Abstract
Acute exacerbation (AE) significantly affects the prognosis of patients with interstitial lung disease (ILD). This study aimed to investigate the best prognostic biomarker for patients with AE-ILD. Clinical data obtained during hospitalization were retrospectively analyzed for 96 patients with AE-ILD at three tertiary hospitals. The mean age of all subjects was 70.1 years; the percentage of males was 66.7%. Idiopathic pulmonary fibrosis accounted for 60.4% of the cases. During follow-up (median: 88 days), in-hospital mortality was 24%. Non-survivors had higher lactate dehydrogenase and C-reactive protein (CRP) levels, lower ratio of partial pressure of oxygen to the fraction of inspiratory oxygen (P/F ratio), and higher relative change in Krebs von den Lungen-6 (KL-6) levels over 1 week after hospitalization than survivors. In multivariable analysis adjusted by age, the 1-week change in KL-6—along with baseline P/F ratio and CRP levels—was an independent prognostic factor for in-hospital mortality (odds ratio 1.094, P = 0.025). Patients with remarkable increase in KL-6 (≥ 10%) showed significantly worse survival (in-hospital mortality: 63.2 vs. 6.1%) than those without. In addition to baseline CRP and P/F ratio, the relative changes in KL-6 over 1 week after hospitalization might be useful for predicting in-hospital mortality in patients with AE-ILD.
Similar content being viewed by others
Introduction
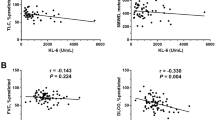
Interstitial lung disease (ILD) is a heterogeneous group of disorders characterized by inflammation and/or fibrosis involving pulmonary interstitium1,2. The clinical course of ILD is highly variable, and acute exacerbation (AE) is a fatal complication with high mortality3. The annual incidence of AE-ILD varies in the range of 4–15% according to the type of ILD or study population4,5,6. Based on previous studies, in-hospital mortality was up to 50% and no significant difference in in-hospital mortality was found between idiopathic pulmonary fibrosis (IPF) and non-IPF ILD4,5,7. Previous studies revealed several predicting factors for mortality in patients with AE-ILD; low baseline forced vital capacity (FVC) and diffusion of carbon monoxide (DLco) before AE, extensive ground-glass opacity or consolidation on high-resolution computed tomography (HRCT), impaired oxygenation, high lactate dehydrogenase (LDH) and C-reactive protein (CRP) levels, and low percentages of lymphocytes on bronchoalveolar lavage (BAL) fluid at the time of hospitalization were associated with poor prognosis of patients with AE-ILD4,8,9,10.
In contrast to the pulmonary function test, HRCT, or BAL fluid analysis, blood biomarkers are relatively easy to test independent of patient effort or reader ability and can be measured less invasively11. Krebs von den Lungen-6 (KL-6) is a mucin-like glycoprotein produced by type 2 alveolar epithelial cells that is released into the bloodstream through the damaged alveolar basement membrane when type 2 alveolar epithelial cells are injured and proliferated12,13. Recently, some studies have revealed that baseline KL-6 levels at hospitalization are associated with mortality in AE-ILD8,14. KL-6 was also reported to be useful for predicting disease severity, clinical course, and prognosis of patients with ILD12,15,16. However, no studies have compared changes in blood biomarkers, including KL-6, in patients with AE-ILD and investigated their role in predicting the prognosis of patients with AE-ILD. Therefore, the aim of this study was to identify the best marker by comparing the usefulness of blood biomarkers for predicting the prognosis of patients with AE-ILD.
Methods
Study population
From March 2020 to December 2020, 160 patients with ILD, who were hospitalized due to AE at three tertiary hospitals in South Korea, were screened for enrolment in this study. Of the 160 patients, 8 patients who were hospitalized because of a second or multiple episode (s) of AE and 56 patients without blood KL-6 data during hospitalization were excluded. Finally, 96 patients with AE-ILD (58 at Asan Medical Center, 29 at Seoul National University Hospital, and 9 at Haeundae Paik Hospital) were included in this study (Fig. 1). ILD was diagnosed according to international guidelines1,2,17,18.
This study was approved by the Institutional Review Board of the Asan Medical Center (IRB No. 2021-0263), the Seoul National University Hospital (IRB No. H-2107-046-1233), and Haeundae Paik Hospital (IRB No. 2021-05-018) and conducted in accordance with the ethical standards of the Declaration of Helsinki. The requirement for written informed consent was waived owing to the retrospective nature of this study. All methods were performed in accordance with the relevant guidelines and regulations.
