Abstract
Research has observed increased mortality among older people attending the emergency department (ED) who had systolic pressure > 7 mmHg lower than baseline primary care values. This study aimed to (1) assess feasibility of identifying this ‘relative hypotension’ using readily available ED data, (2) externally validate the 7 mmHg threshold, and (3) refine a threshold for clinically important relative hypotension. A single-centre retrospective cohort study linked year 2019 data for ED attendances by people aged over 64 to hospital discharge vital signs within the previous 18 months. Frailty and comorbidity scores were calculated. Previous discharge (‘baseline’) vital signs were subtracted from initial ED values to give individuals’ relative change. Cox regression analysis compared relative hypotension > 7 mmHg with mean time to mortality censored at 30 days. The relative hypotension threshold was refined using a fully adjusted risk tool formed of logistic regression models. Receiver operating characteristics were compared to NEWS2 models with and without incorporation of relative systolic. 5136 (16%) of 32,548 ED attendances were linkable with recent discharge vital signs. Relative hypotension > 7 mmHg was associated with increased 30-day mortality (HR 1.98; 95% CI 1.66–2.35). The adjusted risk tool (AUC: 0.69; sensitivity: 0.61; specificity: 0.68) estimated each 1 mmHg relative hypotension to increase 30-day mortality by 2% (OR 1.02; 95% CI 1.02–1.02). 30-day mortality prediction was marginally better with NEWS2 (AUC: 0.73; sensitivity: 0.59; specificity: 0.78) and NEWS2 + relative systolic (AUC: 0.74; sensitivity: 0.63; specificity: 0.75). Comparison of ED vital signs with recent discharge observations was feasible for 16% individuals. The association of relative hypotension > 7 mmHg with 30-day mortality was externally validated. Indeed, any relative hypotension appeared to increase risk, but model characteristics were poor. These findings are limited to the context of older people with recent hospital admissions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Compared to younger people, changes in older people’s vital signs are associated with larger increases in absolute mortality [1]. The most common composite risk score for vital signs, National Early Warning Score v2 (NEWS2), has limitations when applied to older people, having recently been demonstrated to underestimate mortality risk for this group [2, 3]. Absolute thresholds for normal or abnormal continuous data values lack clinical meaningfulness as normal ranges differ in this group, and the overall scores may have less prominence in clinical decision making [4, 5].
Age alters physiological responses to acute health problems such as infection and trauma. Older people are more likely to be living with hypertension, and so when NEWS2 is calculated, blood pressure significantly lower than their usual may still fall within the ‘normal’ range (Fig. 1). Similarly, older people more often use medications such as beta blockers which blunt adaptive responses.
There is no established definition for ‘baseline’ blood pressure. A recent Dutch study obtained a value for baseline systolic blood pressure for older people attending Emergency Departments (ED) by querying primary care and outpatient records and taking the mean of three most recent values [6]. Increased mortality was observed in the tercile with greatest relative reduction, among whom systolic pressure was at least 7 mmHg below baseline. However, in practice Emergency Departments often do not have good access to primary care vital signs data, so this may not be a feasible way of establishing baseline blood pressure. Vital signs recorded during previous hospital episodes, however, are often readily available, particularly where systems use electronic patient records (EPR).
It is not known if using previous hospital readings of vital signs can give a useful baseline against which to judge the relative blood pressure change measured on presentation to the ED, or if relative hypotension against this baseline is a risk factor for mortality.
Objectives
This was a pragmatic initial exploratory analysis using data readily obtainable in real-world emergency care. This study served firstly to assess the feasibility of using previous hospital admission data as a baseline measurement of relative hypotension, and secondly as an external validation of the thresholds derived from primary care data described by Candel et al. [6] which observed greater mortality among people with relative hypotension exceeding 7 mmHg. Finally, we aimed to refine a threshold for relative hypotension that ED clinicians might consider clinically important, developing a risk tool to predict 30-day mortality and comparing the discriminatory performance to NEWS2.
