation also prevented this review from performing a formal review process or aggregating data to conduct a meta-analysis.
Conclusions
Gastrocnemius flaps are by far the most utilized flap type in the setting of revision TKA. Healing rates in this review did not vary significantly across flap types, which suggests that all flap types are viable depending on the extent of the wound defect and demonstrate equivalent, moderate wound healing rates with a minimum 1-year follow-up. The appropriate flap for coverage of soft-tissue defects in TKA revision is based on defect size/location, physician experience, and patient tolerance. We envision that multidisciplinary collaboration and proper patient follow-up will be key to exploring flap use in revision TKA procedures in the coming years.
Availability of data and materials
Not applicable. All studies included in this review are available online.
Abbreviations
- TKA:
-
Total knee arthroplasty
- LD:
-
Latissimus dorsi
- LFCA:
-
Lateral femoral circumflex artery
- FC:
-
Fasciocutaneous
References
Lützner J, Hübel U, Kirschner S, Günther KP, Krummenauer F (2011) Long-term results in total knee arthroplasty. A meta-analysis of revision rates and functional outcome. Chirurg 82(7):618–624
Postler A, Lützner C, Beyer F, Tille E, Lützner J (2018) Analysis of total knee arthroplasty revision causes. BMC Musculoskelet Disord 19(1):55
Corten K, Struelens B, Evans B, Graham E, Bourne RB, MacDonald SJ (2013) Gastrocnemius flap reconstruction of soft-tissue defects following infected total knee replacement. Bone Jt J 95(9):1217–1221
Schmidt I (2017) The role of gastrocnemius muscle flap for reconstruction of large soft tissue defects after infected total knee arthroplasty. Int J Case Rep Images 8(1):7–10
Adam RF, Watson SB, Jarratt JW, Noble J, Watson JS (1994) Outcome after flap cover for exposed total knee arthroplasties. A report of 25 cases. J Bone Jt Surg Br 76(5):750–753
Busfield BT, Huffman GR, Nahai F, Hoffman W, Ries MD (2004) Extended medial gastrocnemius rotational flap for treatment of chronic knee extensor mechanism deficiency in patients with and without total knee arthroplasty. Clin Orthop Relat Res 428:190–197
Rao AJ, Kempton SJ, Erickson BJ, Levine BR, Rao VK (2016) Soft tissue reconstruction and flap coverage for revision total knee arthroplasty. J Arthroplasty 31(7):1529–1538
Chim H, Tan BK, Tan MH, Tan KC, Song C (2007) Optimizing the use of local muscle flaps for knee megaprosthesis coverage. Ann Plast Surg 59(4):398–403
Cho EH, Shammas RL, Carney MJ, Weissler JM, Bauder AR, Glener AD, Kovach SJ, Hollenbeck ST, Levin LS (2018) Muscle versus fasciocutaneous free flaps in lower extremity traumatic reconstruction: a multicenter outcomes analysis. Plast Reconstr Surg 141(1):191–199
Gottlieb LJ, Krieger LM (1994) From the reconstructive ladder to the reconstructive elevator. Plast Reconstr Surg 93(7):1503–1504
Janis JE, Kwon RK, Attinger CE (2011) The new reconstructive ladder: modifications to the traditional model. Plast Reconstr Surg 127(Suppl 1):205S-212S
Hsu D, Chang KV (2020) Gastrocnemius strain. StatPearls edn, Treasure Island
Bordoni B, Varacallo M (2020) Anatomy, bony pelvis and lower limb. Gastrocnemius muscle. StatPearls, Treasure Island
Walton Z, Armstrong M, Traven S, Leddy L (2017) Pedicled rotational medial and lateral gastrocnemius flaps: surgical technique. J Am Acad Orthop Surg 25(11):744–751
Khan IA, Bordoni B, Varacallo M (2020) Anatomy, bony pelvis and lower limb, thigh gracilis muscle. StatPearls, Treasure Island
Jung JA, Kim YW, Cheon YW (2013) Reverse gracilis muscle flap: an alternative means of skin coverage for recurrent infection after TKA. Knee Surg Sports Traumatol Arthrosc 21(12):2779–2783
Tiengo C, Macchi V, Vigato E, Porzionato A, Stecco C, Azzena B, Morra A, De Caro R (2010) Reversed gracilis pedicle flap for coverage of a total knee prosthesis. J Bone Jt Surg Am 92(7):1640–1646