Data collection
Clinical and survival data for all patients during hospitalization were obtained from medical records and/or the National Health Insurance of Korea records. The results of pulmonary function test (PFT) and 6-min walk test (6MWT) within 3 months of hospitalization were also collected and considered baseline values. Spirometry was performed, and DLCO and total lung capacity (TLC) were measured according to the American Thoracic Society/European Respiratory Society recommendations19,20,21. The results are expressed as percentages of the normal predicted values. The BAL fluid analysis and 6MWT were performed in accordance with previously published guidelines22,23. Based on the criteria suggested by Collard et al., AE was defined as acute worsening of dyspnea typically within 30 days, with new bilateral lung infiltration that is not fully explained by heart failure or fluid overload and without any identified extra-parenchymal causes (pneumothorax, pleural effusion, or pulmonary embolism)5.
The Nanopia KL-6 assay (SEKISUI MEDICAL, Tokyo, Japan) was used to measure blood KL-6 levels. All samples were immediately transported and centrifuged after blood collection. The latex-enhanced immunoturbidimetric assay, which measures changes in absorbance by agglutination, was used to measure KL-6 concentration. CRP and LDH levels were measured using Cobas 8000 (ROCHE DIAGNOSTICS, Basel, Switzerland). The partial pressure of oxygen to the fraction of inspiratory oxygen ratio (P/F ratio) was calculated using the arterial blood gas analysis results obtained with pHOX Ultra (NOVA BIOMEDICAL, Waltham, MA, USA).
Statistical analysis
Continuous variables are expressed as mean ± standard deviation and were compared using an unpaired Student’s t-test. Categorical variables are presented as frequency and percentage and were compared using Chi-squared and Fisher’s exact tests. Absolute and relative changes in blood markers over 1 week from the baseline values were calculated as follows: absolute changes = measurement at follow-up − measurement at baseline; and relative changes = (measurement at follow-up − measurement at baseline)/measurement at baseline × 100 (%). Survival was analyzed using the Kaplan–Meier method, and the difference was assessed via a log-rank test. A logistic regression analysis was used to identify risk factors for in-hospital mortality in patients with AE. Variables with a P value of less than 0.1 in the unadjusted analysis were selected and adjusted by age for the multivariable analysis. Using the receiver operating characteristic (ROC) curve analysis, the best cut-off level of variables that predict in-hospital mortality was determined. A P value of less than 0.05 was considered significant. Statistical analyses were performed using IBM SPSS version 25.0 (IBM Corp., Armonk, NY, USA).
Results
Baseline characteristics
The mean age of the total patients was 70.1 years, the percentage of males was 66.7%, and 60.4% of patients had IPF (Table 1). Triggered and idiopathic AE were 32.3% and 67.7%, respectively. The baseline characteristics of patients were similar among the three hospitals, except for body mass index (Supplementary Table S1). During the follow-up period (median 88 days, interquartile range 24–176 days), 42 (43.8%) patients died after hospitalization; in-hospital mortality rate was 24.0% (n = 23). The 30-day and 90-day mortality rates were 21.6% and 36.1%, respectively. There was no difference in survival after hospitalization (the median survival: 134 days vs. not reached, P = 0.250) between patients with AE-IPF and those with AE-non IPF (Supplementary Figure S1). At the time of hospitalization, the non-survivors showed higher LDH and CRP levels and lower P/F ratio than the survivors (Table 1); however, there was no difference in baseline KL-6 levels and other clinical variables between the two groups. During hospitalization, almost all patients (99.0%) received steroid treatment (the median dose: 55.9 mg), and steroid pulse therapy and cytotoxic agents were provided in 45.8% and 12.5%, respectively (Table 2).
Changes in blood biomarkers
The absolute and relative changes in KL-6 levels over 1 week after hospitalization were significantly higher in non-survivors than in survivors (Table 3). However, there were no differences in the changes in LDH, CRP, and P/F ratio levels over 1 week between the two groups.
Risk factors for in-hospital mortality
In the unadjusted logistic regression analysis, CRP, P/F ratio, and relative changes in KL-6 levels over 1 week were identified as significant risk factors for the in-hospital mortality of patients with AE-ILD (Table 4). In the multivariable analysis adjusted by age, CRP, P/F ratio, and changes in KL-6 levels were also independent prognostic factors for in-hospital mortality. When classified according to the type of ILD, baseline LDH and relative changes in KL-6 levels over 1 week were significantly associated with in-hospital mortality in patients with AE-IPF in the unadjusted logistic regression analysis (Supplementary Table S2); however, baseline CRP and changes in CRP levels over 1 were significant prognostic factors in those with AE-non IPF (Supplementary Table S3).