Methods
This retrospective cohort study analysed data which were electronically collected routinely in the ED and inpatient wards from implementation of an EPR to end-2019. In our UK institution, web-based EPR software (NerveCentre) displays not only current and previous ED vital signs observations, but also those recorded during previous inpatient admissions. The EPR has been used for all adult inpatient observations (except Intensive Care) since 2018. Outpatient and primary care data were not integrated electronically at the time of the study. Our ED is large and is one of the busiest in Europe, with approximately 1000 daily attendances in early-2023. Around one-fifth of attendees are aged over 65 [7].
Available data included demographics, vital signs, and diagnoses as ICD-10 codes. All data were extracted from the EPR using automated export by a data manager who was not involved in study analyses. The observation period was selected to mitigate for a plausible effect on attendance patterns and mortality data during the Covid-19 pandemic. In a deviation from the online protocol, only data for people aged over 64 were analysed due to electronic archiving restrictions at the time of access [8]. Data linkage and analyses were performed using R with caret, comorbidity, ggplot2, HFRS, pROC, and survival packages [9]. The study protocol was approved by the University of Leicester’s research ethics committee (ref 33749) and the UK Health Research Authority (ref 313451). Reporting followed the STROBE guidelines [10].
Dataset preparation
Data were filtered so that each individual’s first emergency care attendance in year 2019 (excluding Eye Casualty presentations) was taken as their ‘index’ episode. Index episodes were linked to the person’s immediate prior ‘reference’ episode. Eligible reference episodes were hospital admissions which lasted more than seventy-two hours, had admission date within the previous eighteen months (the EPR implementation period) and ended with discharge more than fourteen days before the index attendance.
The mean values for vital signs observed over the final forty-eight hours of reference episodes were considered to represent ‘baseline’ values, as in this period people would have been usually well enough to go home having reached more stable health. Frailty assessments used the Clinical Frailty Score (CFS), and due to data missingness the Hospital Frailty Risk Score (HFRS) was computer-calculated for all patients from ICD-10 codes at reference discharge [11, 12]. The Charlson Comorbidity Index (CCI) was also computer-calculated from ICD-10 codes.
Relative systolic, diastolic, and pulse values were each calculated by subtracting the baseline reference observations from the first index emergency care value. The final dataset therefore linked demographics, vital signs, and outcomes between people’s index ED attendance and immediate prior reference inpatient discharge.
Statistical analyses
Feasibility of comparison with baseline data
The proportion was reported for ED attendances with linkable hospital vital signs data within the previous eighteen months.
External validation of the 7 mmHg relative hypotension threshold
Summary statistics were presented for age, frailty, comorbidity, episode characteristics including vital signs, and mortality outcome for emergency care attendees with eligible reference episodes. Cases of relative hypotension were identified as negative relative systolic values exceeding 7 mmHg. 30-day mortality and survival frequencies were subclassified by presence of relative hypotension and clinical variables.
Continuous data for age, HFRS, and vital signs were assessed for normality using visual inspection of density plots and Shapiro–Wilk tests. Age, frailty, and relative hypotension were then examined for interaction using the Kruskal Wallis test. Cox regression analysis assessed for association between relative hypotension (7 mmHg threshold) and mean time to mortality censored at 30 days, adjusting for age, sex, frailty, and comorbidity.
Refining the threshold for clinically important relative hypotension and developing a risk tool
Receiver operating characteristic (ROC) curve analysis assessed relative systolic pressure as a predictor of binary 30-day mortality. Area under the curve, sensitivity, and specificity values were determined. The relative hypotension threshold maximising sensitivity and specificity was determined by the Youden Index.
Logistic regression models were used to examine the effect of relative hypotension on binary 30-day mortality, developing a risk tool using forward selection of parameters including age, sex, HFRS, CCI, ethnicity, interaction terms for vital signs and comorbidity, and k-fold internal cross validation (k = 10). Next, relative systolic change was added to the NEWS2 model to assess for improved performance. The ROC curves for the new risk tool and for NEWS2 plus relative systolic pressure were compared with NEWS2 alone.
