Abstract
Purpose
The effect of altered subsphincteric gastric volume and pressure after bariatric surgery on laryngopharyngeal reflux (LPR) remains largely unknown. This was a cross-sectional pilot study conducted between January 2018 and January 2019 to identify changes in LPR symptoms and signs in bariatric surgery patients presurgery and postsurgery.
Materials and Methods
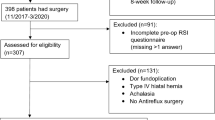
Thirty-four patients listed for bariatric surgery in a single tertiary referral center were recruited, where 31 (77.4% female, mean age 46.3 ± 8.9 years) fulfilled the eligibility criteria. Of the eligible patients, 54.8% and 45.2% underwent sleeve gastrectomy (SG) and gastric bypass (GB), respectively. LPR symptoms were assessed using the self-reported reflux symptom index (RSI). Video-recorded endolaryngeal signs were scored using the reflux finding score (RFS) by two blinded otolaryngologists. Patients’ presurgical and 3-month postsurgical body mass index (BMI), RSI, and RFS were determined. Patients were deemed as having LPR when RSI > 13 or RFS > 7.
Results
There was a significant correlation between the postsurgical RSI and RFS changes (Pearson’s r = 0.474, p = 0.007). Of the 31 patients, 12.9% (RSI) and 6.4% (RFS) recovered from preexisting LPR, whereas 22.6% (RSI) and 3.2% (RFS) developed new de novo LPR postsurgery. The postsurgical mean RFS change improved significantly in the GB group compared with that of the SG group (p < 0.05).
Conclusion
LPR is best assessed clinically using a multimodal approach (RSI and RFS). Bariatric surgery may worsen or lead to de novo LPR. Recognizing the LPR outcomes in these patients is paramount for optimal voice, speech, and swallowing functions.


Similar content being viewed by others
References
Lechien JR, Akst LM, Hamdan AL, et al. Evaluation and management of laryngopharyngeal reflux disease: state of the art review. Otolaryngol Head Neck Surg. 2019;160(5):762–82. https://doi.org/10.1177/0194599819827488.
Dixon JB, Zimmet P, Alberti KG, et al. International Diabetes Federation Taskforce on Epidemiology and Prevention. Bariatric surgery: an IDF statement for obese type 2 diabetes. Diabet Med. 2011;28(6):628–42. https://doi.org/10.1111/j.1464-5491.2011.03306.x.
DeMaria EJ, Sugerman HJ, Kellum JM, et al. Results of 281 consecutive total laparoscopic Roux-en-Y gastric bypasses to treat morbid obesity. Ann Surg. 2002;235(5):640–7. https://doi.org/10.1097/00000658-200205000-00005.
Papasavas PK, Hayetian FD, Caushaj PF, et al. Outcome analysis of laparoscopic Roux-en-Y gastric bypass for morbid obesity. The first 116 cases. Surg Endosc. 2002;16(12):1653–7. https://doi.org/10.1007/s00464-002-8531-5.
Schauer PR, Burguera B, Ikramuddin S, et al. Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg. 2003;238(4):467–85.
DuPree CE, Blair K, Steele SR, et al. Laparoscopic sleeve gastrectomy in patients with preexisting gastroesophageal reflux disease: a national analysis. JAMA Surg. 2014;149(4):328–34. https://doi.org/10.1001/jamasurg.2013.4323.
Boza C, Daroch D, Barros D, et al. Long-term outcomes of laparoscopic sleeve gastrectomy as a primary bariatric procedure. Surg Obes Relat Dis. 2014;10(6):1129–33. https://doi.org/10.1016/j.soard.2014.03.024.
Mandeville Y, Van Looveren R, Vancoillie PJ, et al. Moderating the enthusiasm of sleeve gastrectomy: up to fifty percent of reflux symptoms after ten years in a consecutive series of one hundred laparoscopic sleeve gastrectomies. Obes Surg. 2017;27(7):1797–803. https://doi.org/10.1007/s11695-017-2567-z.
Ulas Biter L, van Buuren MMA, Mannaerts GHH, et al. Quality of life 1 year after laparoscopic sleeve gastrectomy versus laparoscopic Roux-en-Y gastric bypass: a randomized controlled trial focusing on gastroesophageal reflux disease. Obes Surg. 2017;27(10):2557–65. https://doi.org/10.1007/s11695-017-2688-4.
