Abstract
Background
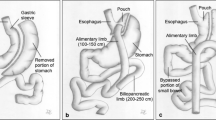
One anastomosis gastric bypass/mini-gastric bypass (OAGB/MGB) is considered an alternative option in metabolic and bariatric surgery. The aim of this study was to evaluate the safety, efficacy and postoperative challenges of OAGB/MGB as a new procedure.
Methods
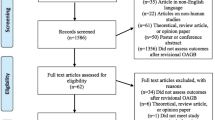
We performed 519 primary MGBs and 8 additional second-stage MGBs during 2014–2018. The data were collected from patients’ notes as well as the surgeons’ prospective data sheets. Two senior surgeons performed the operations. The ultimate primary measures were assessment of the safety and management of the complications. The secondary outcomes were excess weight loss and resolution of the comorbidities.
Results
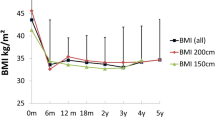
The type 2 diabetes mellitus (T2DM) remission rate was 83% and 70% over 1 and 3 years, respectively (HBA1C < 6.5%). Weight loss was 28–152 kg (SD 23.11). Excess weight loss ranged from 41 to 125%. Hypertension resolution was 61%, 58% and 58% in the first, second and third years, respectively. Ninety-nine per cent of sleep apnoea patients improved symptomatically and went off the continuous positive airway pressure (CPAP) machine. Two (0.37%) patients developed diarrhoea, cured by shortening the afferent biliopancreatic limb (BPL). Eight (1.5%) stomal ulcers were reported. Two patients (0.37%) developed deranged liver function, revised by shortening the BPL in one patient and a reversal in the second patient. The mean follow-up was 2.5 years. Mortality was zero.
Conclusions
This is the largest UK OAGB/MGB study to date showing safety and acceptable results for metabolic syndrome and obesity problems. OAGB/MGB revisional options are rectifying the morbidity and no mortality.
Similar content being viewed by others
References
Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg. 2001;3:276–80.
Rutledge R, Walsh TR. Continued excellent results with the mini-gastric bypass: six-year study in 2,410 patients. Obes Surg. 2005;15:1304–8.
Garcia-Caballero M, Carbajo M. One anastomosis gastric bypass: a simple, safe and efficient surgical procedure for treating morbid obesity. Nutr Hosp. 2004;6:372–5.
Lee W-j, Lin Y-h. Single-anastomosis gastric bypass (SAGB): appraisal of clinical evidence. Obes Surg. 2014;10:1749–56.
Victorzon. Single-anastomosis gastric bypass: Better, faster, and safer? Scand J Surg. 2014;104:48–53.
Kim MJ, Hur KY. Short-term outcomes of laparoscopic single anastomosis gastric bypass (LSAGB) for the treatment of type 2 diabetes in lower BMI (<30 kg/m2) patients. Obes Surg. 2014;24:1044–51.
Chevallier JMA, Gustavo A, Guenzi M, et al. One thousand single anastomosis (omega loop) gastric bypasses to treat morbid obesity in a 7-year period: outcomes show few complications and good efficacy. Obes Surg. 2015;6:951–8.
Musella M, Susa A, Manno E, et al. Complications following the mini/one anastomosis gastric bypass (MGB/OAGB): a multi-institutional survey on 2678 patients with a mid-term (5 years) follow-up. Obes Surg. 2017;27(11):2956–67.
Lee WJ, Ser KH, Lee YC, et al. Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg. 2012;22:1827–34.
Musella M, Apers J, Rheinwalt K, et al. Efficacy of bariatric surgery in type 2 diabetes mellitus remission: the role of mini gastric bypass/one anastomosis gastric bypass and sleeve gastrectomy at 1 year of follow-up. A European survey. Obes Surg. 2016;26(5):933–40.
Carbajo MA, Luque-de-León E, Jiménez JM, et al. Laparoscopic one-anastomosis gastric bypass: technique, results, and long-term follow-up in 1200 patients. Obes Surg. 2017;27(5):1153–67.
Al-Khalifa N, Lee WJ, Hay TC, et al. 15-year experience of laparoscopic single anastomosis (mini-) gastric bypass: comparison with other bariatric procedures. Surg Endosc. 2018;8:3024–31. https://doi.org/10.1007/s00464-017-6011-1.
Mahawar KK, Himpens J, Shikora SA, et al. The first consensus statement on one anastomosis/mini gastric bypass (OAGB/MGB) using a modified Delphi approach. Obes Surg. 2018;28(2):303–12.
Parmar CD, Mahawar KK, Boyle M, et al. Mini gastric bypass: first report of 125 consecutive cases from United Kingdom. Clin Obes. 2016;6:61–7.
http://ww.bomss.org.uk/wp-content/uploads/2014/09/BOMSS-MGB-position-statement-September-2014.pdf. Date of access 26/01/2016.
