Abstract
Background
Bariatric surgery is a durable and effective way for the management of obesity and resolution of related comorbidities. The aim of this study is to evaluate the outcome of laparoscopic sleeve gastrectomy (LSG) and one-anastomosis gastric bypass (OAGB) over long term in a South Asian population.
Materials and Methods
This is a prospective randomised trial comparing the outcome of 100 and 101 LSG and OAGB patients respectively after 5-year follow-up. This study is in continuity with previous published papers with 1- and 3-year follow-up. 71 LSG and 73 OAGB patients followed at 5 years. The results of these patients were analysed and compared in terms of %EWL, comorbidity resolution and quality of life (QoL) at 5 years. Bariatric analysis reporting and outcome system (BAROS) was used to assess the outcome of patients.
Results
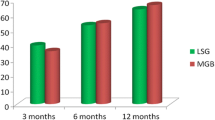
At 5-year follow-up, both LSG and OAGB patients performed well and patients had significant improvement in BMI (kg/m2). The mean preoperative BMI of LSG and OAGB patients was 44.89 ± 7.94 and 45.32 ± 8.24, and their mean BMI at 5 years was 33.41 ± 6.02, 30.80 ± 3.40 respectively. At 5 years, %EWL was 55.95 ± 27.01 and 65.28 ± 13.98 for LSG and OAGB patients respectively. The QoL score of LSG and OAGB patients was 1.86 ± 0.56 and 2.35 ± 0.41 while comorbidity score was 1.84 ± 0.68 and 2.24 ± 0.62 respectively at 5 years.
Conclusions
Both LSG and OAGB are effective bariatric procedures over long term with respect to weight loss, comorbidity resolution and improvement in QoL. OAGB is significantly better than LSG in all the three parameters at 5 years.





Similar content being viewed by others
References
Veenu V, Abdulrehman TA, Bindawas SM. The prevalence of overweight, obesity, hypertension and diabetes in India: analysis of the 2015–2016 National Family Health Survey. Int J Environ Res Public Health. 2019;16(20):3987. https://doi.org/10.3390/ijerph16203987.
Luhar S, Timaeus IA, Jones R, et al. Forecasting the prevalence of overweight and obesity in India to 2040. PLoS One. 2020;15(2):e0229438. https://doi.org/10.1371/journal.pone.0229438.
Bhaskar AG, Prasad A, Raj PP, et al. Trends and progress of bariatric and metabolic surgery in India. Updat Surg. 2020; https://doi.org/10.1007/s13304-020-00774-x.
Oria HE, Moorehead MK. Bariatric analysis and reporting outcome system (BAROS). Obes Surg. 1998;8:487–99.
Seetharamaiah S, Tantia O, Goyal G, et al. LSG vs OAGB—1 year follow-up data: a randomised control trial. Obes Surg. 2017;27(4):948–54.
Shivakumar S, Tantia O, Goyal G, et al. LSG vs MGB-OAGB-OAGB—3 year follow-up data: a randomised control trial. Obes Surg. 2018;28(9):2820–8.
Lakdawala M, Bhasker A. Report: Asian consensus meeting on metabolic surgery. Recommendations for the use of bariatric and gastrointestinal metabolic surgery for treatment of obesity and type II diabetes mellitus in Asian population. Obes Surg. 2010;20(7):929–36.
Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812–21.
Feng J, Gagner M. Laparoscopic bilio-pancreatic diversion with duodenal switch. Semin Laparosc Surg. 2002;9(2):125–9.
Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg. 2001;3:276–80.
Mahawar KK, Borg CM, Kular KS, et al. Understanding objections to one anastomosis (mini) gastric bypass: a survey of 417 surgeons not performing this procedure. Obes Surg. 2017;27(9):2222–8.
De Luca M, Tie T, Ooi G, et al. Mini gastric bypass-one anastomosis gastric bypass (MGB-OAGB)-IFSO position statement. Obes Surg. 2018;28(5):1188–206.
Kular KS, Manchanda N, Rutledge R. A 6- year experience with 1,054 mini-gastric bypasses first study from Indian subcontinent. Obes Surg. 2014;24(9):1430–5.
