Abstract
Introduction
Leishmaniasis is a neglected disease with high prevalence and incidence in tropical and subtropical areas. Existing drugs are limited due to cost, toxicity, declining efficacy and unavailability in endemic places. Drug repurposing has established as an efficient way for the discovery of drugs for a variety of diseases.
Purpose
The objective of the present work was testing the antileishmanial activity of thioridazine, an antipsychotic agent with demonstrated effect against other intracellular pathogens.
Methods
The cytotoxicity for mouse peritoneal macrophages as well as the activity against Leishmania amazonensis, Leishmania mexicana and Leishmania major promastigotes and intracellular amastigotes, as well as in a mouse model of cutaneous leishmaniasis, were assessed.
Results
Thioridazine inhibited the in vitro proliferation of promastigotes (50% inhibitory concentration—IC50—values in the range of 0.73 µM to 3.8 µM against L. amazonensis, L. mexicana and L. major) and intracellular amastigotes (IC50 values of 1.27 µM to 4.4 µM for the same species). In contrast, in mouse peritoneal macrophages, the 50% cytotoxic concentration was 24.0 ± 1.89 µM. Thioridazine inhibited the growth of cutaneous lesions and reduced the number of parasites in the infected tissue of mice. The dose of thioridazine that inhibited lesion development by 50% compared to controls was 23.3 ± 3.1 mg/kg and in terms of parasite load, it was 11.1 ± 0.97 mg/kg.
Conclusions
Thioridazine was effective against the promastigote and intracellular amastigote stages of three Leishmania species and in a mouse model of cutaneous leishmaniasis, supporting the potential repurposing of this drug as an antileishmanial agent.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term “leishmaniasis” encompasses a group of clinically distinct diseases caused by over 20 protozoan species of the genera Leishmania and Endotrypanum [1]. Leishmaniasis is important not only for the high incidence, prevalence and mortality, but also due to its disabling effect. An estimated 700,000 to 1 million new cases occur annually. However, beyond the suffering and lost human lives, the disease is an economical burden for the poorest sectors, which are the most vulnerable population [2, 3].
Pentavalent antimony compounds were the drugs of choice for several decades and are the first line drugs in many countries today. Amphotericin B, pentamidine, paromomycin (either injectable or topical) and miltefosine are the main therapeutic alternatives. In general, drug toxicity, cost, parasite resistance and the variable efficacy (depending on the nosogeographical entity) have limited the impact of treatment at the individual level and as a control measure. Therefore, the development of new, less toxic, more efficacious, and affordable antileishmanial drugs is considered a need [4,5,6].
The cost and time needed for the development of a new chemical entity to the final registration as a drug have been estimated to over US$ 2000 million and 12–15 years and the chances of returning such high investment in the context of a drug indicated for a disease that primarily affects poor countries are remote [7, 8].
Drug repositioning (finding new uses to already licensed drugs for other indications or drugs that have failed clinical trials due to efficacy issues) has emerged as a cost-effective alternative for the development of drugs for neglected diseases [9, 10]. In addition, a repositioned drug may advance quickly from in vitro and in vivo activity assays to its nomination as a drug candidate and to safety and efficacy clinical trials. Moreover, the cost of development has been estimated to be reduced in about US$ 320 million [11]. The likelihood of failure at the latest phases of development, which are the most expensive ones, also decreases since most of the pharmacology and safety profile of the compound is known in advance.
Current antileishmanial drugs including miltefosine (primarily developed as anticancer drug), amphotericin B (antifungal drug), pentamidine (antifungal—treatment of pneumonia caused by Pneumocystis jiroveci) and paromomycin (antibiotic), together with others that have demonstrated antileishmanial activity at experimental level [12,13,14], support the potential of drug repositioning for leishmaniasis.
Thioridazine is a first-generation phenothiazine antipsychotic drug that has gained attention in recent years as a repurposed drug for the treatment of cancer [15, 16], as well as bacterial [17, 18] and mycobacterial infections [19, 20].
Besides its intrinsic antimicrobial activity, thioridazine inhibits efflux pumps that mediate drug resistance in a number of microbes. For this reason, thioridazine has been tested in combination with other drugs in order to either potentiate drug effect or to revert drug resistance [16, 21]. As examples, thioridazine acts in synergy with the beta-lactam antibiotic, dicloxacillin, to kill methicillin-resistant Staphylococcus aureus in vitro and in a mouse model of peritonitis [22,23,24]. Molecular dynamics simulations suggest that such effect is probably mediated by inhibition of S. aureus efflux pump NorA [24]. Thioridazine increases the intracellular accumulation of the efflux pump substrate ethidium bromide in Mycobacterium smegmatis and Mycobacterium avium and inhibits the intrinsic efflux pump system of M. avium that causes erythromycin resistance [25]. In M. tuberculosis, thioridazine inhibits the respiration [26] and the efflux of rifampicin, a process principally mediated by proton gradient-dependent transporters [27].