In the ROC curve analysis, CRP, P/F ratio, and the relative changes in KL-6 levels over 1 week were useful for predicting in-hospital mortality; however, changes in KL-6 levels showed the highest area under the curve (AUC) values (0.902 [P < 0.001] vs. 0.818 [CRP, P < 0.001], 0.713 [P/F ratio, P = 0.005]) (Fig. 2 and Table 5). The best cut-off level for changes in KL-6 over 1 week for the prediction of in-hospital mortality was + 10% (sensitivity of 85.7% and specificity of 81.6%). The prediction models including CRP or P/F ratio, in addition to changes in KL-6 over 1 week, did not improve the performance of the models, including changes in KL-6 alone (Table 5). However, applying the two variables consecutively (from baseline variables to change in KL-6) was more useful for predicting in-hospital mortality (Supplementary Figure S2).
Comparison of the receiver operating characteristic curve of blood markers for predicting in-hospital mortality in patients with AE-ILD. AE-ILD acute exacerbation of interstitial lung disease; ROC curves: blue line, KL-6 relative change from baseline; red line, baseline P/F ratio; green line, baseline CRP. KL-6 Krebs von den Lungen-6, P/F ratio ratio of partial pressure of oxygen to the fraction of inspiratory oxygen, CRP C-reactive protein, AUC area under the curve.
Survival according to KL-6 levels
When all patients were divided into two groups according to the best cut-off level for the change in KL-6 over 1 week, patients with remarkable increase in KL-6 (more than 10% relative increase from baseline) showed significantly worse survival (in-hospital mortality: 63.2 vs. 6.1%; median survival: 42 vs. 142 days; P < 0.001) than those without (Fig. 3).
Comparison of survival curves after hospitalization between groups with high and low changes in KL-6 among patients with AE-ILD. Kaplan–Meier curves: blue line, high KL-6 change group; red line, low KL-6 change group. KL-6 Krebs von den Lungen-6, AE-ILD acute exacerbation of interstitial lung disease.
Discussion
To our knowledge, this is the first study to demonstrate the association between changes in blood biomarkers and the mortality of patients with AE-ILD during hospitalization. In addition to baseline CRP levels and P/F ratio, the change in KL-6 was identified as an independent prognostic factor for in-hospital mortality in ILD patients with AE. During hospitalization, a greater than 10% relative increase in KL-6 levels over 1 week could well differentiate poor prognosis among patients with AE-ILD.
In our study, a 10% relative change in KL-6 over 1 week was associated with poor prognosis of patients with AE-ILD. Previous studies also suggested the usefulness of the change in KL-6 for predicting prognosis of patients with ILD15,24. For 85 patients with ILD (IPF = 27, connective tissue disease [CTD]-ILD = 33, idiopathic NSIP = 18, and other idiopathic interstitial pneumonia = 7), Jiang et al. reported that a greater than 500 or 1000 U/mL increase in KL-6 within 1–6 months predicted disease progression (defined as death or decline in FVC > 10% or DLco ≥ 15% at 12 months) (odds ratio [OR] 1.73, 95% confidence interval [CI] 1.48–1.98, P < 0.01 and OR 2.57, 95% CI 2.26–2.88, P < 0.01, respectively) in the unadjusted logistic regression analysis15. Among 14 patients with rapidly progressive IPF (defined as deterioration of dyspnea within 2 months and the presence of ground glass opacity on HRCT), Yokoyama et al. found that, after corticosteroid pulse therapy, baseline KL-6 levels were significantly decreased at 1 or 3 weeks in survivors (− 18.9 ± 14.4%, P < 0.05 and − 32.7 ± 20.9%, P < 0.05, respectively), whereas KL-6 levels tended to increase at 3 weeks in non-survivors (+ 93.7 ± 103%; P < 0.05)24. These results indicate that a change in KL-6 level might be useful for predicting prognosis or treatment response. Moreover, unlike other biomarkers such as CRP and P/F ratio, KL-6 may more directly reflect the pathophysiology of AE-ILD characterized by diffuse alveolar damage12,13,25. For this reason, the change of KL-6 early in hospitalization could help to predict the prognosis of AE-ILD complementarily in addition to other biomarkers.