Results
Dataset description and feasibility of comparison
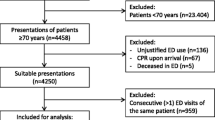
In 2019 our ED was attended 50,860 times by 32,548 people aged over 64 years, and their first attendances were selected for analyses (Fig. 2). 5136 (16%) index ED attendances had eligible reference hospital episodes for data linkage. These individuals’ characteristics are summarized in Table 1. 3318 (65%) people had died by the time of analysis in 2022 [median 318 (IQR 587) days from ED attendance], and 534 died within 30 days. Nearly half (44.8%) of individuals had missing data for CFS. Where CFS was recorded, those who died within 30 days had higher proportion of frailty (52%) than those who survived (36%). Calculated for the whole cohort, the HFRS was similar between people who died and survived [5.7 (IQR 7.8) vs 5.4 (IQR 8.5), median difference: − 0.4; 95% CI − 0.8 to 0].
External validation of the 7 mmHg relative hypotension threshold
People with 30-day mortality had higher frequency of relative hypotension (> 7 mmHg) than those who survived (43.6% vs 26.5%; OR 2.15; 95% CI 1.78–2.59). Frequencies were similar across subclassifications of age, CFS, HFRS, CCI, and index vital signs (Table 2). CFS was omitted from the subsequent analyses due to the extent of missing data; HFRS was used as the frailty measure.
In univariate Cox regression models (Table 3), relative hypotension exceeding 7 mmHg below baseline was associated with 107% increased risk (HR 2.07; 95% CI 1.74–2.45) of mortality (censored at 30 days) compared to relative hypotension ≤ 7 mmHg or relative hypertension. This was also the case in the multivariate model, where there appeared to be 98% increased risk (HR 1.98; 95% CI 1.66–2.45) of mortality within 30 days for individuals with relative hypotension exceeding 7 mmHg below baseline, having adjusted for age, HFRS, CCI, and sex. Mortality risk was also higher for people with higher CCI (HR 1.20; 95% CI 1.13–1.28) and male sex (HR 1.23; 95% CI 1.04–1.45), whereas there was no strong association with age (HR 1.03; 95% CI 1.02–1.04) or HFRS (HR 1.00; 95% CI 0.99–1.02). The survival curves for the multivariate Cox model are shown in Fig. 3, demonstrating poorer survival probability for individuals with relative hypotension exceeding 7 mmHg having adjusted for age, HFRS, CCI, and sex.
Refining the threshold for clinically important relative hypotension and developing a risk tool
A logistic regression model for 30-day mortality and relative systolic pressure (AUC: 0.62; k-fold SDAUC: 0.03) yielded a surprisingly small 1.81 mmHg (lower than baseline) threshold at the point of maximised sensitivity (0.52; 95% CI 0.48–0.57) and specificity (0.67; 95% CI 0.66–0.68). Using this threshold, 1095 of 4366 individuals with apparently normal ED systolic pressure (> 111 mmHg [13]) had relative hypotension from baseline, and their mortality was higher (11.1% vs 7.5%). These people were very slightly older (mean 81.3 vs 80.8) and had slightly higher HFRS (mean 7.24 vs 6.68). Similarly, among 3372 people with reassuring ED NEWS2 (< 3), 946 had relative hypotension and their mortality was 7.9% vs 4.4%.
The final risk tool adjusted for all predictors with evidence for significance in univariate models. Greater relative systolic decrease, pulse increase, comorbidity index, age, and male sex were all significant predictors for 30-day mortality (Table 4). AUC for this adjusted risk tool was 0.69 (k-fold SDAUC: 0.05). The NEWS2 composite score alone had better predictive performance (AUC: 0.73; k-fold SDAUC: 0.05), while adding relative systolic change to the NEWS2 conferred marginal further improvement (AUC: 0.74; k-fold SDAUC: 0.03). Model characteristics for the ROC curves (Fig. 4) are presented in Table 5.