Osei DA, Rebehn KA, Boyer MI (2016) Soft-tissue defects after total knee arthroplasty: management and reconstruction. J Am Acad Orthop Surg 24(11):769–779
Menderes A, Demirdover C, Yilmaz M, Vayvada H, Barutcu A (2002) Reconstruction of soft tissue defects following total knee arthroplasty. Knee 9(3):215–219
Cetrulo CL Jr, Shiba T, Friel MT, Davis B, Buntic RF, Buncke GM, Brooks D (2008) Management of exposed total knee prostheses with microvascular tissue transfer. Microsurgery 28(8):617–622
Hierner R, Reynders-Frederix P, Bellemans J, Stuyck J, Peeters W (2009) Free myocutaneous latissimus dorsi flap transfer in total knee arthroplasty. J Plast Reconstr Aesthet Surg 62(12):1692–1700
Pusic AL, Chen CM, Patel S, Cordeiro PG, Shah JP (2007) Microvascular reconstruction of the skull base: a clinical approach to surgical defect classification and flap selection. Skull Base 17(1):5–16
Meland NB, Fisher J, Irons GB, Wood MB, Cooney WP (1989) Experience with 80 rectus abdominis free-tissue transfers. Plast Reconstr Surg 83(3):481–487
Boyd JB, Taylor GI, Corlett R (1984) The vascular territories of the superior epigastric and the deep inferior epigastric systems. Plast Reconstr Surg 73(1):1–16
Pennington DG, Pelly AD (1980) The rectus abdominis myocutaneous free flap. Br J Plast Surg 33(2):277–282
Perrault D, Manrique OJ, Lee G, Carre AL, Oakes DA, Wong AK (2019) Complex reconstruction of the knee with a free vertical rectus abdominis flap after periprosthetic soft tissue necrosis. Cureus 11(1):e3969
Pontén B (1981) The fasciocutaneous flap: its use in soft tissue defects of the lower leg. Br J Plast Surg 34(2):215–220
Lewis VL, Mossie RD, Stulberg DS, Bailey MH, Griffith BH (1990) The fasciocutaneous flap: a conservative approach to the exposed knee joint. Plast Reconstr Surg 85(2):252–257
Boretto JG, De Cicco FL (2020) Fasciocutaneous flaps. StatPearls, Treasure Island (FL)
Hallock GG (2008) Chimeric gastrocnemius muscle and sural artery perforator local flap. Ann Plast Surg 61(3):306–309
Fu J, Qing L, Wu P, Tang J (2021) Customized reconstruction of a complex soft-tissue defect around the knee with a free perforator flap. Am J Transl Res 13(5):4401–4411
Sano K, Hallock GG, Ozeki S, Suzuki H, Mawatari R, Yoshino K, Hamazaki M (2006) Devastating massive knee defect reconstruction using the cornucopian chimera flap from the subscapular axis: two case reports. J Reconstr Microsurg 22(1):25–32
Yamamoto T, Yamamoto N (2021) A triple-component deep inferior epigastric artery perforator chimeric free flap for three-dimensional reconstruction of a complex knee defect complicated with patella osteomyelitis. Microsurgery 41(4):370–375
Al-Himdani S, Din A, Wright TC, Wheble G, Chapman TWL, Khan U (2020) The medial sural artery perforator (MSAP) flap: a versatile flap for lower extremity reconstruction. Injury 51(4):1077–1085
Kim SW, Kim KN, Hong JP, Park SW, Park CR, Yoon CS (2015) Use of the chimeric anterolateral thigh free flap in lower extremity reconstruction. Microsurgery 35(8):634–639
Kuo YR, An PC, Kuo MH, Kueh NS, Yao SF, Jeng SF (2008) Reconstruction of knee joint soft tissue and patellar tendon defects using a composite anterolateral thigh flap with vascularized fascia lata. J Plast Reconstr Aesthet Surg 61(2):195–199
Han SE, Lee KT, Mun GH (2014) Muscle-chimaeric medial sural artery perforator flap: a new design for complex three-dimensional knee defect. J Plast Reconstr Aesthet Surg 67(4):571–574
Cho YJ, Lee JH, Chung DW (2017) Pedicled chimeric gastrocnemius-medial sural artery adipofascial flap for reconstruction of anterolateral defects of the knee. Microsurgery 37(3):206–211
Sano K, Hallock GG, Hamazaki M, Daicyo Y (2004) The perforator-based conjoint (chimeric) medial Sural(MEDIAL GASTROCNEMIUS) free flap. Ann Plast Surg 53(6):588–592
