Abstract
SARS-CoV2-induced direct cytopathic effects against type II pneumocytes are suspected to play a role in mediating and perpetuating lung damage. The aim of this study was to evaluate serum KL-6 behavior in COVID-19 patients to investigate its potential role in predicting clinical course. Sixty patients (median age IQR, 65 (52–69), 43 males), hospitalized for COVID-19 at Siena COVID Unit University Hospital, were prospectively enrolled. Twenty-six patients were selected (median age IQR, 63 (55–71), 16 males); all of them underwent follow-up evaluations, including clinical, radiological, functional, and serum KL-6 assessments, after 6 (t1) and 9 (t2) months from hospital discharge. At t0, KL-6 concentrations were significantly higher than those at t1 (760 (311–1218) vs. 309 (210–408) p = 0.0208) and t2 (760 (311–1218) vs 324 (279–458), p = 0.0365). At t0, KL-6 concentrations were increased in patients with fibrotic lung alterations than in non-fibrotic group (755 (370–1023) vs. 305 (225–608), p = 0.0225). Area under the receiver operating curve (AUROC) analysis showed that basal KL-6 levels showed good accuracy in discriminating patients with fibrotic sequelae radiologically documented (AUC 85%, p = 0.0404). KL-6 concentrations in patients with fibrotic involvement were significantly reduced at t1 (755 (370–1023) vs. 290 (197–521), p = 0.0366) and t2 (755 (370–1023) vs. 318 (173–435), p = 0.0490). Serum concentrations of KL-6 in hospitalized COVID-19 patients may contribute to identify severe patients requiring mechanical ventilation and to predict those who will develop pulmonary fibrotic sequelae in the follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Krebs von den Lungen-6 (KL-6) is a serum high molecular weight glycoprotein, increased in many interstitial lung diseases (ILDs), including idiopathic pulmonary fibrosis and hypersensitivity pneumonitis [1,2,3]. It is mainly produced by damaged or regenerating alveolar type II pneumocytes and its serum concentrations are regarded as biomarker of lung epithelial damage (reff). The prognostic value of peripheral KL-6 in ILD has been validated as well as its promising value in predicting the response to antifibrotic therapies [4, 5]. Moreover, KL-6 has been also proposed as bioindicator of acute respiratory distress syndrome (ARDS) and infective pneumonia (ref). Since the outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, KL-6 has also been proposed as a prognostic marker for this disease [6,7,8,9]. The pathogenesis of COVID-19 (as the lung disease caused by SARS-CoV-2 is defined) is not entirely clear [10], although it is postulated that elevated serum concentrations of proinflammatory cytokines and oxidative stress mediators contribute to lung injury, facilitating the onset of an acute respiratory syndrome (similar to ARDS) [11]. Host susceptibility and virus-induced direct cytopathic effects against type I and II pneumocytes are suspected to play a crucial role in mediating and perpetuating lung damage [12,13,14].
Our research group first reported elevated serum concentrations of KL-6 in critical COVID-19 patients and our results were soon confirmed by two other papers [8, 9]. However, no data are currently available on KL-6 role in the follow-up of COVID-19 patients or its potential predictive value for fibrotic lung alteration development.
The aim of this study was to evaluate serum KL-6 behavior in a population of COVID-19 hospitalized patients along the 9-month follow-up of our Centre, to investigate its potential role in predicting clinical course of disease.
Materials and methods
Study population
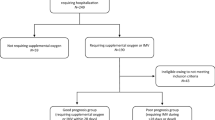
Sixty patients (median IQR, 65 (52–69), 43 males), all hospitalized for COVID-19 at Siena COVID Unit University Hospital, were prospectively enrolled. Fifteen of these patients need intensive care unit (ICU) and mechanical ventilation. Our sixty patients underwent serum sampling specifically for KL-6 assessment on admission (t0). Patients who did not give informed consent to the study or who had a previous diagnosis of interstitial lung disease or chronic obstructive pulmonary disease were excluded.
After 6 (t1) and 9 (t2) months from hospital discharge, twenty-six patients (median age (IQR) 63 (55–71) years, 16 males) underwent follow-up evaluations including physical examination, lung function tests, diffusing capacity of the lung for carbon monoxide (DLCO), blood gas analysis and high-resolution computed tomography (HRCT) of the chest. CT features (fibrotic interstitial lung abnormalities, ground-glass opacities, and air-trapping) were evaluated by on-site radiologists, experienced in interstitial lung diseases. All patients gave their written informed consent to the study for clinical data collection. The study was approved by our local ethics committee (C.E.A.V.S.E Markerlung 17,431).