Limitations
This study used retrospective hospital data from a single centre. Only people aged over 64 were included in the analysis due to archiving, restricting the data accessible for research. The feasibility of comparison with baseline data may be overestimated, with younger people typically having fewer hospital admissions. Furthermore, people with previous hospital admissions are more likely to live with frailty or chronic illness, and therefore interpretation of relative hypotension in primary care or outpatient settings should be with caution. The risk tool presented and the integration of relative systolic with NEWS2 warrant further research with other cohorts.
Data for CFS were missing in approximately half of this sample, despite the scale being in routine use here [14]. Further work is needed to examine the patterns and significance of this missingness. Our analyses therefore instead used the HFRS calculated for all individuals. The CFS considers the phenotypic manifestations of frailty on function and dependence, while the HFRS considers the sensitive diagnoses contributing to frailty-related risks. Elsewhere, these measures have both been shown to predict adverse health outcomes but are only weakly correlated, meaning they may identify different populations who are at risk [15, 16].
Our final model found the Charlson comorbidity index to be associated with 30-day mortality. We did not examine the contributing diagnoses in closer detail, and we did not have access to prescribing data for the included individuals. Investigation of subgroups with specific conditions (such as hypertension) is warranted to better understand this relationship.
We compared models only for the outcome of death within 30 days. Our system lacks routine collection of more person-centred outcomes, which are likely to be more meaningful especially for those living with frailty [17]. Future work might examine relationships between physiological data and person-centred outcomes from healthcare.
Discussion
Using data routinely available to clinicians, we were able to compare 16% older ED attendees’ vital signs to their recent baseline EPR data for hospital episodes. Systems with more established EPR systems might consider longer reference periods, and as technology evolves it may become possible to ‘pull’ primary care vital signs into the hospital EPR for comparison. Furthermore, such integrations and the increasing use of hospital electronic prescribing may enable future consideration of pharmacological contributors to impaired autoregulation. Our initial analysis provided external validity for increased mortality risk when relative systolic pressure exceeds 7 mmHg below baseline, as observed by Candel et al. previously [6].
To refine this threshold using a risk tool, we considered relative systolic pressure as a continuous variable and observed a surprisingly small 1.81 mmHg (lower than baseline). Test characteristics were poor for sensitivity and specificity, and this threshold is not measurable in practice due to device precision, variation, and calibration. Our data did not report the method for each blood pressure measurement, but we expect the majority to have used automatic cuffs with digital displays. It appeared, then, that in effect any relative hypotension could confer mortality risk.
In our sample, the unaltered NEWS2 had similar performance for 30-day mortality prediction to previous research observing older people living with frailty [3]. Incorporating relative systolic change into a NEWS2 model marginally improved predictive performance for 30-day mortality. This yielded the best-performing AUC in this study, which at only 0.74 prompts for consideration on the limitations of risk stratification scores compared with ED clinician judgement, especially when applied to older people living with frailty [5, 18].
Theories for the mortality effect of relative hypotension
We had sought to determine whether systolic pressure lower than baseline was associated with mortality, having based our theory on knowledge of hypotension causing poor outcomes. However, re-examination of Table 1 presents an alternative hypothesis. People who died had slightly lower ED systolic pressure than baseline value (mean 123 mmHg vs 127 mmHg), while survivors had relatively higher systolic pressure than their previous baseline (mean 138 mmHg vs 129 mmHg). We postulate that the mechanism underlying our small observed ‘relative hypotension’ threshold was not the relative decrease in these individuals’ systolic pressure, but rather their absence of autoregulatory relative hypertension during illness [19]. Future work might therefore consider risks for people with blood pressure at or below previous discharge values. We assumed that these discharge values represented individuals’ ‘normal’ baseline pressure, but with strict inpatient medications concordance and dynamic physiology during illness recovery this may not have been the case; further work observing hospital discharge and subsequent vital signs in primary care is warranted.
