Abstract
Objectives
One-anastomosis gastric bypass (OAGB) is as effective as Roux-en-Y gastric bypass (RYGB) regarding weight loss and diabetes remission. However, there are no data on gut hormone secretions after OAGB. The aim of this study was to compare fasting and postprandial secretions of gut and pancreatic hormones in OAGB versus RYGB patients.
Design and Methods
Twenty-nine patients, 16 OAGB- and 13 RYGB-operated, underwent a liquid mixed-meal tolerance test at 2 years’ post-surgery. Blood was sampled before and 15, 30, 60, 90, and 120 min after meal for plasma measurement of glucose, C-peptide, insulin, glucagon, GLP-1, GIP, GLP-2, PYY, and ghrelin.
Results
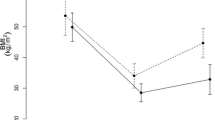
Percentage of total weight loss 2 years post-surgery were -33.9 ± 1.8% for OAGB and -31.2 ± 1.6% for RYGB (p = 0.6). Four patients with persistent diabetes were excluded for further analysis. Fasting and postprandial glucose levels (peaks and area under curve values) were similar between groups. HOMA index was lower in the OAGB group (0.8 ± 0.1 vs 1.3 ± 0.2 in RYGB, p < 0.05). Levels of C-peptide (or insulin) measured at 30 min were significantly lower in OAGB vs RYGB patients (6.9 ± 0.5 vs 9.7 ± 1.1 µg/l, p < 0.05). No difference was observed between OAGB and RYGB groups for GLP-1, GLP-2, PYY, or ghrelin postprandial secretions, but GIP tended to be lower in OAGB vs RYGB patients (756 ± 155 vs 1100 ± 188 pg/ml for postprandial peak concentrations, p = 0.06).
Conclusions
This is the first clinical study showing that OAGB procedure, like RYGB, results in high postprandial secretions of gut hormones, in particular GLP-1.
Trial Registration
Clinical Trials NCT03482895
Graphical abstract


Similar content being viewed by others
Abbreviations
- RYGB:
-
Roux-en-Y gastric bypass
- OAGB:
-
One anastomosis gastric bypass
- EEC:
-
Enteroendocrine cells
- BPL:
-
Biliopancreatic limb
- BMI:
-
Body mass index
- EBMIL:
-
Excess body mass index loss
- HOMA-IR:
-
Homeostatic Model Assessment of Insulin Resistance
- T2D:
-
Type 2 diabetes
- AUC:
-
Area under curve
- GLP-1 or GLP-2:
-
Glucagon-like-peptide-1 or glucagon-like-peptide-2
- PYY:
-
Peptide YY
- GIP:
-
Gastric inhibitory peptide
References
Rubino F, Nathan DM, Eckel RH, Schauer PR, Alberti KGMM, Zimmet PZ, et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by International Diabetes Organizations. Diabetes Care. 2016;39:861–77. https://doi.org/10.2337/dc16-0236.
Halimi S. Chirurgie bariatrique : état des lieux en France en 2019. Médecine des Maladies Métaboliques. 2019;13:677–86. https://doi.org/10.1016/S1957-2557(19)30210-X.
Gimeno RE, Briere DA, Seeley RJ. Leveraging the gut to treat metabolic disease. Cell Metab. 2020;31:679–98. https://doi.org/10.1016/j.cmet.2020.02.014.
Robert M, Espalieu P, Pelascini E, Caiazzo R, Sterkers A, Khamphommala L, et al. Efficacy and safety of one anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity (YOMEGA): a multicentre, randomised, open-label, non-inferiority trial. Lancet. 2019;393:1299–309. https://doi.org/10.1016/S0140-6736(19)30475-1.
Reed MA, Pories WJ, Chapman W, Pender J, Bowden R, Barakat H, et al. Roux-en-Y Gastric Bypass Corrects Hyperinsulinemia Implications for the Remission of Type 2 Diabetes. J Clin Endocrinol Metab. 2011;96:2525–31. https://doi.org/10.1210/jc.2011-0165.
Abou Ghazaleh R, Bruzzi M, Bertrand K, M’harzi L, Zinzindohoue F, Douard R, et al. Is mini-gastric bypass a rational approach for type-2 diabetes? Curr Atheroscler Rep 2017;19:51. https://doi.org/10.1007/s11883-017-0689-3.
Ribeiro-Parenti L, Cavin J-B, Le Gall M. Intestinal adaptations following bariatric surgery: towards the identification of new pharmacological targets for obesity-related metabolic diseases. Curr Opin Pharmacol. 2017;37:29–34. https://doi.org/10.1016/j.coph.2017.08.002.
Lee W-J, Chong K, Lin Y-H, Wei J-H, Chen S-C. Laparoscopic sleeve gastrectomy versus single anastomosis (mini-) gastric bypass for the treatment of type 2 diabetes mellitus: 5-year results of a randomized trial and study of incretin effect. Obes Surg. 2014;24:1552–62. https://doi.org/10.1007/s11695-014-1344-5.
Magouliotis DE, Tasiopoulou VS, Sioka E, Chatedaki C, Zacharoulis D. Impact of bariatric surgery on metabolic and gut microbiota profile: a systematic review and meta-analysis. Obes Surg. 2017;27:1345–57. https://doi.org/10.1007/s11695-017-2595-8.