Kuo YR, Seng-Feng J, Kuo FM, Liu YT, Lai PW (2002) Versatility of the free anterolateral thigh flap for reconstruction of soft-tissue defects: review of 140 cases. Ann Plast Surg 48(2):161–166
Auregan JC, Lin JD, Lombardi JM, Jang E, Macaulay W, Rosenwasser MP (2016) The hemisoleus rotational flap provides a novel superior autograft reconstructive option for the treatment of chronic extensor mechanism disruption. Arthroplast Today 2(2):49–52
Bonnin M, Lustig S, Huten D (2016) Extensor tendon ruptures after total knee arthroplasty. Orthop Traumatol Surg Res 102(1 Suppl):S21-31
Casanova D, Hulard O, Zalta R, Bardot J, Magalon G (2001) Management of wounds of exposed or infected knee prostheses. Scand J Plast Reconstr Surg Hand Surg 35(1):71–77
Jaureguito JW, Dubois CM, Smith SR, Gottlieb LJ, Finn HA (1997) Medial gastrocnemius transposition flap for the treatment of disruption of the extensor mechanism after total knee arthroplasty. J Bone Joint Surg Am 79(6):866–873
Anract P, Missenard G, Jeanrot C, Dubois V, Tomeno B (2001) Knee reconstruction with prosthesis and muscle flap after total arthrectomy. Clin Orthop Relat Res 384:208–216
Chiou HM, Chang MC, Lo WH (1997) One-stage reconstruction of skin defect and patellar tendon rupture after total knee arthroplasty. A new technique. J Arthroplasty 12(5):575–579
Gerwin M, Rothaus KO, Windsor RE, Brause BD, Insall JN (1993) Gastrocnemius muscle flap coverage of exposed or infected knee prostheses. Clin Orthop Relat Res 286:64–70
McPherson EJ, Patzakis MJ, Gross JE, Holtom PD, Song M, Dorr LD (1997) Infected total knee arthroplasty. Two-stage reimplantation with a gastrocnemius rotational flap. Clin Orthop Relat Res 341:73–81
Papp A, Kettunen J, Miettinen H (2003) Pedicled gastrocnemius flap in complicated total knee arthroplasty. Scand J Surg 92(2):156–159
Pozzobon LR, Helito CP, Guimaraes TM, Gobbi RG, Pecora JR, Camanho GL (2013) Rotation flaps for coverage after total knee arthroplasty. Acta Ortop Bras 21(4):219–222
Tetreault MW, Della Valle CJ, Hellman MD, Wysocki RW (2017) Medial gastrocnemius flap in the course of treatment for an infection at the site of a total knee arthroplasty. JBJS Essent Surg Tech 7(2):e14
Ries MD, Bozic KJ (2006) Medial gastrocnemius flap coverage for treatment of skin necrosis after total knee arthroplasty. Clin Orthop Relat Res 446:186–192
Warren SI, Murtaugh TS, Lakra A, Reda LA, Shah RP, Geller JA, Cooper HJ (2018) Treatment of periprosthetic knee infection with concurrent rotational muscle flap coverage is associated with high failure rates. J Arthroplasty 33(10):3263–3267
Boopalan PR, Daniel AJ, Chittaranjan SB (2009) Managing skin necrosis and prosthesis subluxation after total knee arthroplasty. J Arthroplasty 24(2):322.e323-327
Moog P, Tinwald I, Aitzetmueller M, Bauer AT, Megerle K, Machens HG, Laszlo Kovacs L, Kuekrek H (2020) The usage of pedicled or free muscle flaps represents a beneficial approach for periprosthetic infection after knee arthroplasty. Ann Plast Surg 85(5):539–545
Nahabedian MY, Mont MA, Orlando JC, Delanois RE, Hungerford DS (1999) Operative management and outcome of complex wounds following total knee arthroplasty. Plast Reconstr Surg 104(6):1688–1697
Ng SW, Fong HC, Tan BK (2018) Two sequential free flaps for coverage of a total knee implant. Arch Plast Surg 45(3):280–283
Suda AJ, Cieslik A, Grützner PA, Münzberg M, Heppert V (2014) Flaps for closure of soft tissue defects in infected revision knee arthroplasty. Int Orthop 38(7):1387–1392
Tetreault MW, Della Valle CJ, Bohl DD, Lodha SJ, Biswas D, Wysocki RW (2016) What factors influence the success of medial gastrocnemius flaps in the treatment of infected TKAs? Clin Orthop Relat Res 474(3):752–763
Theil C, Stock ME, Gosheger G, Moellenbeck B, Schwarze J, Schmidt-Braekling T (2020) Gastrocnemius muscle flaps for soft tissue coverage in periprosthetic knee joint infection. J Arthroplasty 35(12):3730–3736