Thioridazine is also active against Trypanosoma cruzi in vitro and in animal models [28]. In Leishmania braziliensis, Leishmania guyanensis, and Leishmania mexicana, thioridazine inhibits the energy-dependent efflux of pirarubicin and calcein cetoxymethylester, which are both well-known substrates of the mammalian multidrug-resistant pumps [29]. However, to the best of our knowledge, there is no previous report on the antileishmanial activity of thioridazine. Therefore, the aim of the present work was studying the in vitro inhibitory activity of thioridazine against the promastigote and intracellular amastigote stages of three Leishmania species as well as in mouse experimentally infected with Leishmania amazonensis.
Materials and Methods
Parasites and Cultures
L. amazonensis MHOM/BR/77/LTB0016 reference strain was kindly donated by the Department of Immunology of Fundação Oswaldo Cruz (Fiocruz), Brazil. L. mexicana MNYC/BZ/62/M379 and L. major MHOM/IL/81/Friedlin reference strains were kindly donated by Paul A. Bates, Division of Biomedical and Life Sciences, Faculty of Health and Medicine, Lancaster University, United Kingdom. The promastigotes were cultivated at 26 °C in Schneider’s Insect Medium (Sigma-Aldrich, St. Louis, MO, U.S.A.) supplemented with 10% heat-inactivated (56 °C, 30 min) fetal bovine serum (Gibco, USA) and antibiotics (200 UI penicillin and 200 µg/mL streptomycin). Exponential multiplication of the promastigotes of the three species was attained by passages every 3–4 days. Intracellular amastigotes were multiplied in mouse peritoneal macrophages obtained by peritoneal lavage of BALB/c mice and cultivated in RPMI-1640 medium supplemented with fetal bovine serum and antibiotics as described for Schneider’s Insect Medium.
Test Compound
Thioridazine was supplied by BioCubaFarma, (Havana, Cuba) and was part of a commercial lot of pharmacologically active ingredient used to produce tablets. The sample satisfied quality specifications, was accompanied by the quality certificate and had 99.7% purity. For in vitro studies, the compound was dissolved in dimethyl sulfoxide (DMSO, Sigma-Aldrich, St. Louis, MO, USA) at 10 mg/mL and then serially diluted in an appropriate concentration range depending on its activity and the type of assay. For in vivo experiments, thioridazine was dissolved in 0.9% saline solution. Amphotericin B deoxycholate (Gibco, USA) was dissolved in sterile distilled water and used as positive control of activity for in vitro and in vivo assays.
Activity Against Promastigotes
The growth inhibition assay was conducted according to Bodley and Shapiro’s procedure [30]. Briefly, all wells in the 96-well culture plate were seeded with 199 µL of culture medium containing 5 × 105 stationary phase promastigotes/mL. One microliter of compound solutions in DMSO was then added per well, the plate was sealed with parafilm and incubated for 72 h at 26 °C. Control wells were treated with 1 µL DMSO. After the incubation period, 20 μL of 20 mg/mL p-nitro-phenyl-phosphate (Sigma-Aldrich) in sodium acetate (pH 5.5)—1% Triton X100 was added to each well. Plates were incubated for 3 h at 37 °C and absorbance was read in a Tecan Infinite 200 Pro microplate reader at 405 nm. Fifty percent inhibitory concentrations (IC50) were estimated by non-linear fitting to the sigmoid Emax equation [31]. Each drug concentration was tested in quadruplicate and the assay was repeated three times.
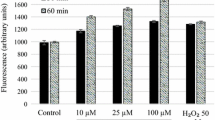
Cytotoxicity Assay in Mouse Peritoneal Macrophages
BALB/c mice were killed by CO2 inhalation and their peritoneal macrophages were collected by washing the abdominal cavity with cold RPMI-1640 culture medium supplemented with antibiotics (sodium penicillin 200 UI and streptomycin 200 µg/mL) and 10% fetal bovine serum. The macrophages were distributed in 96-well culture plates at 105 cells/well. After 4 h incubation at 37 °C and 5% CO2, the culture medium was replaced by fresh medium containing test compounds and the plates were incubated for other 48 h. Afterwards, 10 µL Alamar Blue (DAL1025, Thermo Fisher Scientific) was added per well. After other 6–8 h of incubation (37 °C and 5% CO2), the reduction of Alamar Blue by viable cells was assessed by reading fluorescence at EX/EM 530/585 nm (cutoff, 550 nm) in a Tecan Infinite 200 Pro microplate reader. Fifty percent cytotoxic concentrations (CC50) were estimated by non-linear fitting to the Emax sigmoid model [31].