Taha O, Abdelaal M, Abozeid M, et al. Outcomes of omega loop gastric bypass, 6-years’ experience of 1520 cases. Obes Surg. 2017;27:1952–60.
Carbajo MA, Luque-de-Leon E, Jimenez JM, et al. Laparoscopic one-anastomosis gastric bypass: technique, result, and long-term follow-up in 1200 patients. Obes Surg. 2017;27(5):1153–67.
Peraglie C. Laparoscopic mini-gastric bypass in patients age 60 and older. Surg Endosc. 2016;30(1):38–43.
Noun R, Skaff J, Riachi E, et al. One thousand consecutive mini-gastric bypass: short and long term outcome. Obes Surg. 2012;22(5):697–703.
Neuberg M, Blanchet MC, Gignoux B, et al. Long term outcomes after one-anastomosis gastric bypass (OAGB) in morbidly obese patients. Obes Surg. 2020;30(4):1379–84. https://doi.org/10.1007/s11695-019-04287-4.
Parmar CD, Mahawar KK. One anastomosis (mini) gastric bypass is now an established bariatric procedure: a systematic review of 12,807 patients. Obes Surg. 2018;28(9):2956–67. https://doi.org/10.1007/s11695-018-3382-x
Jammu GS, Sharma R. A 7-year clinical audit of 1107 cases com-paring sleeve gastrectomy, Roux-en-Y gastric bypass, and mini-gastric bypass, to determine an effective and safe bariatric and metabolic procedure. Obes Surg. 2016;26(5):926–32.
Lee W-J, Chong K, Lin Y-H, et al. Laparoscopic sleeve gastrectomy versus single anastomosis (mini-) gastric bypass for the treatment of type 2 diabetes mellitus: 5 year results of randomised trial and study of incretin effect. Obes Surg. 2014;24:1552–62.
Wang F-G, Yu Z-P, Yan W-M, et al. Comparision of safety and effectiveness between laparoscopic mini-gastric bypass and laparoscopic sleeve gastrectomy. Medicine. 2017;96(50):e8924.
Chang W, Bai R, Yan W, et al. Clinical outcomes of one anastomosis gastric bypass versus sleeve gastrectomy for morbid obesity. Obes Surg. 2020;30(3):1021–31.
Parmar CD, Bryant C, Luque-de-Leon E, et al. One anastomosis gastric bypass in morbidly obese patients with BMI ≥50: a systematic review comparing it with Roux-en-Y gastric bypass and sleeve gastrectomy. Obes Surg. 2019;29(9):3039–46.
Rutledge R, Walsh TR. Continued excellent result with the mini-gastric bypass: six-year study in 2,410 patients. Obes Surg. 2005;15(9):1304–8.
Wang W, Wei P-L, Lee Y-C, et al. Short term results of laparoscopic mini-gastric bypass. Obes Surg. 2005;15(5):648–54.
Wityk M, Makarewicz W, Kaczmarkiewicz C, et al. Quality of life after laparoscopic sleeve gastrectomy – review of literature. Eur J Transl Clin Med. 2019;2(2):52–60.
Charalampakis V, Seretis C, Daskalakis M, et al. The effect of laparoscopic sleeve gastrectomy on quality of life: a prospective cohort study with 5-years follow-up. Surg Obes Relat Dis. 2018;14(11):1652–8.
Hachem A, Brennan L. Quality of life outcomes of bariatric surgery: a systematic review. Obes Surg. 2016;26:395–409.
Oria HE, Moorehead MK. Updated bariatric analysis and reporting outcome system (BAROS). Surg Obes Relat Dis. 2009;5:60–6.
Acknowledgements
We extend our heartfelt gratitude to the staff and members of ILS Hospitals, Salt Lake, Kolkata.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The study was conducted after the approval of ILS Hospital Ethics Committee (DCGI & NABH approved EC).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and or national research committee with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jain, M., Tantia, O., Goyal, G. et al. LSG vs MGB-OAGB: 5-Year Follow-up Data and Comparative Outcome of the Two Procedures over Long Term—Results of a Randomised Control Trial. OBES SURG 31, 1223–1232 (2021). https://doi.org/10.1007/s11695-020-05119-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-05119-6