Chuffart E, Sodji M, Dalmay F, et al. Long-term results after sleeve gastrectomy for gastroesophageal reflux disease: a single-center French study. Obes Surg. 2017;27(11):2890–7. https://doi.org/10.1007/s11695-017-2698-2.
El-Hadi M, Birch DW, Gill RS, et al. The effect of bariatric surgery on gastroesophageal reflux disease. Can J Surg. 2014;57(2):139–44. https://doi.org/10.1503/cjs.030612.
Abd Elmonem M, Kamal AEA, Gad A, Radwan H, Elgaaly S. Prevalence of laryngopharyngeal reflux among GERD patients. Al Azhar Assiut Med J. 2012; 10(3 Suppl 3).
Ramzy I, El Shazly M, Marzaban R, et al. Laryngopharyngeal reflux in gastroesophageal reflux disease: does “silent laryngopharyngeal reflux” really exist? Open J Gastroenterol. 2014;4(3):130–40. https://doi.org/10.4236/ojgas.2014.43020.
Groome M, Cotton JP, Borland M, et al. Prevalence of laryngopharyngeal reflux in a population with gastroesophageal reflux. Laryngoscope. 2007;117(8):1424–8. https://doi.org/10.1097/MLG.0b013e31806865cf.
Mohammad NMY. Development of Bahasa Malaysia reflux symptom index (M-RSI) [dissertation]. Kubang Kerian (Kelantan): Universiti Sains Malaysia; 2015. Available from: http://eprints.usm.my/40630/1/Dr._Nik_Mohd_Yunus_Mohamad_%28Otorhinolaryngology_%E2%80%93Head_and_Neck_Surgery%29-24_pages.pdf. Accessed 15 May 2016.
Obesity: clinical assessment and management (Quality standard 127) [Internet]. London: National Institute for Health and Care Excellence (NICE); c2020 [cited 2019. Available from: https://www.nice.org.uk/guidance/qs127. Accessed 20 June 2016.
Kasama K, Mui W, Lee WJ, et al. IFSO-APC consensus statements 2011. Obes Surg. 2012;22(5):677–84. https://doi.org/10.1007/s11695-012-0610-7.
Belafsky PC, Postma GN, Koufman JA. Validity and reliability of the reflux symptom index (RSI). J Voice. 2002;16(2):274–7. https://doi.org/10.1016/s0892-1997(02)00097-8.
Belafsky PC, Postma GN, Koufman JA. The validity and reliability of the reflux finding score (RFS). Laryngoscope. 2001;111(8):1313–7. https://doi.org/10.1097/00005537-200108000-00001.
Kawamura O, Aslam M, Rittmann T, et al. Physical and pH properties of gastroesophagopharyngeal refluxate: a 24-hour simultaneous ambulatory impedance and pH monitoring study. Am J Gastroenterol. 2004;99(6):1000–10.
Vaezi MF. We should learn from important negative results. Laryngoscope. 2006;116(9):1718. https://doi.org/10.1097/01.mlg.0000225954.62763.18.
Bardhan KD, Strugala V, Dettmar PW. Reflux revisited: advancing the role of pepsin. Int J Otolaryngol. 2012;2012:646901. https://doi.org/10.1155/2012/646901.
Tutuian R, Mainie I, Agrawal A, et al. Nonacid reflux in patients with chronic cough on acid-suppressive therapy. Chest. 2006;130(2):386–91. https://doi.org/10.1378/chest.130.2.386.
Mainie I, Tutuian R, Agrawal A, et al. Fundoplication eliminates chronic cough due to non-acid reflux identified by impedance pH monitoring. Thorax. 2005;60(6):521–3. https://doi.org/10.1136/thx.2005.040139.
Becker V, Drabner R, Graf S, et al. New aspects in the pathomechanism and diagnosis of the laryngopharyngeal reflux-clinical impact of laryngeal proton pumps and pharyngeal pH metry in extraesophageal gastroesophageal reflux disease. World J Gastroenterol. 2015;21(3):982–7. https://doi.org/10.3748/wjg.v21.i3.982.
Koufman JA, Aviv JE, Casiano RR, et al. Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg. 2002;127(1):32–5. https://doi.org/10.1067/mhn.2002.125760.
Hicks DM, Ours TM, Abelson TI, et al. The prevalence of hypopharynx findings associated with gastroesophageal reflux in normal volunteers. J Voice. 2002;16(4):564–79. https://doi.org/10.1016/s0892-1997(02)00132-7.