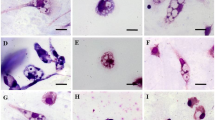
Drug Activity Against Intracellular Amastigotes
Mouse peritoneal macrophages were collected, seeded in 96-well culture plates at 105 cells/well and incubated at 34 °C, 5% CO2 for 2 h. Non-adherent cells were removed by change of the culture medium and the adhered cells were infected with stationary phase promastigotes (either L. amazonensis, L. mexicana or L. major promastigotes) at a rate of four parasites per host cell for L. amazonensis and ten parasites per macrophage for the other two species. After 4 h of incubation at 34 °C and 5% CO2, free promastigotes were eliminated, and the medium was replaced by 199 µL culture medium and 1 µL test compound solutions in DMSO. Four replicates of each drug concentration were tested in every assay. Plates were then incubated for 72 h at 37 °C and 5% CO2. Afterwards, the culture medium was discarded, replaced by Schneider’s Insect Medium and the plates were incubated for other 72 h at 26 °C to allow surviving amastigotes to transform into promastigotes and replicate. P-nitro-phenyl-phosphate was then added to each well as described in the promastigote assay and the IC50 values were estimated as previously indicated.
Animals
Female, 16–18 g, 6–8-weeks-old BALB/c mice were supplied by the National Center for the Production of Laboratory Animals (Cuba). They were maintained under controlled environmental conditions (room temperature 22–25 °C, relative humidity 60–65%, light cycle 10 h light-14 h dark) and were handled by qualified personnel. At the end of studies, mice were killed by CO2 inhalation. The experimental protocol was approved by the Institutional Ethics Committee for the Care and Use of Laboratory Animals of the Center of Bioactive Chemicals (CBQ/CEAE/2021.4).
In Vivo Antileishmanial Assay
Fifty mice were infected by intradermal inoculation in the left hind footpads with 107 stationary phase L. amazonensis promastigotes. Once lesions developed (21 days post-infection), mice were randomly allocated to five experimental groups and were treated for 14 days. Two groups were treated with thioridazine (50 or 25 mg/kg, intraperitoneal route); one with amphotericin B (5 mg/kg, intraperitoneal route, every other day); one with 0.9% saline solution (0.2 mL, intraperitoneal route); and one group received no-treatment at all (control group).
The dorsoplantar diameters of both rear limbs were weekly measured using a caliper (Krœplin, Längenmesstechnick, error 0.05 mm). Lesion size was calculated by subtracting the measure of the non-infected pad to that of the infected one. The groups were statistically compared by repeated measures analysis of variance, the Fisher’s least significant difference test and the Dunnett’s test, using STATISTICA software [32].
Four mice per group were killed 2 weeks after the end of therapy and the number of amastigotes in the infected tissue was determined by the limiting dilution assay technique as described elsewhere [33]. Parasite loads were compared by Kruskal–Wallis test and the distribution-free multiple comparisons test. Values of p under 0.05 were considered statistically significant.
Dose–Effect of Thioridazine Against Experimental Cutaneous Leishmaniasis
Experimentally infected mice (as described above) with evident lesions were randomized and then treated by intraperitoneal route for 14 days with either thioridazine at 25, 20, 15, 10 or 5 mg/kg; amphotericin B at 5 mg/kg or were not treated at all (control). The lesion size and parasite loads were assessed and statistically analyzed as described for the previous assay. The doses reducing lesion size and parasite load by 50% compared to controls were estimated by non-linear fitting of dose–effect curves.
Results
In Vitro Antileishmanial Activity and Cytotoxicity
Thioridazine was active against L. amazonensis, L. mexicana and L. major promastigotes (Table 1). IC50 values ranged from 1.73 µM to 3.8 µM and L. amazonensis seamed slightly more sensitive than the two other species. It was also active against intracellular amastigotes of the three species of Leishmania tested. The IC50 values against intracellular amastigotes ranged from 1.27 to 4.4 µM.
Thioridazine was moderately cytotoxic for the host mammalian cells (mouse peritoneal macrophages); however, CC50 values were significantly higher than the IC50 values against the intracellular amastigotes for the three Leishmania species tested.
