Abstract
Purpose
Sleeve gastrectomy (SG) is a widely used and effective treatment for patients with obesity and comorbid metabolic abnormalities. No specialized tool is available to predict metabolic syndrome (MS) remission after SG. We presented a nomogram that evaluated the probability of MS remission in obese patients 1 year after SG.
Materials and Methods
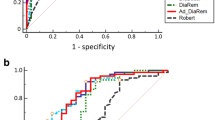
Patients with preoperative MS who underwent SG were enrolled in this retrospective study. They were divided into a training set and a validation set. Multivariate logistic regression analysis was performed to identify independent predictors of MS remission, and these predictors were included in the nomogram. Receiver operating characteristic curve was used to evaluate discrimination. Calibration was performed with the Hosmer–Lemeshow goodness-of-fit test. The net benefits of the nomogram were evaluated using decision curve analysis (DCA).
Results
Three hundred and eighteen patients with a median age of 34.0 years were analyzed. A training set and a validation set with 159 individuals each were established. A combination of age, preoperative high-density lipoprotein cholesterol, elevated triglycerides and glycated hemoglobin level independently and accurately predicted MS remission. The nomogram included these factors. The discriminative ability was moderate in training and validation sets (Area under curve 0.800 and 0.727, respectively). The Hosmer–Lemeshow X2 value of the nomogram was 8.477 (P = 0.388) for the training set and 5.361 (P = 0.718) for the validation set, indicating good calibration. DCA showed the nomogram had clinical benefits in both datasets.
Conclusion
Our nomogram could accurately predict MS remission in Chinese patients with obesity 1 year after SG.
Graphical Abstract






Similar content being viewed by others
Data Availability
The data are not publicly available due to their containing information that could compromise the privacy of the research participants.
References
NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. 2016; 387(10026): 1377–96.
Mottillo S, Filion KB, Genest J, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56(14):1113–32.
Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287(3):356–9.
Li R, Li W, Lun Z, et al. Prevalence of metabolic syndrome in Mainland China: a meta-analysis of published studies. BMC Public Health. 2016;16:296.
Jaspers Faijer-Westerink H, Kengne AP, Meeks KAC, et al. Prevalence of metabolic syndrome in sub-Saharan Africa: a systematic review and meta-analysis. Nutr Metab Cardiovasc Dis. 2020;30(4):547–65.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366(17):1567–76.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. N Engl J Med. 2017;376(7):641–51.
Aminian A, Zajichek A, Arterburn DE, et al. Association of metabolic surgery with major adverse cardiovascular outcomes in patients with type 2 diabetes and obesity. JAMA. 2019;322(13):1271–82.
Arterburn DE, Telem DA, Kushner RF, et al. Benefits and risks of bariatric surgery in adults: a review. JAMA. 2020;324(9):879–87.
Tu Y, Bao Y, Zhang P. Metabolic surgery in China: present and future. J Mol Cell Biol. 2021;13(8):594–609.
Faria G, Pestana D, Aral M, et al. Metabolic score: insights on the development and prediction of remission of metabolic syndrome after gastric bypass. Ann Surg. 2014;260(2):279–86.
Turner PL, Saager L, Dalton J, et al. A nomogram for predicting surgical complications in bariatric surgery patients. Obes Surg. 2011;21(5):655–62.
Ó Hartaigh B, Gransar H, Callister T, et al. Development and validation of a simple-to-use nomogram for predicting 5-, 10-, and 15-year survival in asymptomatic adults undergoing coronary artery calcium scoring. JACC Cardiovasc Imaging. 2018;11(3):450–8.
Wu J, Zhang H, Li L, et al. A nomogram for predicting overall survival in patients with low-grade endometrial stromal sarcoma: a population-based analysis. Cancer Commun (Lond). 2020;40(7):301–12.
Di J, Wang C, Zhang P, et al. The middle-term result of laparoscopic sleeve gastrectomy in Chinese obesity patients in a single hospital, with the review of literatures and strategy for gastric stenosis. Ann Transl Med. 2018;6(24):479.