Magouliotis DE, Tasiopoulou VS, Tzovaras G. One anastomosis gastric bypass versus Roux-en-Y gastric bypass for morbid obesity: an updated meta-analysis. Obes Surg. 2019;29:2721–30. https://doi.org/10.1007/s11695-019-04005-0.
Kim MJ, Park HK, Byun DW, Suh KI, Hur KY. Incretin levels 1 month after laparoscopic single anastomosis gastric bypass surgery in non-morbid obese type 2 diabetes patients. Asian J Surg. 2014;37:130–7. https://doi.org/10.1016/j.asjsur.2013.09.008.
Zubiaga L, Abad R, Ruiz-Tovar J, Enriquez P, Vílchez JA, Calzada M, et al. The effects of one-anastomosis gastric bypass on glucose metabolism in Goto-Kakizaki rats. Obes Surg. 2016;26:2622–8. https://doi.org/10.1007/s11695-016-2138-8.
Marciniak C, Chávez-Talavera O, Caiazzo R, Hubert T, Zubiaga L, Baud G, et al. Characterization of one anastomosis gastric bypass and impact of biliary and common limbs on bile acid and postprandial glucose metabolism in a minipig model. Am J Physiol Endocrinol Metab. 2021. https://doi.org/10.1152/ajpendo.00356.2020.
Poitou C, Bouaziz-Amar E, Genser L, Oppert J-M, Lacorte J-M, Le Beyec J. Fasting levels of glicentin are higher in Roux-en-Y gastric bypass patients exhibiting postprandial hypoglycemia during a meal test. Surg Obes Relat Dis 2018. https://doi.org/10.1016/j.soard.2018.03.014
Roberts GP, Kay RG, Howard J, Hardwick RH, Reimann F, Gribble FM. Gastrectomy with Roux-en-Y reconstruction as a lean model of bariatric surgery. Surg Obes Relat Dis. 2018;14:562–8. https://doi.org/10.1016/j.soard.2018.01.039.
Larraufie P, Roberts GP, McGavigan AK, Kay RG, Li J, Leiter A, et al. Important role of the GLP-1 axis for glucose homeostasis after bariatric surgery. Cell Rep. 2019;26:1399-1408.e6. https://doi.org/10.1016/j.celrep.2019.01.047.
Patrício BG, Morais T, Guimarães M, Veedfald S, Hartmann B, Hilsted L, et al. Gut hormone release after gastric bypass depends on the length of the biliopancreatic limb. Int J Obes (Lond). 2019;43:1009–18. https://doi.org/10.1038/s41366-018-0117-y.
Gasbjerg LS, Helsted MM, Hartmann B, Jensen MH, Gabe MBN, Sparre-Ulrich AH, et al. Separate and combined glucometabolic effects of endogenous glucose-dependent insulinotropic polypeptide and glucagon-like peptide 1 in healthy individuals. Diabetes. 2019;68:906–17. https://doi.org/10.2337/db18-1123.
Nauck MA, Meier JJ. GIP and GLP-1: stepsiblings rather than monozygotic twins within the incretin family. Diabetes. 2019;68:897–900. https://doi.org/10.2337/dbi19-0005.
Lee W-J, Yu P-J, Wang W, Chen T-C, Wei P-L, Huang M-T. Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity: a prospective randomized controlled clinical trial. Ann Surg. 2005;242:20–8.
Acknowledgements
The sponsor was Assistance Publique – Hôpitaux de Paris (APHP) (Direction de la Recherche Clinique et de l’Innovation), represented by the Clinical Research Unit (Hôpital Européen Georges Pompidou, Paris, head: Pr Sandrine KATSAHIAN). We are very grateful to the team of the Clinical Investigation Center (Hôpital Européen Georges Pompidou, Paris) where the patients were monitored for the meal test, and to Melinda Zehani and the technical staff of the endocrine biochemistry department (Hôpital Pitié Salpêtrière, Paris) who realized some of the routine dosages.
Funding
This study was funded by the ANTADIR grant of the Société Francophone de Nutrition Clinique et Métabolique (SFNCM), Institut National de la Santé et de la Recherche Médicale (INSERM), and Assistance Publique Hôpitaux de Paris (APHP).
Author information
Authors and Affiliations
Contributions
DDB, CC, and JLB designed the research; JMC and TB operated the patients; DDB, CRL, and CC recruited the patients; DDB, YF, DB, CC, and JLB conducted the research and collected the data; DDB, MLG, CC, and JLB analyzed the data. DDB, CC, and JLB wrote the manuscript; all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Total weight loss was similar 2 years after OAGB and RYGB.
• The HOMA-IR was lower in OAGB-operated patients 2 years after surgery.
• GLP-1, GLP-2, and PYY postprandial secretions were similar 2 years after OAGB and RYGB.
• GIP postprandial secretion tended to be lower in OAGB- vs RYGB-operated patients.
Rights and permissions
About this article
Cite this article
De Bandt, D., Rives-Lange, C., Frigout, Y. et al. Similar Gut Hormone Secretions Two Years After One Anastomosis Gastric Bypass and Roux-en-Y Gastric Bypass: a Pilot Study. OBES SURG 32, 757–762 (2022). https://doi.org/10.1007/s11695-021-05837-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05837-5