Efficacy in a Murine Model of Cutaneous Leishmaniasis
Dose-finding pilot studies (data not shown) were conducted prior to the activity assays to identify maximum tolerable doses (MTD). Thioridazine was daily administered by intraperitoneal route for 21 days and the MTD was 50 mg/kg. Higher doses of thioridazine (100 mg/kg) caused a severe and lethal lethargy of mice.
In the first in vivo activity study, thioridazine was administered at its MTD and at half the MTD, i.e., 50 mg/kg and 25 mg/kg (Fig. 1). At both dose levels, it was observed a statistically significant arrest of lesion growth compared to non-treated mice (p < 0.01). It is relevant that the effect of thioridazine was evident since the first week of treatment (50 mg/kg, p < 0.05), whereas amphotericin B required 3 weeks of treatment to demonstrate a visible and statistically significant effect.
The number of parasites in the infected skin tissue 2 weeks after the end of therapy (Fig. 2) was in correspondence with lesion size. Mice treated with thioridazine at 50 mg/kg and 25 mg/kg showed 96.7% and 96.2% reduction of parasite load, respectively, compared to controls (p < 0.01) and were similar (p > 0.1) to amphotericin B-treated mice (95.5% reduction). The effect of thioridazine at the two dose levels was similar (p > 0.1) both in terms of lesion size and parasite load.
In the second animal efficacy study, thioridazine was administered at doses from 5 to 25 mg/kg (Fig. 3). A statistically significant effect on lesion size compared to control mice was achieved with doses from 15 to 25 mg/kg. The estimated 50% effective dose (ED50; mean ± standard error) at 21 days after the onset of treatment was 23.3 ± 3.1 mg/kg and 24.1 ± 2.9 mg/kg at 28 days. Comparable results were obtained in terms of parasite loads at 28 days (Fig. 4), however, with a lower ED50 of 11.1 ± 0.97 mg/kg.
Discussion
Thioridazine is a piperazine phenothiazine derivative which acts by postsynaptic inhibition of dopamine receptors. Thioridazine has other peripheral and central nervous system effects, producing both alpha-adrenergic stimulation and blocking histamine- and serotonin-mediated effects. Thioridazine is indicated for the therapy of acute and chronic psychosis. It was approved for use in the United States in 1978 and was formerly a commonly prescribed antipsychotic medication, but in recent years has been replaced in large part by the atypical antipsychotics, which have fewer extrapyramidal side effects. Use of thioridazine is also restricted because of its propensity to cause prolongation of the QTc interval and increased risk of sudden death. The recommended dose in adults is 50 mg to 100 mg three times daily, increasing based upon effect and tolerance to a maximum of 800 mg daily [34]. Despite its side effects, thioridazine has been the recent focus of repurposing as an anticancer drug [15, 16, 35, 36], as an antibacterial [17,18,19,20, 37, 38] and as an antiviral [39].
To our knowledge, there is no previous report on the antileishmanial activity of thioridazine neither In vitro (promastigotes and amastigotes) nor in vivo. However, it is known that some phenothiazine derivatives, thioridazine inclusive, can inhibit energy-dependent efflux systems in L. guyanensis, L. braziliensis and L. mexicana promastigotes [29].
In the present study, low concentrations of thioridazine inhibited proliferation of In vitro cultured promastigotes and amastigotes. The activity was specific, as indicated by appropriate therapeutic indices in both the extracellular and the intracellular In vitro systems. Thioridazine was also capable of reducing the growth of lesions and the load of parasites in the skin of mice experimentally infected with L. amazonensis. Furthermore, the in vivo effect of thioridazine was comparable to that of amphotericin B at 5 mg/kg used as positive control.
Thioridazine showed a dose-dependent and statistically significant effect in vivo at doses from 15 to 25 mg/kg. The maximum recommended dose in humans is 800 mg/day (about 11.4 mg/kg for a patient of 70 kg) [34, 40], which is allometrically equivalent to 137 mg/kg in mice [41]. According to these figures, thioridazine could be a relatively safe systemic alternative treatment for cutaneous leishmaniasis. However, daily oral doses above 50 mg/kg caused a severe respiratory depression in mice and 100 mg/kg were lethal.
Though thioridazine was widely used for years as an antipsychotic agent (and it is still used in many countries), its indication as an oral drug for cutaneous leishmaniasis could raise ethical concern, due to the potential occurrence of severe side effects in the context of a nonlethal form of the disease. Consequently, developing a formulation of thioridazine for topical used could be more reasonable. Given its molecular weight (370.6 g/mol) and lipophilicity (logKo/w = 5.90) values, the development of a formulation with proper skin permeability is theoretically feasible according to the values of permeability constant (1.2–4.3 × 10–5 cm/s) calculated using three different QSAR models [42,43,44].
