Abstract
Background
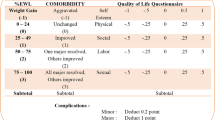
This study aims to evaluate and compare long-term results of laparoscopic sleeve gastrectomy (LSG) and one anastomosis gastric bypass (OAGB) based on bariatric analysis reporting and outcome system (BAROS) score.
Materials and Methods
Patients operated for morbid obesity between 2013 and 2015 were randomised to LSG and OAGB groups. Based on inclusion and exclusion criteria, 201 patients (100 LSG and 101 OAGB) were analysed for changes in total body weight (TBW), body mass index (BMI), percent excess weight loss (%EWL), percent total weight loss (%TWL), QoL (quality of life) scores, comorbidity resolution and outcome based on BAROS at 7 years.
Results
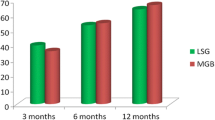
Sixty-six LSG and 64 OAGB patients were followed up at 7 years. Mean pre-operative TBW and BMI were 119 ± 28.2 and 44.87 ± 7.71 for LSG group and 113.25 ± 23.74 and 44.71 ± 8.75 for OAGB group respectively. At 7 years after surgery, there was significant drop in mean TBW and BMI in both groups. Mean %EWL for LSG and OAGB patients was 50.78 ± 28.48 and 59.99 ± 23.32 and mean %TWL for LSG and OAGB patients was 23.22 ± 12.66 and 27.71 ± 12.27 respectively. Mean QoL scores at 7 years were significantly higher than the pre-operative scores and most of the patients in both groups had remission or improvement in their comorbidities. 68.76% OAGB patients had very good or excellent outcome on BAROS score while only 36.37% LSG patients had similar outcome.
Conclusions
LSG and OAGB are successful bariatric procedures over the long term. OAGB outperforms LSG and has significantly higher %EWL and %TWL over the long term.
Graphical Abstract





Similar content being viewed by others
References
Conway B, Rene A. Obesity is a disease: no lightweight matter. Obes Rev. 2004;5(3):145–51.
Xie W, Johnston SS. Bariatric surgery and weight loss in the short- and long-term: evidence from NHANES 2015-2018. Clin Obes. 2023;13(1):e12563.
Arterburn DE, Telem DA, Kushner RF, et al. Benefits and risks of bariatric surgery in adults: a review. JAMA. 2020;324(9):879–87.
Parmar CD, Mahawar KK. One anastomosis (Mini) gastric bypass is now an established bariatric procedure: A systematic review of 12,807 patients. 2018;28(9):2956–67.
Oria HE, Moorehead MK. Bariatric Analysis and Reporting Outcome System (BAROS). Obes Surg. 1998;8:487–99.
Seetharamaiah S, Tantia O, Goyal G, et al. LSG vs OAGB—1 year follow-up data: a randomised control trial. Obes Surg. 2017;27(4):948–54.
Shivakumar S, Tantia O, Goyal G, et al. LSG vs MGB-OAGB-OAGB—3 year follow-up data: a randomised control trial. Obes Surg. 2018;28(9):2820–8.
Jain M, Tantia O, Goyal G, et al. LSG vs MGB-OAGB: 5-year follow-up data and comparative outcome of the two procedures over long term – results of a randomised control trial. Obes Surg. 2021;31(3):1223–32.
Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812–21.
WHO expert consultation. Appropriate body mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63.
Soong TC, Lee MH, Lee WJ, et al. Long-term efficacy of bariatric surgery for the treatment of super-obesity: comparision of SG RYGB and OAGB. Obes Surg. 2021;31(8):3391–9.
Ramos AC, Chevallier JM, Mahawar K, et al. IFSO (International Federation for Surgery of Obesity and Metabolic Disorders) consensus conference statement on one anastomosis gastric bypass (OAGB-MGB): results of a modified Delphi study. Obes Surg. 2020;30(5):1625–34.
Feng J, Gagner M. Laparoscopic bilio-pancreatic diversion with duodenal switch. Semin Laparosc Surg. 2002;9(2):125–9.
Wolf AM, Falcone AR, Kortner B, et al. BAROS: an effective system to evaluate the results of patients after bariatric surgery. Obes Surg. 2000;10(5):445–50.
Kular KS, Manchanda N, Rutledge R. A 6- year experience with 1,054 mini-gastric bypasses first study from Indian subcontinent. Obes Surg. 2014;24(9):1430–5.
Sakran N, Soifer K, Hod K, et al. Long-term reported outcomes following primary laparoscopic sleeve gastrectomy. Obes Surg. 2023;33:117–28.
Kowalewski PK, Olszewski R, Waledziak MS, et al. Long-term outcomes of laparoscopic sleeve gastrectomy-a single-centre, retrospective study. Obes Surg. 2018;28:130–4.
Soong TC, Lee MH, Lee WJ, et al. One anastomosis gastric bypass for the treatment of type 2 diabetes: long term results and recurrence. Obes Surg. 2021;31(3):935–41.
Liagre A, Debs T, Kassir R, et al. One anastomosis gastric bypass with biliopancreatic limb of 150cm: weight loss, nutritional outcomes, endoscopic results, and quality of life at 8-year follow-up. Obes Surg. 2020;30:4206–17.
Tovar JR, Carbajo MA, Jimenez JM, et al. Long-term follow-up after sleeve gastrectomy versus Roux-en-Y gastric bypass versus one-anastomosis gastric bypass: a prospective randomized comparative study of weight loss and remission of comorbidities. Surg Endosc. 2019;33:401–10.
Chang W, Bai R, Yan W, et al. Clinical outcomes of one anastomosis gastric bypass versus sleeve gastrectomy for morbid obesity. Obes Surg. 2020;30(3):1021–31.
Grover BT, Morell MC, Kothari SN, et al. Defining weight loss after surgery: a call for standardization. Obes Surg. 2019;29:3493–9.
Coulman KD, Abdelrahman T, Owen-Smith A, et al. Patient-reported outcomes in bariatric surgery: a systematic review of standards of reporting. Obes Rev Off J Int Assoc Study Obes. 2013;14:707–20.
Kolotin RL, Crosby RD, Koslosky KD, et al. Development of brief measure to assess quality of life in obesity. Obes Res. 2001;9:102–11.
Neuberg M, Blanchet MC, Gignoux B, Frering V. Long-term outcomes after one-anastomosis gastric bypass (OAGB) in morbidly obese patients. 2020;30(4):1379–84.
Znamirowski P, Bryk P, Lewitowicz P, et al. GERD – a burning problem after sleeve gastrectomy. Int J Environ Res Public Health. 2021;15(18):10829.
Saarinen T, Pietilainen KH, Loimaala A, et al. Bile reflux is a common finding in the gastric pouch after one anastomosis gastric bypass. Obes Surg. 2020;30:875–81.
Eldredge TA, Bills M, Ting YY, et al. Once in a bile – the incidence of bile reflux post-bariatric surgery. Obes Surg. 2022;32:1428–38.
Acknowledgements
We extend our heartfelt gratitude to the staff and members of ILS Hospitals, Salt Lake, Kolkata.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Statement of Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Both LSG and OAGB are safe and effective procedures over the long term.
• OAGB outperforms LSG over the long term (7 years).
• Mean %EWL, QoL score and T2DM resolution are significantly better with OAGB over the long term.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jain, M., Tantia, O., Goyal, G. et al. LSG vs OAGB: 7-Year Follow-up Data of a Randomised Control Trial and Comparative Outcome Based on BAROS Score. OBES SURG 34, 1295–1305 (2024). https://doi.org/10.1007/s11695-024-07114-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-024-07114-7