KL-6 assay
Serum samples were obtained from all patients on admission, before any biological treatment or intravenous infusion of high-dose steroids or invasive ventilation, and from 26 patients at follow-up, 6 and 9 months after discharge from hospital. Serum concentrations of Krebs von den Lungen-6 were measured by KL-6 reagent assay (Fujirebio Europe, UK), as previously reported [2, 3, 9, 15, 16]. The principle of the assay is agglutination of sialylated carbohydrate antigen with KL-6 mAb by antigen–antibody reaction. The change in absorbance was measured to determine serum concentrations of KL-6, which were expressed in U/ml. A cut-off value of 465 U/ml was applied, as previously reported [17].
Lung function tests
Lung function tests were performed according to ATS/ERS standards [18] using a Jaeger body plethysmograph with corrections for temperature and barometric pressure. Forced expiratory volume in the first second (FEV1), forced vital capacity (FVC) and diffusing capacity of the lung for carbon monoxide (DLCO) were recorded.
Statistical analysis
The data did not show a normal distribution. Results were reported as median (IQR), unless otherwise stated. One-way ANOVA nonparametric test (Kruskal–Wallis test) and Dunn’s post test were used for multiple comparisons. The Mann–Whitney test was used to compare pairs of variables. Wilcoxon matched pairs signed rank test was used to compare variables of the same patient at t0 and t1. The Chi-squared test was used for categorical variables as appropriate. Statistical analysis and graphic representation of the data were performed with GraphPad Prism 8.0 software.
Results
Table 1 shows the main characteristics of our COVID-19 population at t0 (hospital admission). Serum concentrations of KL-6, PFT and blood gas analysis parameters were collected (Table1).
At each sampling time, the study population did not differ significantly in terms of sex, age or comorbidities, whereas serum KL-6 concentrations were higher at hospitalization (t0) than at t1 (760 (311–1218) vs 309 (210–408) p = 0.0208) and t2 (760 (311–1218) vs 324 (279–458), p = 0.0365). About PFT parameters, we did not collect these data at t0 in hospitalized patients affected by COVID19.
According to CT radiological features, patients were classified according to the evidence of fibrotic lung alterations (including ground-glass opacities, linear thickening, or organizing pneumonia areas).
At t0, KL-6 serum concentrations were significantly increased in fibrotic (n = 14) than non-fibrotic (n = 12) group (755 (370–1023) vs 305 (225–608), p = 0.0225) (Fig. 1). Area under the receiver operating curve (AUROC) analysis showed that basal KL-6 had good accuracy in discriminating patients with HRCT evidence of fibrotic interstitial lung abnormalities (AUC = 85%, Std. Error 0.1080, 95%CI 64–100, p = 0.0404) (Fig. 2). The best cut-off value for KL-6 concentrations was 455U/ml (75% sensitivity and 80% specificity). At t1 and t2, no differences of demographic features, blood gas analysis values, and PFT parameters were observed between the two groups (data available). KL-6 concentrations in fibrotic group significantly reduced at t1 (755 (370–1023) vs 290 (197–521), p = 0.0366) and t2 (755 (370–1023) vs 318 (173–435), p = 0.0490) (Table 2). Interestingly, three patients maintained very high KL-6 concentrations after 6 and 9 months of follow-up (median IQR, t0: 1006 (1000–1011); t1: 595 (570–1799); t2: 527 (498–1373)), showing simultaneous HRCT evidence of interstitial lung involvement (Fig. 1S). Patients with no fibrotic lung sequelae at HRCT of the chest showed normal KL-6 concentrations at follow-up.
Concerning respiratory function, no significant differences in FVC and/or DLCO percentages were found between patients with and without fibrotic lung alterations at CT scan.
