Abstract
Introduction
Gastroesophageal reflux disease (GERD) may manifest atypically as cough, hoarseness or difficulty breathing. However, it is difficult to diagnostically establish a cause-and-effect between atypical symptoms and GERD. In addition, the benefit of laparoscopic anti-reflux surgery (LARS) in patients with laryngopharyngeal manifestations of GERD are not well characterized. We report the largest series reported to date assessing operative and quality of life (QOL) outcomes after LARS in patients experiencing extraesophageal manifestations of GERD and discuss recommendations for this patient population.
Methods
A retrospective review of patients with extraesophageal symptoms and pathologic reflux that underwent LARS between February 2012 and July 2019 was conducted. Inclusion criteria consisted of patients with atypical manifestations of GERD as defined by preoperative survey in addition to physiological diagnosis of pathological reflux. Patient QOL outcomes was analyzed using four validated instruments: the Reflux Symptom Index (RSI), Laryngopharyngeal Reflux QOL, Swallowing QOL (SWAL), and Gastroesophageal Reflux Disease-Health Related Quality of Life (GERD-HRQOL) surveys.
Results
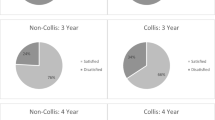
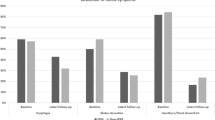
420 patients (24% male, 76% female) with a mean age of 61.7 ± 13.0 years and BMI of 28.6 ± 5.0 kg/m2 were included in this study. Thirty-day wound (0.2%) and non-wound (6.74%) related complication rates were recorded in addition to thirty-day readmission rate (2.6%). Patients reported significant improvements in laryngopharyngeal symptoms at mean follow-up of 18.9 ± 16.6 months post LARS reflected by results of four QOL instruments (RSI − 64%, LPR − 75%, GERD-HRQOL − 80%, SWAL + 18%). The majority of patients demonstrated complete resolution of symptoms upon subsequent encounters with 68% of patients reporting no atypical extraesophageal manifestations during follow-up survey (difficulty breathing − 86%, chronic cough − 81%, hoarseness − 66%, globus sensation − 68%) and 68% of patients no longer taking anti-reflux medication. Seventy-two percent of patients reported being satisfied with their symptom control at latest follow-up.
Conclusions
In appropriately selected candidates with atypical GERD symptomatology and objective diagnosis of GERD LARS may afford significant QOL improvements with minimal operative or long-term morbidity.


Similar content being viewed by others
References
El-Serag HB, Sweet S, Winchester CC et al (2014) Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 63(6):871–880
Wilkund I (2001) Quality of life in patients with gastroesophageal reflux disease. Am J Gastroenterol 96:S46–53
Sidhwa F, Moore A, Alligood E et al (2017) Diagnosis and treatment of the extraesophageal manifestations of gastroesophageal reflux disease. Ann Surg. 265(1):63–67
Heidelbaugh JJ, Gill AS, Harrison RV et al (2008) Atypical presentations of gastroesophageal reflux disease. Am Fam Phys 78(4):483–488
Huggins S (2008) The role of gastroesophageal reflux disease in asthma. J Am Acad Nurse Pract 20:238–242
Takada K, Matsumoto S, Kojima E et al (2011) Prospective evaluation of the relationship between acute exacerbations of COPD and gastroesohpageal reflux disease diagnosed by questionnaire. Respir Med 105:1531–1536
Lee AL, Goldstein RS (2015) Gastroesophageal reflux disease in COPD: links and risks. Int J Chron Obstruct Pulmon Dis 10:1935–1949
Malfertheiner P, Hallerback B (2005) Clinical manifestations and complications of gastroesophageal reflux disease (GERD). Int J Clin Pract 59:346–355
Stefanidis D, Hope WW, Kohn GP et al (2010) Guidelines for surgical treatment of gastroesophageal reflux disease. Surg Endosc 24:2647–2669
Oelschlager BK, Quiroga E, Parra JD et al (2008) Long-term outcomes after laparoscopic antireflux surgery. Am J Gastroenterol 103(2):280–287