Like Leishmania amastigotes, M. tuberculosis resides inside macrophages. Accessing inner cell compartments could be a problem for other drugs, but thioridazine. This drug accumulates inside macrophages and reaches higher intra-macrophagic concentration compared to that in blood plasma [45, 46]. The In vitro activity of thioridazine against M. tuberculosis, its efficacy as monotherapy and in combination with anti-tuberculosis drugs in animal models, as well as in extensively drug-resistant tuberculosis patients have been reported [47, 48]. Thioridazine acts synergistically with anti-tuberculosis drugs in vivo, particularly against drug-resistant M. tuberculosis strains [45, 49]. Based on such results, the second use of thioridazine as a drug for the treatment of tuberculosis has been proposed.
Thioridazine improves cardiac function and survival time in acute and chronic murine models of Chagas’ disease [28]. Moreover, phenothiazine derivatives also inhibit two major T. cruzi enzymes: trypanothione reductase and dihydrolipoamide dehydrogenase [50, 51]. Due to the close taxonomic relationship between Leishmania spp. and T. cruzi, thioridazine probably inhibits the homologous enzymes in Leishmania spp.
Efflux pumps not only participate in drug extraction from the cell and mediate drug resistance [17, 27, 29] but they are also involved in the physiological detoxication of the cell by preventing the accumulation of harmful metabolic byproducts [16, 52]. This way, efflux pump inhibition by thioridazine potentially mediates its direct antileishmanial effect by promoting the intracellular accumulation of waste products.
In conclusion, the results demonstrated the potential of thioridazine as an antileishmanial drug, which is further supported by thioridazine activity against intracellular pathogens such as T. cruzi and M. tuberculosis. Aspects like its activity in murine models of visceral leishmaniasis, the interaction with currently used antileishmanial drugs (specially in drug-resistant strains) and the antileishmanial activity of potential neurologically inert thioridazine metabolites (thioridazine-5-sulphoxide) [46] and derivatives as well as nanoencapsulated thioridazine [53] deserve additional investigation.
Data availability
Primary data supporting the results are available upon request to the corresponding author.
References
Mathison BA, Bradley BT (2023) Review of the clinical presentation, pathology, diagnosis, and treatment of leishmaniasis. Lab Med 54(4):363–371. https://doi.org/10.1093/labmed/lmac134
Alvar J, Vélez ID, Bern C, Herrero M, Desjeux P, Cano J, Jannin J, den Boer M, The WHO Leishmaniasis Control Team (2012) Leishmaniasis worldwide and global estimates of its incidence. PLoS ONE 7(5):e35671. https://doi.org/10.1371/journal.pone.0035671
- WHO. Leishmaniasis. Last updated: 12 January 2023, Accessed: 10 Mar 2023. https://www.who.int/news-room/fact-sheets/detail/leishmaniasis
Brindha J, Balamurali MM, Chanda K (2021) An overview on the therapeutics of neglected infectious diseases—leishmaniasis and chagas diseases. Front Chem 9:622286. https://doi.org/10.3389/fchem.2021.622286
Chakravarty J, Sundar S (2019) Current and emerging medications for the treatment of leishmaniasis. Expert Opin Pharmacother 20:1251–1265. https://doi.org/10.1080/14656566.2019.1609940
Knight CA, Harris DR, Alshammari SO, Gugssa A, Young T, Lee CM (2023) Leishmaniasis: recent epidemiological studies in the Middle East. Front Microbiol 13:1052478. https://doi.org/10.3389/fmicb.2022.1052478
Adams CP, Brantner VV (2006) Estimating the cost of new drug development: Is it really $802 million? Health Aff 25(2):420–428. https://doi.org/10.1377/hlthaff.25.2.420
Wouters OJ, McKee M, Luyten J (2020) Estimated research and development investment needed to bring a new medicine to market, 2009–2018. JAMA 323(9):844–853. https://doi.org/10.1001/jama.2020.1166