Discussion
This report first described KL-6 peripheral concentrations in a population of COVID-19 patients after 6 and 9 months from hospitalization discharge together with radiological and functional parameters. Serum concentrations of KL-6 at hospital admission were reported to be significantly increased in severe patients admitted to intensive care unit and requiring intubation with mechanical ventilation, but not in mild-moderate patients with less severe respiratory impairment [9]. This mucin protein has been widely studied in idiopathic pulmonary fibrosis and ARDS patients, but limited data are available on its prognostic potential in infectious viral pneumonia [11,12,13]. Our interest aroused from the observation that KL-6 was associated with prognosis in ILD and ARDS, reflecting type I and type II alveolar pneumocyte damage. SARS-CoV-2 is known to have specific tropism for alveolar epithelial cells, causing interstitial lung damage, epithelial lung alterations, and regenerative processes, mainly in the acute phase [9]. A significant increase in serum concentrations of KL-6 was demonstrated in patients critically ill with COVID-19 [8, 9] and was further confirmed in our study.
Interestingly, our results demonstrated for the first time a normalization of serum concentrations of KL-6 (< 465U/ml) 6 and 9 months after discharge from hospital. Lung damage due to COVID-19 seemed not to be necessarily progressive, unlike in idiopathic pulmonary fibrosis, where KL-6 tends to increase with IPF progression [1, 4, 5]. Moreover, in the majority of patients with fibrotic sequelae, the decrease and substantial normalization of serum KL-6 concentrations may reflect the amelioration of the clinical status, suggesting that fibrotic interstitial lung abnormalities related to COVID-19 are not associated with persistent active epithelial damage and consequent aberrant fibrogenesis. On the contrary, those patients who developed severe persistent fibrotic lung sequelae at HRCT showed persistent high levels of KL-6 in the follow-up, implicating that this biomarker may be useful in the mid-long-term management of these patients. However, these data will be further evaluated in a longer follow-up to be confirmed. Moreover, in our population, lung volumes were almost preserved at follow-up as well as DLCO percentages, differently from a recent follow-up study reporting functional alterations in more than 25% of patients, albeit after a shorter follow-up of 3 months [19], and this aspect may surely influence the heterogeneity of our population.
Thus, this study contributes to the definition of the natural course of COVID-19 as the normalization of peripheral KL-6 concentrations, recorded 6 and 9 months after the acute phase of SARS-CoV-2 infection, suggesting a non-progressive fibrotic lung involvement in the majority of patients.
Serum concentrations of KL-6 seemed to reflect lung involvement in COVID-19 patients as reflected by HRCT features at 6-month follow-up.
In conclusion, increased serum concentrations of KL-6 in hospitalized COVID-19 patients may help to early discriminate severe patients requiring mechanical ventilation and predict those developing fibrotic lung sequelae in the follow-up.
Abbreviations
- KL-6:
-
Krebs von den Lungen-6
- ILDs:
-
Interstitial lung diseases
References
d’Alessandro M, Bergantini L, Cameli P, Vietri L, Lanzarone N, Alonzi V et al (2020) Krebs von den Lungen-6 as biomarker for disease severity assessment in interstitial lung disease: a comprehensive review. Biomark Med 68(6):414–421
Lanzarone N, Gentili F, Alonzi V, Bergantini L, d’Alessandro M, Rottoli P, et al. Bronchoalveolar lavage and serum KL-6 concentrations in chronic hypersensitivity pneumonitis: correlations with radiological and immunological features. Intern Emerg Med. 2020.
d’Alessandro M, Bergantini L, Cameli P, Lanzarone N, Antonietta Mazzei M, Alonzi V et al (2020) Serum KL-6 levels in pulmonary Langerhans’ cell histiocytosis. Eur J Clin Invest 20:e13242
Wakamatsu K, Nagata N, Kumazoe H, Oda K, Ishimoto H, Yoshimi M et al (2017) Prognostic value of serial serum KL-6 measurements in patients with idiopathic pulmonary fibrosis. Respir Investig 55(1):16–23
Bergantini L, Bargagli E, Cameli P, Cekorja B, Lanzarone N, Pianigiani L et al (2019) Serial KL-6 analysis in patients with idiopathic pulmonary fibrosis treated with nintedanib. Respir Investig 57(3):290–291
Awano N, Inomata M, Kuse N, Tone M, Takada K, Muto Y et al (2020) Serum KL-6 level is a useful biomarker for evaluating the severity of coronavirus disease 2019. Respir Investig 58(6):440–447
Xue M, Zheng P, Bian X, Huang Z, Huang H, Zeng Y et al (2020) Exploration and correlation analysis of changes in Krebs von den Lungen-6 levels in COVID-19 patients with different types in China. Biosci Trends 14(4):290–296
d’Alessandro M, Cameli P, Bergantini L, Franchi F, Scolletta S, Bargagli E. Serum concentrations of Krebs von den Lungen-6 in different COVID-19 phenotypes. J Med Virol. 2020.
