Abstract
Obesity is a global epidemic and will soon become the number one priority in healthcare management. Bariatric surgery causes a significant improvement in obesity and its related complications. Pre-operative esophago-gastro-duodenoscopy (EGD) is done by several bariatric surgical teams across the world but is still not mandatory.
Aim
To study the percentage of symptomatic and asymptomatic pathological EGD findings in obese patients undergoing bariatric surgery and to analyze whether these findings influence the eventual choice of bariatric surgery.
Materials and Methods
All patients posted for bariatric surgery at our institute from January 2015 to March 2017 had a pre-operative EGD done by the same team of endoscopists.
Results
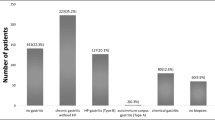
In this study, totally, 675 patients were assessed prior to routine bariatric surgery. 78.52% of all pre-operative patients had an abnormal EGD. The most common endoscopic abnormalities found were hiatus hernia (52.44%), gastritis (46.22%), presence of Helicobacter (H.) pylori (46.67%), reflux esophagitis (16.89%), Barrett’s esophagus (1.78%), gastric erosions (13.19%), and polyps (7.41%). Fifty patients had upper gastrointestinal polyps: 41 in the stomach, 3 in the esophagus, and 6 in the duodenum, mostly benign hyperplastic or inflammatory polyps. Two patients had gastrointestinal stromal tumor (GIST), 6 leiomyoma, and 6 neuroendocrine tumors (NET). Of those with endoscopic evidence of gastroesophageal reflux disease (GERD), 70 (60.03%) of patients were asymptomatic. The pre-operative EGD findings resulted in a change of the planned surgical procedure in 67 (9.93%) patients.
Conclusion
Our study suggests that a large percentage of patients undergoing bariatric surgery have pathologically significant endoscopic findings of which a significant number are asymptomatic; this can lead to a change in the planned bariatric procedure in a section of patients; hence, we believe that EGD should be made mandatory as a pre-operative investigation in all bariatric surgery patients.



Similar content being viewed by others
References
Guh DP, Zhang W, Bansback N, et al. The incidence of co-morbidities related to obesity and over-weight: a systematic review and meta-analysis. BMC Public Health. 2009;25:88.
Muñoz R, Ibáñez L, Salinas J, et al. Importance of routine pre-operative upper GI endoscopy: why all patients should be evaluated? Obes Surg. 2009;19:427–31.
Wadden TA, Frey DL. A multicenter evaluation of a proprietary weight loss program for the treatment of marked obesity: a five-year follow-up. International Journal of Eating Disorders. 22(2):203–12.
Rosenthal RJ. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of >12,000 cases. Surg Obesity Rel Dis. 2012;8:8–19.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles Classification. Gut. 1999;45:172–80.
Hill AD, Kozarek RA, Kraemer SJM, et al. The gastroesophageal flap valve: in vitro and in vivo observations. Gastrointest Endosc. 1996;44:541–7.
Korenkov M, Sauerland S, Shah S, et al. Is routine preoperative upper endoscopy in gastric banding patients really necessary? Obes Surg. 2006;16:45–7.
Zeni TM, Frantzides CT, Mahr C, et al. Value of preoperative upper endoscopy in patients undergoing laparoscopic gastric bypass. Obes Surg. 2006;16:142–6.
Anderson MA, Gan SI, Fanelli RD, et al. ASGE guideline: role of endoscopy in the bariatric surgery patient. Gastrointest Endosc. 2008;68:1–10.
Sharaf RN, Weinshel EH, Bini EJ, et al. Endoscopy plays an important preoperative role in bariatric surgery. Obes Surg. 2004; Nov-Dec;14(10):1367–72.
Kakar K, Singhal V, Khaitan L. Preoperative upper endoscopy should be standard of care for patients undergoing bariatric surgery. SAGES 2014
Victoria Gomez MD, Rajat Bhalla MD, et al. Routine screening endoscopy before bariatric surgery: is it necessary? Bariatric Surgery Practice Patient Care. 2014;9(4):143–9.
Rodriguez Diez, Maria D. et al. Upper endoscopy findings in obese morbid patients candidates for bariatric surgery. Gastroenterol Hepatol 2015; 38(7): 426–430.
Bennett S et al. The role of routine preoperative upper endoscopy in bariatric sx: a systematic review and meta analysis. Surg Obes Relat Dis. 2016;12(5):1116–23.