In older people, both high and low blood pressures are associated with poorer outcomes in a range of clinical situations [20,21,22]. Older people are more likely to experience chronic hypertension, with resulting small vessel disease, arterial stiffness, and reduced arterial compliance [19, 23]. As a result, the brain may become chronically adapted to higher resting perfusion pressures, and may be more vulnerable to acute episodes of hypotension due to a rightward shift in the cerebral autoregulation curve [23, 24]. Cerebral autoregulation is the intrinsic property of the brain to regulate its own blood supply, buffering falls and rises in systemic blood pressure, maintaining oxygen delivery and preventing pressure surges [25]. Therefore, moderately elevated blood pressure during acute illness may confer a protective effect by maintaining consistent cerebral perfusion, and not breaching the lower or upper limits of cerebral autoregulation. However, larger rises in blood pressure may also be detrimental, as with ageing the blood vessels become more fragile, and the risk of cerebral haemorrhage is higher [19].
Observed individuals who survived and died were similar in age and had only slight differences in HFRS and Charlson comorbidity scores. Consistent with previous research, those with higher CFS had poorer 30-day mortality although the degree of missing data was substantial [7]. Further examination for differences between these groups is warranted in order to explain this absence of relative hypertension. In particular, this might consider not only the diagnoses contributing to underlying comorbidity but also individual medications and polypharmacy [26]. The presenting issue and ED diagnosis are also candidates for investigation, with sepsis and trauma plausibly disrupting homeostatic mechanisms for blood pressure compensation [27].
Conclusions
In this single-centre study, relative change in vital signs was calculated using routine electronic patient records for a modest proportion of ED attendees. Independent external validation was demonstrated for the association between relative systolic decrease exceeding 7 mmHg from baseline and increased mortality within 30 days. An adjusted risk tool in effect showed any relative hypotension to confer increased mortality risk. These findings have restricted context to those older people with previous hospital admissions, and should be interpreted with caution in other settings. Further investigation is needed to identify differences within comorbidity subgroups.
Data availability
The dataset generated and analysed during the current study are not publicly available due to the ethical approvals granted but are available from the corresponding author on reasonable request.
References
Candel BGJ et al (2022) The association between vital signs and clinical outcomes in emergency department patients of different age categories. Emerg Med J 39(12):903–911
Nissen SK et al (2021) The impact of age on predictive performance of national early warning score at arrival to emergency departments: development and external validation. Ann Emerg Med 79:354–363
Kemp K et al (2020) National Early Warning Score 2 (NEWS2) and 3-level triage scale as risk predictors in frail older adults in the emergency department. BMC Emerg Med 20(1):83
Warmerdam M et al (2018) The association between systolic blood pressure and in-hospital mortality in older emergency department patients who are hospitalised with a suspected infection. Emerg Med J 35(10):619
Vardy ERLC et al (2022) NEWS2 and the older person. Clin Med 22(6):522
Candel BGJ et al (2022) The difference between the patients' initial and previously measured systolic blood pressure as predictor of mortality in older emergency department patients. Eur Geriatr Med 13(2):59–365
Elliott A et al (2021) Does the clinical frailty scale at triage predict outcomes from emergency care for older people? Ann Emerg Med 77(6):620–627
van Oppen JD et al (2022) Relative hypotension in emergency care. protocols.io. https://doi.org/10.17504/protocols.io.14egn2876g5d/v1
R Core Team (2022) R: a language and environment for statistical computing. R Foundation for Statistical Computing: Vienna
von Elm E et al (2008) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–349
Rockwood K et al (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ 173(5):489–495
Gilbert T et al (2018) Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet 391(10132):1775–1782