Liu J, Grundy SM, Wang W, et al. Ethnic-specific criteria for the metabolic syndrome: evidence from China. Diabetes Care. 2006;29(6):1414–6.
Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? Diabetes Care. 2009;32(11):2133–5.
Du X, Fu XH, Peng BQ, et al. Resolution of metabolic syndrome and related metabolic disorders after bariatric surgery: comparison of sleeve gastrectomy and gastric bypass. Surg Obes Relat Dis. 2018;14(9):1348–56.
Hady HR, Dadan J, Luba M. The influence of laparoscopic sleeve gastrectomy on metabolic syndrome parameters in obese patients in own material. Obes Surg. 2012;22(1):13–22.
Chen Y, Chen L, Ye L, et al. Association of metabolic syndrome with prevalence of obstructive sleep apnea and remission after sleeve gastrectomy. Front Physiol. 2021;12: 650260.
Wozniewska P, Diemieszczyk I, Groth D, et al. The influence of patient’s age on metabolic and bariatric results of laparoscopic sleeve gastrectomy in 2-year observation. BMC Surg. 2020;20(1):323.
Batsis JA, Romero-Corral A, Collazo-Clavell ML, et al. Effect of bariatric surgery on the metabolic syndrome: a population-based, long-term controlled study. Mayo Clin Proc. 2008;83(8):897–907.
Chung KW. Advances in understanding of the role of lipid metabolism in aging. Cells. 2021;10(4):880.
Zhao L, Zou X, Feng Z, et al. Evidence for association of mitochondrial metabolism alteration with lipid accumulation in aging rats. Exp Gerontol. 2014;56:3–12.
Fahed G, Aoun L, Bou Zerdan M, et al. Metabolic syndrome: updates on pathophysiology and management in 2021. Int J Mol Sci. 2022;23(2):786.
Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365(9468):1415–28.
Martini F, Anty R, Schneck AS, et al. Predictors of metabolic syndrome persistence 1 year after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2015;11(5):1054–60.
Nassour I, Almandoz JP, Adams-Huet B, et al. Metabolic syndrome remission after Roux-en-Y gastric bypass or sleeve gastrectomy. Diabetes Metab Syndr Obes. 2017;10:393–402.
Succurro E, Marini MA, Arturi F, et al. Usefulness of hemoglobin A1c as a criterion to define the metabolic syndrome in a cohort of italian nondiabetic white subjects. Am J Cardiol. 2011;107(11):1650–5.
Saravia G, Civeira F, Hurtado-Roca Y, et al. Glycated hemoglobin, fasting insulin and the metabolic syndrome in males. Cross-sectional analyses of the Aragon workers' health study baseline. PLoS One. 2015;10(8):e0132244.
Jung JY, Ryoo JH, Chung PW, et al. Association of fasting glucose and glycated hemoglobin with the long-term risk of incident metabolic syndrome: Korean genome and epidemiology study (KoGES). Acta Diabetol. 2019;56(5):551–9.
Acknowledgements
This study was supported by grants from the Clinical Research Plan of SHDC (SHDC2020CR1017B) and Important Disease Joint Research Project in Xuhui Health Systems of Shanghai (XHLHGG202110).
Funding
This work was supported by Clinical Research Plan of SHDC, SHDC2020CR1017B, Yuqian Bao, Important Disease Joint Research Project in Xuhui Health Systems of Shanghai, XHLHGG202110, Yuqian Bao
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
1. A nomogram for MS remission in patients with obesity 1 year after SG is established.
2. The nomogram is composed of age, preoperative HDL-c, HbA1c, and presence of elevated TG.
3. The nomogram predicts MS remission after SG accurately with good calibration and clinical benefits.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pan, Y., Han, X., Tu, Y. et al. Nomogram for Predicting Remission of Metabolic Syndrome 1 Year after Sleeve Gastrectomy Surgery in Chinese Patients with Obesity. OBES SURG 34, 1590–1599 (2024). https://doi.org/10.1007/s11695-024-07156-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-024-07156-x