Young K, Chummun S, Wright T, Darley E, Chapman TW, Porteous AJ, Murray JR, Khan U (2016) Management of the exposed total knee prosthesis, a six-year review. Knee 23(4):736–739
Carlesimo B, Marchetti F, Tempesta M, Marcasciano M, Ruggiero M, Scuderi N (2013) Muscular gastrocnemius spacer: a two stage reimplantation technique for infected total knee arthroplasty. Ann Ital Chir 84(2):179–185
Houdek MT, Wagner ER, Wyles CC, Harmsen WS, Hanssen AD, Taunton MJ, Moran SL (2018) Long-term outcomes of pedicled gastrocnemius flaps in total knee arthroplasty. J Bone Jt Surg Am 100(10):850–856
Gravvanis A, Kyriakopoulos A, Kateros K, Tsoutsos D (2014) Flap reconstruction of the knee: a review of current concepts and a proposed algorithm. World J Orthop 5(5):603–613
Mitsala G, Varey AH, O’Neill JK, Chapman TW, Khan U (2014) The distally pedicled gracilis flap for salvage of complex knee wounds. Injury 45(11):1776–1781
Raymond AC, Liddle AD, Alvand A, Donaldson JR, Carrington RWJ, Miles J (2021) Clinical outcome of free latissimus dorsi flaps for coverage of soft tissue defects in multiply revised total knee arthroplasties. J Arthroplasty 36(2):664–669
Markovich GD, Dorr LD, Klein NE, McPherson EJ, Vince KG (1995) Muscle flaps in total knee arthroplasty. Clin Orthop Relat Res 321:122–130
Browne EZ Jr, Stulberg BN, Sood R (1994) The use of muscle flaps for salvage of failed total knee arthroplasty. Br J Plast Surg 47(1):42–45
Hallock GG (1990) Salvage of total knee arthroplasty with local fasciocutaneous flaps. J Bone Jt Surg A 72(8):1236–1239
Kovacs L, Zimmermann A, Juhnke P, Taskov C, Papadopulos NA, Biemer E (2006) Soft tissue defects as a complication in knee arthroplasty. Surgical strategies for soft tissue reconstruction. Orthopade 35(2):162–168
Nahabedian MY, Orlando JC, Delanois RE, Mont MA, Hungerford DS: Salvage procedures for complex soft tissue defects of the knee. 119–124; 1998
Papaioannou K, Lallos S, Mavrogenis A, Vasiliadis E, Savvidou O, Efstathopoulos N (2010) Unilateral or bilateral V–Y fasciocutaneous flaps for the coverage of soft tissue defects following total knee arthroplasty. J Orthop Surg Res 5(1):1
Vaienti L, Menozzi A, Lonigro J, Soresina M, Ravasio G (2010) The salvage of knee-exposed prosthesis using neurofasciocutaneous sural flap. Musculoskeletal Surg 94(1):33–40
Siim E, Jakobsen IE, Medgyesi S (1991) Soft-tissue procedures for the exposed knee arthroplasty. 18 cases followed for 7 (1–17) years. Acta Orthop Scand 62(4):312–314
Misra A, Niranjan NS (2005) Fasciocutaneous flaps based on fascial feeder and perforator vessels for defects in the patellar and peripatellar regions. Plast Reconstr Surg 115(6):1625–1632
Acknowledgements
The authors would like to acknowledge Yingting Zhang, Research Services Librarian at Rutgers Robert Wood Johnson Library of the Health Sciences, for her assistance with the literature search.
Funding
No grants, funding, or technical support were received by any of the authors for this project.
Author information
Authors and Affiliations
Contributions
A.A.C., F.R., A.T., L.M., and M.Z. analyzed and interpreted literature regarding reconstructive flap use in revision total knee arthroplasty procedures. A.A.C., F.R., L.M., A.T., and R.S.Y. were major contributors in writing and editing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. Institutional review board approval was not required for this review.
Consent for publication
Not applicable.
Competing interests
The author(s) declare(s) that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chandra, A.A., Romanelli, F., Tang, A. et al. A comparison of healing and complication rates between common flaps utilized in total knee arthroplasty: a review of the literature. Knee Surg & Relat Res 34, 15 (2022). https://doi.org/10.1186/s43019-022-00145-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43019-022-00145-3