Royal College of Physicians (2017) National Early Warning Score (NEWS) 2: Standardising the assessment of acute-illness severity in the NHS. https://www.rcplondon.ac.uk/projects/outputs/national-early-warning-score-news-2. Accessed 10 Feb 2022
Aijaz F, Conroy S, Banerjee J (2018) Embedding the clinical frailty scale in the emergency department and its impact on patient care. Age Ageing 47:iii20–iii23
Subramaniam A et al (2022) Comparison of the predictive ability of clinical frailty scale and hospital frailty risk score to determine long-term survival in critically ill patients: a multicentre retrospective cohort study. Crit Care 26(1):121
Alshibani A et al (2022) A comparison between the clinical frailty scale and the hospital frailty risk score to risk stratify older people with emergency care needs. BMC Emerg Med 22(1):171
van Oppen JD et al (2022) What matters most in acute care: an interview study with older people living with frailty. BMC Geriatr 22:156
Veldhuis LI et al (2022) Performance of early warning and risk stratification scores versus clinical judgement in the acute setting: a systematic review. Emerg Med J 39(12):918
Beishon L et al (2021) Vascular and haemodynamic issues of brain ageing. Pflugers Arch 473(5):735–751
Peters R et al (2018) Orthostatic hypotension and symptomatic subclinical orthostatic hypotension increase risk of cognitive impairment: an integrated evidence review and analysis of a large older adult hypertensive cohort. Eur Heart J 39(33):3135–3143
Kang YY, Wang JG (2016) The J-curve phenomenon in hypertension. Pulse (Basel) 4(1):49–60
Appleton JP, Sprigg N, Bath PM (2016) Blood pressure management in acute stroke. Stroke Vasc Neurol 1(2):72–82
van Beek AH et al (2008) Cerebral autoregulation: an overview of current concepts and methodology with special focus on the elderly. J Cereb Blood Flow Metab 28(6):1071–1085
Beishon L, Haunton VJ, Panerai RB (2022) Antihypertensives in dementia: good or bad for the brain? J Cereb Blood Flow Metab 43:1800–1802
Panerai RB (1998) Assessment of cerebral pressure autoregulation in humans—a review of measurement methods. Physiol Meas 19(3):305–338
Prybys KM, Melville KA, Hannah JR (2002) Polypharmacy in the elderly: clinical challenges in emergency practice: part 1. Emerg Med Rep 23(11):145–153
Carrara M et al (2021) The autonomic nervous system in septic shock and its role as a future therapeutic target: a narrative review. Ann Intensive Care 11(1):80
Funding
Statistical analyses were conducted with funding from the Royal College of Emergency Medicine. Three authors received National Institute for Health and Care Research (NIHR) grants: Doctoral Research Fellowship (JvO), Academic Clinical Lectureship (LB), Senior Investigator (TC). RKO is supported by the Academy of Medical Sciences/the Wellcome Trust/ the Government Department of Business, Energy and Industrial Strategy/the British Heart Foundation/Diabetes UK Springboard Award (SBF006\1122).
Author information
Authors and Affiliations
Contributions
JvO and LB conceptualised the study. JvO, RKO, LB, and TC prepared the protocol and obtained regulatory approvals. WJ prepared the dataset. JvO linked and analysed the data under supervision by RKO. All authors contributed to manuscript drafting and revision. JvO takes responsibility for the work overall.
Corresponding author
Ethics declarations
Conflict of interest
RKO is a member of the National Institute for Health and Care Excellence (NICE) Technology Appraisal Committee, member of the NICE Decision Support Unit (DSU), and associate member of the NICE Technical Support Unit (TSU). She has served as a paid consultant to the pharmaceutical industry, providing unrelated methodological advice. She reports teaching fees from the Association of British Pharmaceutical Industry (ABPI) and the University of Bristol.
Ethical approval
The study protocol was approved by the University of Leicester’s research ethics committee (ref 33749) and the UK Health Research Authority (ref 313451). Individual informed consent was not applicable as the study used anonymised data.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Oppen, J.D., Owen, R.K., Jones, W. et al. The effect of relative hypotension on 30-day mortality in older people receiving emergency care. Intern Emerg Med 19, 787–795 (2024). https://doi.org/10.1007/s11739-023-03468-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-023-03468-5