Andrews KT, Fisher G, Skinner-Adams TS (2014) Drug repurposing and human parasitic protozoan diseases. Int J Parasitol Drugs Drug Resist 4(2):95–111. https://doi.org/10.1016/j.ijpddr.2014.02.002
Charlton RL, Rossi-Bergmann B, Denny PW, Steel PG (2018) Repurposing as a strategy for the discovery of new anti-leishmanials: the-state-of-the-art. Parasitology 145(2):219–236. https://doi.org/10.1017/S0031182017000993
Sateriale A, Bessoff K, Sarkar IN, Huston CD (2014) Drug repurposing: mining protozoan proteomes for targets of known bioactive compounds. J Am Med Inform Assoc 21(2):238–244. https://doi.org/10.1136/amiajnl-2013-001700
Melcon-Fernandez E, Galli G, García-Estrada C, Balaña-Fouce R, Reguera RM, Pérez-Pertejo Y (2023) Miltefosine and nifuratel combination: a promising therapy for the treatment of Leishmania donovani visceral leishmaniasis. Int J Mol Sci 24:1635. https://doi.org/10.3390/ijms24021635
El-Dirany R, Fernández-Rubio C, Peña-Guerrero J (2022) Repurposing the antibacterial agents peptide 19–4LF and peptide 19–2.5 for treatment of cutaneous Leishmaniasis. Pharmaceutics 14(11):2528. https://doi.org/10.3390/pharmaceutics14112528
Borges BS, Bueno GP, Tomiotto-Pellissier F, Figueiredo FB, Soares Medeiros LC (2023) In vitro anti-Leishmania activity of triclabendazole and its synergic effect with amphotericin B. Front Cell Infect Microbiol 12:1044665. https://doi.org/10.3389/fcimb.2022.1044665
Tran TH, Kao M, Liu HS, Hong YR, Su Y, Huang CYF (2023) Repurposing thioridazine for inducing immunogenic cell death in colorectal cancer via eIF2α/ATF4/CHOP and secretory autophagy pathways. J Cell Commun Signal 21(1):184. https://doi.org/10.1186/s12964-023-01190-5
Rácz B, Spengler G (2023) Repurposing antidepressants and phenothiazine antipsychotics as efflux pump inhibitors in cancer and infectious diseases. Antibiotics 12(1):137. https://doi.org/10.3390/antibiotics12010137
Mirzaii M, Alebouyeh M, Sohrabi MB, Eslami P, Fazli M, Ebrahimi M, Rashidan M (2023) Antibiotic resistance assessment and multi-drug efflux pumps of Enterococcus faecium isolated from clinical specimens. J Infect Dev Ctries 17(05):649–655. https://doi.org/10.3855/jidc.17304
Vo N, Sidner BS, Yu Y, Piepenbrink KH (2023) Type IV pilus-mediated inhibition of Acinetobacter baumannii biofilm formation by phenothiazine compounds. Microbiol Spectr. https://doi.org/10.1128/spectrum.01023-23
Rodrigues T (2023) Repositioning of antipsychotic phenothiazines for cancer therapy: nanotechnological opportunities to overcome obstacles. Curr Pharm Des 29(25):1959–1960. https://doi.org/10.2174/1381612829666230821092254
Patino I, Preuss C (2023) New drugs in synthesis research for tuberculosis. In: Shegokar R, Pathak Y (eds) Infectious diseases drug delivery systems. Springer International Publishing, Cham, pp 29–50. https://doi.org/10.1007/978-3-031-20521-7_2
Grimsey EM, Piddock LJV (2019) Do phenothiazines possess antimicrobial and efflux inhibitory properties? FEMS Microbiol Rev 43:577–590. https://doi.org/10.1093/femsre/fuz017
Poulsen MO, Jacobsen K, Thorsing M, Kristensen NR, Clasen J, Lillebaek EM, Skov MN, Kallipolitis BH, Kolmos HJ, Klitgaard JK (2013) Thioridazine potentiates the effect of a beta-lactam antibiotic against Staphylococcus aureus independently of mecA expression. Res Microbiol 164:181–188. https://doi.org/10.1016/j.resmic.2012.10.007
Rasmussen KS, Poulsen MO, Jacobsen K, Skov MN, Kolmos H, Kallipolitis BH, Klitgaard JK (2017) Combination of thioridazine and dicloxacillin as a possible treatment strategy of staphylococci. New Microbiol 40(2):146–147
Zhou H, Luan W, Wang Y, Song Y, Xu H, Tang X, Yu L (2022) The combination of cloxacillin, thioridazine and tetracycline protects mice against Staphylococcus aureus peritonitis by inhibiting α-Hemolysin-induced MAPK/NF-κB/NLRP3 activation. Int J Biol Macromol 198:1–10. https://doi.org/10.1016/j.ijbiomac.2021.12.112
Rodrigues L, Wagner D, Viveiros M, Sampaio D, Couto I, Vavra M, Kern WV, Amaral L (2008) Thioridazine and chlorpromazine inhibition of ethidium bromide efflux in Mycobacterium avium and Mycobacterium smegmatis. J Antimicrob Chemother 61:1076–1082. https://doi.org/10.1093/jac/dkn070