d’Alessandro M, Cameli P, Refini RM, Bergantini L, Alonzi V, Lanzarone N et al (2020) Serum KL-6 concentrations as a novel biomarker of severe COVID-19. J Med Virol 92(10):2216–2220
D’alessandro M, Bennett D, Montagnani F, Cameli P, Perrone A, Bergantini L et al (2020) Peripheral lymphocyte subset monitoring in COVID19 patients: a prospective Italian real-life case series. Minerva Med. https://doi.org/10.23736/S0026-4806.20.06638-0
Sato H, Callister MEJ, Mumby S, Quinlan GJ, Welsh KI, duBois RM et al (2004) KL-6 levels are elevated in plasma from patients with acute respiratory distress syndrome. Eur Respir J 23(1):142–145
Nakamura H, Tateyama M, Tasato D, Haranaga S, Yara S, Higa F et al (2009) Clinical utility of serum beta-d-glucan and KL-6 levels in Pneumocystis jirovecii pneumonia. Intern Med Tokyo Jpn 48(4):195–202
Arai Y, Obinata K, Sato Y, Hisata K, Tadokoro R, Tawa T et al (2001) Clinical significance of the serum surfactant protein D and KL-6 levels in patients with measles complicated by interstitial pneumonia. Eur J Pediatr 160(7):425–429
Kawasaki Y, Aoyagi Y, Abe Y, Go H, Imamura T, Kaneko M et al (2009) Serum KL-6 levels as a biomarker of lung injury in respiratory syncytial virus bronchiolitis. J Med Virol 81(12):2104–2108
d’Alessandro M, Carleo A, Cameli P, Bergantini L, Perrone A, Vietri L et al (2020) BAL biomarkers’ panel for differential diagnosis of interstitial lung diseases. Clin Exp Med 20(2):207–216
d’Alessandro M, Perillo F, Metella Refini R, Bergantini L, Bellisai F, Selvi E et al (2020) Efficacy of baricitinib in treating rheumatoid arthritis: modulatory effects on fibrotic and inflammatory biomarkers in a real-life setting. Int Immunopharmacol 86:106748
Ohnishi H, Yokoyama A, Kondo K, Hamada H, Abe M, Nishimura K et al (2002) Comparative study of KL-6, surfactant protein-A, surfactant protein-D, and monocyte chemoattractant protein-1 as serum markers for interstitial lung diseases. Am J Respir Crit Care Med 165(3):378–381
Culver BH, Graham BL, Coates AL, Wanger J, Berry CE, Clarke PK et al (2017) Recommendations for a standardized pulmonary function report an official American thoracic society technical statement. Am J Respir Crit Care Med. 196(11):1463–1472
Zhu C, Zhao YB, Kong LF, Li ZH, Kang J (2016) The expression and clinical role of KL-6 in serum and BALF of patients with different diffuse interstitial lung diseases. Zhonghua Jie He He Hu Xi Za Zhi Zhonghua Jiehe He Huxi Zazhi Chin J Tuberc Respir Dis 39(2):93–97
Funding
Open Access funding provided by Università degli Studi di Siena. The study was performed at Siena University without funding or sponsors.
Author information
Authors and Affiliations
Consortia
Contributions
MD, LB, PC, and EB conceived the study and supervised all aspects. MD, PC, GC, LR, FB, and MAM collected data and built the database. MD, PC, LB, EB, and MAM oversaw data analysis and interpretation of results. All authors drafted and revised the paper.
Corresponding author
Ethics declarations
Conflict of interest
All the authors have no conflicts of interest to declare.
Statement of human and animal rights
The research was approved by the local ethics committee (MARKERLUNG n° 17431, C.E.A.V.S.E n° 18712).
Informed consent
All subjects gave their written informed consent to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
d’Alessandro, M., Bergantini, L., Cameli, P. et al. Serial KL-6 measurements in COVID-19 patients. Intern Emerg Med 16, 1541–1545 (2021). https://doi.org/10.1007/s11739-020-02614-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-020-02614-7