The baseline value of KL-6 was not associated with the prognosis of patients with IPF in our study. Contrary to our results, those of a previous study revealed the association between baseline KL-6 levels and prognosis of patients with AE-ILD8. For 58 patients with AE-IPF, Kishaba et al. demonstrated that high KL-6 levels at hospitalization were associated with increased risk of 90-day mortality (hazard ratio [HR] 2.909, P = 0.038) in the multivariable Cox analysis8. This contradicting result might be explained by the different clinical characteristics of the study population; our cohort had a higher P/F ratio (289.9 vs. 100–200) at hospitalization and more frequently used antifibrotic agents before AE (62.5% vs. 0%) than the cohort of the previous study8. Moreover, our cohort had a relatively lower mortality rate (in-hospital mortality: 24 vs. 56.9%; 3-month mortality rate: 36.1 vs. 70.7%) than the cohort of the previous report8. Antifibrotic agent can significantly reduce mortality after hospitalization in patients with IPF26; however, the previous study was not performed in the era of antifibrotic therapy8. Therefore, prolonged survival times in our study may reduce the predictive value of baseline KL-6 levels.
In our study, low baseline P/F ratio and high CRP levels were associated with poor prognosis of patients with AE-ILD. Previous studies have also reported similar results8,27. Through a multivariable Cox analysis, Kishaba et al. showed that a P/F ratio < 100 was associated with an increased risk of 3-month mortality (HR 2.42, P = 0.041) in patients with AE-IPF (n = 58)8. Cao et al. also revealed, through multivariable Cox analysis, that a lower P/F ratio at the time of hospitalization was associated with an increased risk of mortality (HR 0.989, 95% CI 0.984–0.994, P < 0.001) in patients with CTD-ILD (n = 70)27. Through unadjusted Cox analysis, Kamiya et al. reported that CRP levels at the onset of AE were associated with all-cause mortality (HR 1.05, 95% CI 1.02–1.08, P = 0.003) in 243 patients with AE-IPF28. Through multivariable logistic analysis, Song et al. also showed that CRP levels were associated with an increased risk of in-hospital mortality (OR 2.467, 95% CI 1.030–5.911, P = 0.043) and reduced P/F ratio (OR 0.989, 95% CI 0.983–0.996, P = 0.001) in patients with AE of IPF (n = 96)4. These results support our findings. However, unlike KL-6, the changes in CRP and P/F ratio could not predict prognosis. Thus, KL-6 was the only marker that could predict the prognosis of AE-ILD based on changes in its level over 1 week.
This study had some limitations. First, this study was of a retrospective nature and was conducted on Asian population, which may question the generalizability of our findings. Nonetheless, the baseline characteristics of patients in our study were found to be similar to those of patients in previous studies4,15,24. Second, only two time points (baseline and 1 week after hospitalization) were selected to evaluate the predictive role of the change in blood biomarkers. It was difficult to establish more time points during the follow-up owing to the high mortality rate of AE-ILD and the retrospective nature of this study. Nevertheless, the change in KL-6 over 1 week could well discriminate patients with poor prognosis. Third, patients with various ILDs, including IPF, were included in this study, resulting in a heterogenous distribution of diseases. However, the prognosis of AE of IPF and non-IPF ILD did not differ in a previous study7.
In conclusion, the relative change in KL-6 over 1 week was useful for predicting in-hospital mortality in patients with AE-ILD, in addition to baseline CRP and P/F ratio. Our data suggest that during hospitalization, a remarkable change in KL-6 level is useful for differentiating patients with poor prognosis among patients with AE-ILD.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Raghu, G. et al. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am. J. Respir. Crit. Care Med. 198, 44-e68 (2018).
Travis, W. D. et al. An Official American Thoracic Society/European Respiratory Society Statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am. J. Respir. Crit. Care Med. 188, 733–748 (2013).
Kim, D. S., Collard, H. R. & King, T. E. Jr. Classification and natural history of the idiopathic interstitial pneumonias. Proc. Am. Thorac. Soc. 3, 285–292 (2006).
Song, J. W., Hong, S. B., Lim, C. M., Koh, Y. & Kim, D. S. Acute exacerbation of idiopathic pulmonary fibrosis: Incidence, risk factors and outcome. Eur. Respir. J. 37, 356–363 (2011).
Collard, H. R. et al. Acute exacerbation of idiopathic pulmonary fibrosis. An International Working Group Report. Am. J. Respir. Crit. Care Med. 194, 265–275 (2016).
Park, I. N. et al. Acute exacerbation of interstitial pneumonia other than idiopathic pulmonary fibrosis. Chest 132, 214–220 (2007).
Moua, T. et al. Patients with fibrotic interstitial lung disease hospitalized for acute respiratory worsening: A large cohort analysis. Chest 149, 1205–1214 (2016).
Kishaba, T., Tamaki, H., Shimaoka, Y., Fukuyama, H. & Yamashiro, S. Staging of acute exacerbation in patients with idiopathic pulmonary fibrosis. Lung 192, 141–149 (2014).
