Abstract
Introduction
Roux-en-Y gastric bypass (RYGB) is a well-established treatment for morbid obesity and type 2 diabetes. The effects of RYGB on bone metabolism and bone health are largely unknown.
Objective
Determine the changes in osteoclast function and bone density 1 year after RYGB as compared with a control group undergoing a diabetes support and education program (DSE).
Design
A prospective cohort study with patients matched for weight and age assigned to RYGB or DSE.
Setting
Large academic institution.
Patients or Other Participants
Patients with type 2 diabetes mellitus and morbid obesity (body mass index greater than 35 kg/m2).
Intervention
Subjects either received laparoscopic RYBG or DSE, which consisted of nutritional, exercise, and dietary counseling performed by a certified diabetic educator and a nutritionist three times over a year.
Main Outcome Measure
Osteoclast activity, bone mineral density.
Results
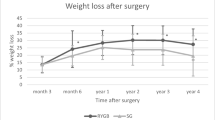
One year after, intervention subjects undergoing RYGB have a 280% increase in osteoclast activity as compared with a 7.6% increase in the DSE control group (P < 0.001). Furthermore, there was a statistically significant increase in sclerostin levels in subjects undergoing RYGB compared with an increase in the control group. The total bone mineral density was statistically unchanged within 1 year of intervention in both groups. A statistically significant decrease in bone mineral density in the left ribs (decrease of 6.8%, P < 0.05) and lumbar spine (decrease of 4.0%, P < 0.05) was seen 1 year after RYGB.
Conclusions
There is a significant increase in osteoclast activity observed 1 year after RYGB; the long-term clinical implications of this increased bone metabolism are unknown.



Similar content being viewed by others
References
Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–14.
Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. Int J Obes. 2013;37(6):889–91.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg. 2009;19(12):1605–11.
Khoo CM, Chen J, Pamuklar Z, et al. Effects of Roux-en-Y gastric bypass or diabetes support and education on insulin sensitivity and insulin secretion in morbidy obese patients with type 2 diabetes. Ann Surg. 2014;259(3):494–501.
Pizzorno L. Bariatric surgery: bad to the bone, part 1. Integr Med. 2016;15(1):48–54.
Chang SH, Stoll CR, Song J, et al. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003 - 2012. JAMA Surg. 2014;149(3):275–87.
Sjöström L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307(1):56–65.
Yu EW. Bone metabolism after bariatric surgery. J Bone Miner Res. 2014;29(7):1507–18.
Pizzorno L. Bad to the bone part 2. Integr Med [Encinitas]. 2016;15(2):35–46.
Yu EW, Bouxsein ML, Putman MS, et al. Two-year changes in bone density after Roux-en-Y gastric bypass surgery. J Clin Endocrinol Metab. 2015;100:1452–9.
Frost HM. Bone “mass” and the “mechanostat”: a proposal. Anat Rec. 1987;219(1):1–9.
Krolner B, Ranlov PJ, Clemmesen T, et al. Bone loss after gastroplasty for morbid obesity: side-effect or adaptive response to weight reduction? Lancet. 1982;1(8278):956–7.
Tsiftsis DDA, Mylonas P, Mead N, et al. Bone mass decreases in morbidly obese women after long limb-biliopancreatic diversion and marked weight loss without secondary hyperparathyroidism. A physiological adaptation to weight loss? Obes Surg. 2009;19(11):1497–503.
Vilarrasa N, San Jose P, Garcia I, et al. Evaluation of bone mineral density loss in morbidly obese women after gastric bypass: 3-year follow-up. Obes Surg. 2011;21:465–72.
Muschitz C, Kocijan R, Marterer C, et al. Sclerostin levels and changes in bone metabolism after bariatric surgery. J Clin Endocrinol Metab. 2015;100(3):891–901.
Scibora LM, Ikramuddin S, Buchwald H, et al. Examining the link between bariatric surgery, bone loss, and osteoporosis: a review of bone density studies. Obes Surg. 2012;22(4):654–67.
Nakamura KM, Haglind EG, Clowes JA, et al. Fracture risk following bariatric surgery: a population-based study. Osteoporos Int. 2014;25(1):151–8.
Rosen HN, Moses AC, Garber J, et al. Serum CTX: a new marker of bone resorption that shows treatment effect more often than other markers because of low coefficient of variability and large changes with bisphosphonate therapy. Calcif Tissue Int. 2000;66(2):100–3.
Piec I, Washbourne C, Tang J, et al. How accurate is your sclerostin measurement? Comparison between three commercially available sclerostin ELISA kits. Calcif Tissue Int. 2016;98:546–55.
Shanbhogue VV, Støving RK, Frederiksen KH, et al. Bone structural changes after gastric bypass surgery evaluated by HR-pQCT: a two-year longitudinal study. Eur J Endocrinol. 2017;176(6):685–93. https://doi.org/10.1530/EJE-17-0014.
Von Mach M-A, Stoeckli R, Bilz S, et al. Changes in bone mineral content after surgical treatment of morbid obesity. Metab Clin Exp. 2004;53(7):918–21.
Yu EW, Bouxsein M, Roy AE, et al. Bone loss after bariatric surgery: discordant results between DXA and QCT bone density. J Bone Miner Res. 2014;29(3):542–50.
Dixon JB, Strauss BJG, Laurie C, et al. Changes in body composition with weight loss: obese subjects randomized to surgical and medical programs. Obesity. 2007;15(5):1187–98.
Hofso D, Bollerslev J, Sandbu R, et al. Bone resportion following weight loss surgery is associated with treatment procedure and changes in secreted Wnt antagonists. Endocrine. 2016;53(1):313–21.
Muschitz C, Kocijan R, Haschka J, et al. The impact of vitamin D, calcium, protein supplementation, and physical exercise on bone metabolism after bariatric surgery: the BABS study. J Bone Miner Res. 2016;31:672–82.
Gagnon C, Schafer AL. Bone health after bariatric surgery. J Bone Miner Res. 2018;2(3):121–33.
Funding
This study was supported by NIH Grant K23 DK075907 to Dr. Alfonso Torquati.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later** amendments or comparable ethical standards.
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tangalakis, L.L., Tabone, L., Spagnoli, A. et al. Effects of Roux-en-Y Gastric Bypass on Osteoclast Activity and Bone Density in Morbidly Obese Patients with Type 2 Diabetes. OBES SURG 30, 290–295 (2020). https://doi.org/10.1007/s11695-019-04154-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04154-2