Gee DW, Andreoli MT, Rattner DW (2008) Measuring the effectiveness of laparoscopic antireflux surgery: long-term results. Arch Surg 143(5):482–487
Fein M, Bueter M, Thalheimer A (2008) Ten-year outcome of laparoscopic antireflux surgery. J Gastrointest Surg 12(11):1893–1899
Sidhwa F, Moore A, Alligood E et al (2017) Surgical treatment of extraesophageal manifestations of gastroesophageal reflux disease. World J Surg 41:2566–2571
Weltz AS, Zahiri HR, Sibia U et al (2017) Patients are well served by Collis gastroplasty when indicated. Surgery 162:568–576
Park AE, Hoogerboord CM, Sutton E (2012) Use of the falciform ligament flap for closure of the esophageal hiatus in giant paraesophageal hernia. J Gastrointest Surg 16(7):1417–1421
Ghanem O, Sebastian R, Park A (2015) New surgical approach for giant paraesophageal hernia repair: closure of the esophageal hiatus anteriorly using the left triangular ligament. Dig Surg 32(2):124–128. https://doi.org/10.1159/000375131
Belafsky PC, Postma GN, Koufman JA (2002) Validity and reliability of the reflux symptom index (RSI). J Voice. 16(2):274–277
Carrau RL, Khidr A, Gold KF et al (2005) Validation of a quality-of-life instrument for Laryngopharyngeal reflux. Arch Otoyngol Head Neck 131(4):315
McHorney CA, Robbins J, Lomax K et al (2002) The SWAL-QOL and SWAL-CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia 17(2):97
Velanovich V (2007) The development of the GERD-HRQL symptom severity instrument. Diseases Esophagus 20(2):130
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381
Hu Z, Wu J, Liang W (2015) Laparoscopic fundoplication for gastroesophageal reflux disease-related cough: a report of 70 cases. Zhonghua Wei Chang Wai Ke Za Zhi 18(12):1244–1247
Carrasquer A, Targarona EM, Marinello F et al (2012) Laparoscopic fundoplication results in the treatment of the non-gastrointestinal symptoms of gastroesophageal reflux. Cir Esp 90(4):238–242
Moore M, Afaneh C, Benhuri D et al (2016) Gastroesophageal reflux disease: a review of surgical decision making. World J Gastrointest Surg 8(1):77–83
Jobe BA, Richter JE, Hoppo T et al (2013) Preoperative diagnostic workup before antireflux surgery: an evidence and experience-based consensus of the esophageal diagnostic advisory panel. J Am Coll Surg 217(4):586–597
Brown SR, Gyawali CP, Melman L et al (2011) Clinical outcomes of atypical extra-esophageal reflux symptoms following laparoscopic antireflux surgery. Surg Endosc 25(12):3852
Ali T, Roberts DN, Tierney WM (2009) Long-term safety concerns with proton pump inhibitors. Am J Med 122(10):896
Cunningham R, Dale B, Undy B et al (2003) Proton pump inhibitors as a risk factor for Clostridium difficile diarrhea. J Hosp Infect 54:243–245
Laheij RJ, Sturkenboom MC, Hassing RJ et al (2004) Risk of community-acquired pneumonia and use of gastric acid-suppressive drugs. JAMA 292:1955–1960
Eid SM, Boueiz A, Paranji S et al (2010) Patterns and predictors of proton pump inhibitor overuse among academic and non-academic hospitalists. Intern Med 49(23):2561–2568
Funding
No financial support was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Park reports grants and personal fees from Stryker, outside the submitted work; Dr. Addo, Weltz, Zahiri, Connors and Mr. Broda have no conflict of interest or financial or relevant financial ties to disclose.
Informed consent
All authors certify that they accept responsibility as an author and have contributed to the concept, data gathering, analysis, manuscript drafting, and give their final approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Weltz, A.S., Addo, A., Broda, A. et al. The impact of laparoscopic anti-reflux surgery on quality of life: do patients with atypical symptoms benefit?. Surg Endosc 35, 2515–2522 (2021). https://doi.org/10.1007/s00464-020-07665-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07665-7