Simon-Blancal, V. et al. Acute exacerbation of idiopathic pulmonary fibrosis: Outcome and prognostic factors. Respiration 83, 28–35 (2012).
Takei, R. et al. Impact of lymphocyte differential count > 15% in BALF on the mortality of patients with acute exacerbation of chronic fibrosing idiopathic interstitial pneumonia. BMC Pulm. Med. 17, 67 (2017).
Tzouvelekis, A., Kouliatsis, G., Anevlavis, S. & Bouros, D. Serum biomarkers in interstitial lung diseases. Respir. Res. 6, 78–78 (2005).
Ishikawa, N., Hattori, N., Yokoyama, A. & Kohno, N. Utility of KL-6/MUC1 in the clinical management of interstitial lung diseases. Respir. Investig. 50, 3–13 (2012).
Nobuoki, K. et al. New serum indicator of interstitial pneumonitis activity: Sialylated carbohydrate antigen KL-6. Chest 96, 68–73 (1989).
Ohshimo, S. et al. Baseline KL-6 predicts increased risk for acute exacerbation of idiopathic pulmonary fibrosis. Respir. Med. 108, 1031–1039 (2014).
Jiang, Y. et al. Sequential changes of serum KL-6 predict the progression of interstitial lung disease. J. Thorac. Dis. 10, 4705–4714 (2018).
Kim, H. C., Choi, K. H., Jacob, J. & Song, J. W. Prognostic role of blood KL-6 in rheumatoid arthritis–associated interstitial lung disease. PLoS One 15, e0229997 (2020).
Raghu, G. et al. Diagnosis of hypersensitivity pneumonitis in adults. An official ATS/JRS/ALAT clinical practice guideline. Am. J. Respir. Crit. Care Med. 202, e36–e69 (2020).
Park, S. W. et al. Korean guidelines for diagnosis and management of interstitial lung diseases: Part 1. Introduction. Tuberculosis Respir. Dis. 82, 269–276 (2019).
MacIntyre, N. et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur. Respir. J. 26, 720–735 (2005).
Miller, M. R. et al. Standardisation of spirometry. Eur. Respir. J. 26, 319–338 (2005).
Wanger, J. et al. Standardisation of the measurement of lung volumes. Eur. Respir. J. 26, 511–522 (2005).
Holland, A. E. et al. An official European Respiratory Society/American Thoracic Society technical standard: Field walking tests in chronic respiratory disease. Eur. Respir. J. 44, 1428–1446 (2014).
Meyer, K. C. et al. An Official American Thoracic Society Clinical Practice Guideline: The clinical utility of bronchoalveolar lavage cellular analysis in interstitial lung disease. Am. J. Respir. Crit. Care Med. 185, 1004–1014 (2012).
Yokoyama, A. et al. Circulating KL-6 predicts the outcome of rapidly progressive idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 158, 1680–1684 (1998).
Leuschner, G. & Behr, J. Acute exacerbation in interstitial lung disease. Front. Med. (Lausanne) 4, 176–176 (2017).
Kang, J., Han, M. & Song, J. W. Antifibrotic treatment improves clinical outcomes in patients with idiopathic pulmonary fibrosis: A propensity score matching analysis. Sci. Rep. 10, 15620 (2020).
Cao, M. et al. Acute exacerbations of fibrosing interstitial lung disease associated with connective tissue diseases: A population-based study. BMC Pulm. Med. 19, 215 (2019).
Kamiya, H. & Panlaqui, O. M. Systematic review and meta-analysis of prognostic factors of acute exacerbation of idiopathic pulmonary fibrosis. BMJ Open 10, e035420 (2020).
Acknowledgements
This work was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and Technology (NRF-2019R1A2C2008541), Republic of Korea.
Author information
Authors and Affiliations
Contributions
Conceptualization: J.W.S.; data curation: J.W.S.; formal analysis: M.G.C.; funding acquisition: J.W.S.; investigation: M.G.C., S.M.C., J.H.L., J-K.Y., J.W.S.; project administration: J.W.S.; resources: J.W.S., S.M.C., J.H.L.; software: M.G.C.; supervision: J.W.S.; validation: J.W.S.; visualization: M.G.C; writing—original draft: M.G.C., J.W.S.; writing—review and editing: M.G.C, S.M.C., J.H.L, J-K.Y., J.W.S.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Choi, M.G., Choi, S.M., Lee, J.H. et al. Changes in blood Krebs von den Lungen-6 predict the mortality of patients with acute exacerbation of interstitial lung disease. Sci Rep 12, 4916 (2022). https://doi.org/10.1038/s41598-022-08965-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-08965-9
- Springer Nature Limited