Boshoff HIM, Myers TG, Copp BR, McNeil MR, Wilson MA, Barry CE (2004) The transcriptional responses of Mycobacterium tuberculosis to inhibitors of metabolism. J Biol Chem 279:40174–40184. https://doi.org/10.1074/jbc.M406796200
Valıyeva G, Durupınar B, Coban AY (2023) Efflux pump effects on Mycobacterium tuberculosis drug resistance. J Chemother. https://doi.org/10.1080/1120009X.2023.2173857
Lo Presti MS, Bazán PC, Strauss M, Báez AL, Rivarola HW, Paglini-Oliva PA (2015) Trypanothione reductase inhibitors: overview of the action of thioridazine in different stages of Chagas disease. Acta Trop 145:79–87. https://doi.org/10.1016/j.actatropica.2015.02.012
Essodaïgui M, Frézard F, Moreira ES, Dagger F, Garnier-Suillerot A (1999) Energy-dependent efflux from Leishmania promastigotes of substrates of the mammalian multidrug resistance pumps. Mol Biochem Parasitol 100(1):73–84. https://doi.org/10.1016/s0166-6851(99)00036-5
Bodley AL, McGarry MW, Shapiro TA (1995) Drug cytotoxicity assay for African trypanosomes and Leishmania species. J Infect Dis 172(4):1157–1159. https://doi.org/10.1093/infdis/172.4.1157
He P, Li X, Guo X, Bian X, Wang R, Wang Y, Huang S, Qi M, Liu Y, Feng M (2023) Pharmacokinetics and pharmacodynamics of a novel vancomycin derivative LYSC98 in a murine thigh infection model against Staphylococcus aureus. Infect Drug Resist 18(16):1019–1028. https://doi.org/10.2147/IDR.S399150
Stat_Soft_Inc (2007) STATISTICA (data analysis software system), version 8.0. https://www.statsoft.com
Titus RG, Marchand M, Boon T, Louis JA (1987) A limiting dilution assay for quantifying Leishmania major in tissues of infected mice. Paras Immunol 7(5):545–555. https://doi.org/10.1111/j.1365-3024.1985.tb00098.x
U.S. National Library of Medicine (2023) LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [internet]. Drug Record: Thioridazine. Last updated July 1, 2020; retrieved 16 Mar 2023. https://www.ncbi.nlm.nih.gov/books/NBK548347/
Luo Y, Yu T, Li X, Qian G (2022) Thioridazine enhances cisplatin-induced DNA damage in cisplatin-resistant human lung cancer cells. Evid Based Complement Alternat Med 30:3702665. https://doi.org/10.1155/2022/3702665
Wang Y, Xia L, Lin J, Gong XY, Xu Y, Liu L, Bao J, Zhang C, Chai Y, Li H (2022) Thioridazine combined with carboplatin results in synergistic inhibition of triple negative breast cancer by targeting cancer stem cells. Transl Oncol 26:101549. https://doi.org/10.1016/j.tranon.2022.101549
Ahmadi F, Khalvati B, Eslami S, Mirzaii M, Roustaei N, Mazloomirad F, Khoramrooz SS (2022) The inhibitory effect of thioridazine on adeB efflux pump gene expression in multidrug-resistant Acinetobacter baumannii isolates using real time PCR. Avicenna J Med Biotechnol 14(2):132–136. https://doi.org/10.18502/ajmb.v14i2.8884
Adkin P, Hitchcock A, Smith LJ, Walsh SE (2022) Priming with biocides: a pathway to antibiotic resistance? J Appl Microbiol 133(2):830–841. https://doi.org/10.1111/jam.15564
Yuan W, Dong X, Chen L, Lei X, Zhou Z, Guo L, Wang J (2022) Screening for inhibitors against SARS-CoV-2 and its variants. Biosaf Health 4(3):186–192. https://doi.org/10.1016/j.bsheal.2022.05.002
- Feinberg SM, Fariba KA, Saadabadi A (2022) Thioridazine. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. [Updated 2022 May 2]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459140/
Reagan-Shaw S, Nihal M, Ahmad N (2008) Dose translation from animal to human studies revisited. FASEB J 22(3):659–661. https://doi.org/10.1096/fj.07-9574lsf
Potts RO, Guy RH (1992) Predicting skin permeability. Pharm Res 9:663–669. https://doi.org/10.1023/a:1015810312465
Wilschut A, ten Berge WF, Robinson PJ, McKone TE (1995) Estimating skin permeation. The validation of five mathematical skin permeation models. Chemosphere 30(7):1275–1296. https://doi.org/10.1016/0045-6535(95)00023-2