Di Francesco V, Baggio E, Mastromauro M, et al. Obesity and gastro- esophageal acid reflux: physiopathological mechanisms and role of gastric bariatric surgery. Obes Surg. 2004;14:1095–102.
Bhumika V, Arvind B, Pragati M, et al. Gastroesophageal Reflux disease and its association with BMI: Clinical and Endoscopic Study. J Clin Diagn Res. 2017;11(4):OC01–4.
El-Serag H. The association between obesity and GERD : a review of the epidemiological evidence. Dig Dis Sci. 2008 Sep;53(9):2307–12.
Bennett S, Gostimir M, Shorr R, et al. The role of routine preoperative upper endoscopy in bariatric surgery : a systematic review and meta-analysis. Surg Obes Relat Dis. 2016;12(5):1116–25.
Felsenreich D, Kefurt R, Schermann M, et al. Reflux, sleeve dilation, and Barrett’s esophagus after laparoscopic sleeve gastrectomy: long-term follow-up. Obes Surg. 2017; https://doi.org/10.1007/s11695-017-2748-9.
Genco A, Soricelli E, Casella G, et al. Gastroesophageal reflux disease and Barrett’s esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication. Surg Obes Relat Dis. 2017;13:568–74.
Cobey F, Oelschlager B. Complete regression of Barrett’s esophagus after Roux-en-Y gastric bypass. Obes Surg. 2005;15(5):710–2.
Rasmussen JJ, Fuller W, Ali MR. Marginal ulceration after laparoscopic gastric bypass: an analysis of predisposing factors in 260 patients. Surg Endosc. 2007;21(7):1090–4.
Loewen M, Giovanni J, Barba C. Screening endoscopy before bariatric surgery: a series of 448 patients. Surg Obes Relat Dis. 2008;4:709–12.
Foster A, Richards WO, McDowell J, et al. Gastrointestinal symptoms are more intense in morbidly obese patients. Surg Endosc. 2003;17:1766–8.
Howard DD, Caban AM, Cendan JC, et al. Gastroesophageal reflux after sleeve gastrectomy in morbidly obese patients. Surg Obes Relat Dis. 2011;7:709–13.
DuPree CE, Blair K, et al. Laparoscopic sleeve gastrectomy in patients with preexisting gastroesophageal reflux disease, a national analysis. JAMA Surgery. 2014;149(4):328–34.
Adlekha C et al. Prevalence of H. Pylori infection among patients undergoing upper gastrointestinal endoscopy in a Medical College Hospital in Kerela, India. Ann Med Health Sci Res. 2013;3(4):559–63.
Hooi KY, Wong WS, Kaplan GG, et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology. 2017;153(2):420–9.
Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection—the Maastricht IV/ Florence Consensus. Gut. 2012;61:646–64.
Papasavas PK, Gagne DJ, Donnelly PE, et al. Prevalence of Helicobacter pylori infection and value of preoperative testing and treatment in patients undergoing laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2008;4(3):383–8.
Erim T, Cruz-Correa MR, Szomstein S, et al. Prevalence of Helicobacter pylori seropositivity among patients undergoing bariatric surgery: a preliminary study. World J Surg. 2008;32:2021–5.
Verma S, Sharma D, Kanwar P, et al. Prevalence of helicobacter pylori infection in bariatric patients: a histologic assessment. Surg Obes Relat Dis. 2013;9:679–85.
Schirmer B, Erenoglu C, Miller A. Flexible endoscopy in the management of patients undergoing Roux-en-Y gastric bypass. Obes Surg. 2002;12:634–8.
Sharaf RN, Weinshel EH, Bini EJ, et al. Endoscopy plays an important preoperative role in bariatric surgery. Obes Surg. 2004;14:1367–72.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient – 2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic and Bariatric Surgery. Obesity. 2013;21:S1–S27.
ASGE Standards of Practice Committee. The role of endoscopy in the bariatric surgery patient. Surg Endosc. 2015 May;29(5):1007–17.
Sauerland S, Angrisani L, Belachew M, et al. Obesity surgery. Evidence-based guidelines of the European Association for Endoscopic Surgery (E.A.E.S.). Surg Endosc. 2005;19:200–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflict of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human and Animal Rights
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
D’Silva, M., Bhasker, A.G., Kantharia, N.S. et al. High-Percentage Pathological Findings in Obese Patients Suggest that Esophago-gastro-duodenoscopy Should Be Made Mandatory Prior to Bariatric Surgery. OBES SURG 28, 2753–2759 (2018). https://doi.org/10.1007/s11695-018-3230-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3230-z