Ayazi S, Lipham JC, Hagen JA, et al. A new technique for measurement of pharyngeal pH: normal values and discriminating pH threshold. J Gastrointest Surg. 2009;13(8):1422–9. https://doi.org/10.1007/s11605-009-0915-6.
Arslan H, Çandar T, Kuran S, et al. New inflammatory parameters in laryngopharyngeal reflux. J Laryngol Otol. 2016;130(9):878–82. https://doi.org/10.1017/S0022215116008653.
Muderris T, Gokcan MK, Yorulmaz I. The clinical value of pharyngeal pH monitoring using a double-probe, triple-sensor catheter in patients with laryngopharyngeal reflux. Arch Otolaryngol Head Neck Surg. 2009;135(2):163–7. https://doi.org/10.1001/archoto.2008.532.
Johnson LF, Demeester TR. Twenty-four-hour pH monitoring of the distal esophagus. A quantitative measure of gastroesophageal reflux. Am J Gastroenterol. 1974;62(4):325–32.
Samuels TL, Johnston N. Pepsin as a marker of extraesophageal reflux. Ann Otol Rhinol Laryngol. 2010;119(3):203–8. https://doi.org/10.1177/000348941011900310.
Merati AL, Ulualp SO, Lim HJ, et al. Meta-analysis of upper probe measurements in normal subjects and patients with laryngopharyngeal reflux. Ann Otol Rhinol Laryngol. 2005;114(3):177–82. https://doi.org/10.1177/000348940511400302.
Abou-Ismail A, Vaezi MF. Evaluation of patients with suspected laryngopharyngeal reflux: a practical approach. Curr Gastroenterol Rep. 2011;13(3):213–8. https://doi.org/10.1007/s11894-011-0184-x.
Ford CN. Evaluation and management of laryngopharyngeal reflux. JAMA. 2005;294(12):1534–40. https://doi.org/10.1001/jama.294.12.1534.
Bove MJ, Rosen C. Diagnosis and management of laryngopharyngeal reflux disease. Curr Opin Otolaryngol Head Neck Surg. 2006;14(3):116–23. https://doi.org/10.1097/01.moo.0000193177.62074.fd.
Acknowledgements
We would like to thank the Director General of Health, Malaysian Ministry of Health, for granting permission to publish this study
Funding
Dr. Suriakanthan and Dr. Pravin Roy assisted in the patient recruitment. Ms. Prema Subramaniam from the Clinical Research Center, Taiping Hospital, Malaysia, facilitated in the registry of study and in obtaining ethical approval. Paramedics Mr. Norizam b. Idris and Mr. Hakimi assisted in data recording and storage.
Author information
Authors and Affiliations
Contributions
Purushotman Ramasamy had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
• Conceptualization and design of study: Purushotman Ramasamy, Vigneswaran Kumarasamy, C. Rajkumar Vinayak, and Shubash Shander Ganapathy
• Acquisition, analysis, and interpretation of data: Purushotman Ramasamy, Vigneswaran Kumarasamy, Avatar Singh Mohan Singh, and Shubash Shander Ganapathy
• Statistical analysis: Shubash Shander Ganapathy and Purushotman Ramasamy
• Administrative, technical, and material support: All authors
• Supervision: Mohd Zulkiflee b. Abu Bakar and Prepageran Narayanan
• Manuscript drafting: Purushotman Ramasamy, Vigneswaran Kumarasamy, and C. Rajkumar Vinayak
• Critical revision of the manuscript for important intellectual content: All authors. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the local medical ethics review board (registration ID: NMRR173558-38038).
Consent to participate
Informed consent was obtained from all individual participants included in the study
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• This cross-sectional pilot study investigates the effect of bariatric surgery on laryngopharyngeal reflux (LPR) using the reflux symptom index (RSI) and endolaryngeal findings score or the reflux finding score (RFS).
• Bariatric surgery produces a spectrum of effect on LPR—from those who improved postsurgery to those with newly developed LPR (de novo LPR)—while some worsened postsurgery.
• Gastric bypass shows relatively better endolaryngeal signs 3 months postsurgery.
• RSI and RFS are the easiest and readily available tools to employ in a multimodal assessment of LPR among bariatric surgery patients.
Rights and permissions
About this article
Cite this article
Ramasamy, P., Kumarasamy, V., Singh, A.S.M. et al. Laryngopharyngeal Reflux Among Patients Undergoing Bariatric Surgery. OBES SURG 31, 3749–3757 (2021). https://doi.org/10.1007/s11695-021-05492-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05492-w