Agha RA, Borrelli MR, Vella-Baldacchino M, et al. The STROCSS statement: strengthening the reporting of cohort studies in surgery. Int J Surg. 2017;46:198–202.
Kular KS, Manchanda N, Rutledge R. A 6-year experience with 1,054 mini-gastric bypasses-first study from Indian subcontinent. Obes Surg. 2014;24:1430–5.
Quan Y, Huang A, Ye M, et al. Efficacy of laparoscopic mini gastric bypass for obesity and type 2 diabetes mellitus: a systematic review and Meta-Analysis. Gastroenterol Res Pract. 2015;2015:152852.
Parikh M, Eisenberg D, Johnson J, El-Chaar M; American Society for Metabolic and Bariatric Surgery Clinical Issues Committee. Bypass. Surg Obes Relat Dis. 2018.
Kamvissi V, Salerno A, Bornstein SR, et al. Incretins or anti-incretins? A new model for the “entero-pancreatic axis”. Horm Metab Res. 2015;47(1):84–7.
Bruzzi M, Rau C, Voron T, et al. Single anastomosis or mini-gastric bypass: long-term results and quality of life after a 5-year follow-up. Surg Obes Relat Dis. 2015;11:321–6.
Jammu GS, Sharma R. A 7-year clinical audit of 1107 cases comparing sleeve gastrectomy, Roux-En-Y gastric bypass, and mini-gastric bypass, to determine an effective and safe bariatric and metabolic procedure. Obes Surg. 2016;26:926–32.
Ramadan M, Loureiro M, Laughlan K, et al. Risk of dumping syndrome after sleeve gastrectomy and Roux-en-Y gastric bypass: early results of a multicentre prospective study. Gastroenterol Res Pract. 2016;2016:2570237.
Loar 3rd PV, Sanchez-Ramos L, Kaunitz AM, et al. Maternal death caused by midgut volvulus after bariatric surgery. Am J Obstet Gynecol. 2005;5:1748–9.
Facchiano E, Iannelli A, Lucchese M. Internal hernia after mini-gastric bypass: myth or reality? J Visc Surg. 2016;3:231–2.
http://www.websurg.com/Laparoscopic_internal_hernia_repair_after_mini_gastric_bypass-vd01en4097.htm. Date of access 01/05/2017.
Moon RC, Teixeira AF, Jawad MA. Chronic abdominal pain in Roux-en-y gastric bypass and biliopancreatic diversion-duodenal switch patients. Bariatric Times. 2014;11:14–6.
Facchiano E, Leuratti L, Veltri M, et al. Laparoscopic conversion of one anastomosis gastric bypass to roux-en-Y gastric bypass for chronic bile reflux. Obes Surg. 2016;26:701–3.
Johnson WH, Fernanadez AZ, Farrell TM, et al. Surgical revision of loop (“mini”) gastric bypass procedure: multicenter review of complications and conversions to Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2007;1:37–41.
Tolone S, Cristiano S, Savarino E, et al. Effects of omega-loop bypass on esophagogastric junction function. Surg Obes Relat Dis. 2016;12:62–9.
Coblijn UK, Goucham AB, Lagarde SM, et al. Development of ulcer disease after Roux-en-Y gastric bypass, incidence, risk factors, and patient presentation: a systematic review. Obes Surg. 2014;24(2):299–309.
Hussain A, EL-Hasani S. Gastric stomal ulcers following Roux-en-Y gastric bypass. Obes Surg. 2014;24:2171.
D’hondt MA, Pottel H, Devriendt D, et al. Can a short course of prophylactic low-dose proton pump inhibitor therapy prevent stomal ulceration after laparoscopic Roux-en-Y gastric bypass? Obes Surg. 2010;5:595–9.
Lee WJ, Yu PJ, Wang W, et al. Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity: a prospective randomized controlled clinical trial. Ann Surg. 2005;1:20–8.
Mahawar KK, Parmar C, Graham Y, et al. Monitoring of liver function tests after Roux-en-Y gastric bypass: an examination of evidence base. Obes Surg. 2016;26(10):2516–22.
Carbajo M, García-Caballero M, Toledano M, et al. One-anastomosis gastric bypass by laparoscopy: results of the first 209 patients. Obes Surg. 2005;15:398–404.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
A Statement of Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Hussain, A., EL-Hasani, S. Short- and Mid-term Outcomes of 527 One Anastomosis Gastric Bypass/Mini-Gastric Bypass (OAGB/MGB) Operations: Retrospective Study. OBES SURG 29, 262–267 (2019). https://doi.org/10.1007/s11695-018-3516-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3516-1