Frasch HF (2002) A random walk model of skin permeation. Risk Anal 22:265–276. https://doi.org/10.1111/0272-4332.00024
Ordway D, Viveiros M, Leandro C, Bettencourt R, Almeida J, Martins M, Kristiansen JE, Molnar J, Amaral L (2003) Clinical concentrations of thioridazine kill intracellular multidrug-resistant Mycobacterium tuberculosis. Antimicrob Agents Chemother 47(3):917–922. https://doi.org/10.1128/aac.47.3.917-922.2003
Thanacoody HKR (2007) Thioridazine: resurrection as an antimicrobial agent? Br J Clin Pharmacol 64(5):566–574. https://doi.org/10.1111/j.1365-2125.2007.03021.x
van Soolingen D, Hernandez-Pando R, Orozco H, Aguilar D, Magis-Escurra C, Amaral L, van Ingen J, Boeree MJ (2010) The antipsychotic thioridazine shows promising therapeutic activity in a mouse model of multidrug-resistant tuberculosis. PLoS ONE 5(9):e12640. https://doi.org/10.1371/journal.pone.0012640
Abbate E, Vescovo M, Natiello M, Cufré M, García A, Gonzalez PM, Ambroggi M, Ritacco V, van Soolingen D (2012) Successful alternative treatment of extensively drug-resistant tuberculosis in Argentina with a combination of linezolid, moxifloxacin and thioridazine. J Antimicrob Chemother 67(2):473–477. https://doi.org/10.1093/jac/dkr500
Dutta NK, Pinn ML, Karakousis PC (2014) Reduced emergence of isoniazid resistance with concurrent use of thioridazine against acute murine tuberculosis. Antimicrob Agents Chemother 58(7):4048–4053. https://doi.org/10.1128/aac.02981-14
Gutiérrez-Correa J (2006) Trypanosoma cruzi dihydrolipoamide dehydrogenase as target for phenothiazine cationic radicals. Effect of antioxidants Curr Drug Targets 7(9):1155–1179. https://doi.org/10.2174/138945006778226615
Gutierrez-Correa J, Fairlamb AH, Stoppani AO (2011) Trypanosoma cruzi trypanothione reductase is inactivated by peroxidase-generated phenothiazine cationic radicals. Free Radic Res 34(4):363–378. https://doi.org/10.1080/10715760100300311
Hajiagha MN, Kafil HS (2023) Efflux pumps and microbial biofilm formation. Infect Genet Evol. https://doi.org/10.1016/j.meegid.2023.105459
Ruth MM, Pennings LJ, Koeken VACM, Schildkraut JA, Hashemi A, Wertheim HFL, Hoefsloot W, van Ingen J (2020) Thioridazine is an efflux pump inhibitor in Mycobacterium avium complex but of limited clinical relevance. Antimicrob Agents Chemother 64(7):e00181–e0018120. https://doi.org/10.1128/AAC.00181-20
Acknowledgements
Special thanks to Daniel Andrés Sánchez Almaraz and Ofelia Pérez Olvera for their technical support.
Funding
Dirección General de Asuntos del Personal Académico,Universidad Nacional Autónoma de México, IN212422, María Magdalena Aguirre-García,CONACyT (MX), 284018, María Magdalena Aguirre-García.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by SSR, NM-D, LM-F and ARE-M. The first draft of the manuscript was written by SSR and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
This research was funded by the Secretaría de Educación Pública—Consejo Nacional de Ciencia y Tecnología (SEP-CONACyT, México), grant number 284018, and partially sponsored by the DGAPA-PAPIIT, grant number IN212422, given to María Magdalena Aguirre García. Sergio Sifontes Rodríguez was supported by a UNAM-DGAPA Postdoctoral fellowship 2021–2022 (Dirección General de Asuntos del Personal Académico, Universidad Nacional Autónoma de México).
Ethical Approval
The experimental protocol was approved by the Institutional Ethics Committee for the Care and Use of Laboratory Animals of the Center of Bioactive Chemicals (CBQ/CEAE/2021.4). All animal experiments complied with the ARRIVE guidelines and were carried out in accordance with the International Council for Laboratory Animal Science (ICLAS) ethical guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sifontes-Rodríguez, S., Mollineda-Diogo, N., Monzote-Fidalgo, L. et al. In Vitro and In Vivo Antileishmanial Activity of Thioridazine. Acta Parasit. 69, 324–331 (2024). https://doi.org/10.1007/s11686-023-00746-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11686-023-00746-2