Abstract
Background
The objective of this article is a review and an analysis of the current state of centralization of pancreatic surgery in Europe. Numerous recent publications demonstrate higher postoperative in-hospital mortality rates in low-volume clinics after pancreatic resection than previously assumed due to their not publishing significantly worse outcomes when compared to high-volume centres. Although the benefits of centralization of pancreatic surgery in high-volume centres have been demonstrated in many studies, numerous countries have so far failed to establish centralization in their respective health care systems.
Methods
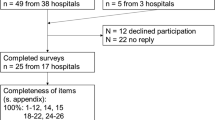
A systematic literature search of the Medline database for studies concerning centralization of pancreatic surgery in Europe was conducted. The studies were reviewed independently for previously defined inclusion and exclusion criteria. We included 14 studies with a total of 117,634 patients. All data were extracted from or provided by health insurance company or governmental registry databases.
Results
Thirteen out of the 14 studies demonstrate an improvement in their respective outcome related to volume. Twelve studies showed a significantly lower postoperative mortality rate in the highest annual volume group in comparison to overall postoperative mortality rate in the whole patient cohort.
Conclusion
As the available data indicate, most European countries have so far failed to establish centralization of pancreatic surgery to high-volume centres due to numerous reasons. Considering a plateau in survival rates of patients undergoing treatment for pancreatic cancer in Europe during the last 15 years, this review enforces the worldwide plea for centralization to lower post-operative mortality after pancreatic surgery.

Similar content being viewed by others
References
Ilic M, Ilic I. Epidemiology of pancreatic cancer. World J Gastroenterol 2016;22:9694–705. https://doi.org/10.3748/wjg.v22.i44.9694.
Allemani C, Matsuda T, Carlo VD, Harewood R, Matz M, Nikšić M, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 2018 https://doi.org/10.1016/S0140-6736(17)33326-3.
Doi R, Imamura M, Hosotani R, Imaizumi T, Hatori T, Takasaki K, et al. Surgery versus radiochemotherapy for resectable locally invasive pancreatic cancer: final results of a randomized multi-institutional trial. Surg Today 2008;38:1021–8. https://doi.org/10.1007/s00595-007-3745-8.
Büchler MW, Wagner M, Schmied BM, Uhl W, Friess H, Z’graggen K. Changes in morbidity after pancreatic resection: toward the end of completion pancreatectomy. Arch Surg Chic Ill 1960 2003;138:1310–4; discussion 1315. https://doi.org/10.1001/archsurg.138.12.1310.
Distler M, Rückert F, Hunger M, Kersting S, Pilarsky C, Saeger H-D, et al. Evaluation of survival in patients after pancreatic head resection for ductal adenocarcinoma. BMC Surg 2013;13:12. https://doi.org/10.1186/1471-2482-13-12.
Parikh P, Shiloach M, Cohen ME, Bilimoria KY, Ko CY, Hall BL, et al. Pancreatectomy risk calculator: an ACS-NSQIP resource. HPB 2010;12:488–97. https://doi.org/10.1111/j.1477-2574.2010.00216.x.
Uzunoglu FG, Reeh M, Vettorazzi E, Ruschke T, Hannah P, Nentwich MF, et al. Preoperative Pancreatic Resection (PREPARE) score: a prospective multicenter-based morbidity risk score. Ann Surg 2014;260:857–63; discussion 863-864. https://doi.org/10.1097/SLA.0000000000000946.
Grützmann R, Rückert F, Hippe-Davies N, Distler M, Saeger H-D. Evaluation of the International Study Group of Pancreatic Surgery definition of post-pancreatectomy hemorrhage in a high-volume center. Surgery 2012;151:612–20. https://doi.org/10.1016/j.surg.2011.09.039.
Keck T, Wellner UF, Bahra M, Klein F, Sick O, Niedergethmann M, et al. Pancreatogastrostomy Versus Pancreatojejunostomy for RECOnstruction After PANCreatoduodenectomy (RECOPANC, DRKS 00000767). Ann Surg 2016;263:440–9. https://doi.org/10.1097/SLA.0000000000001240.
Schmidt CM, Turrini O, Parikh P, House MG, Zyromski NJ, Nakeeb A, et al. Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Arch Surg Chic Ill 1960 2010;145:634–40. https://doi.org/10.1001/archsurg.2010.118.
Birkmeyer JD. Progress and challenges in improving surgical outcomes. Br J Surg 2012;99:1467–9. https://doi.org/10.1002/bjs.8933.
Luft HS, Bunker JP, Enthoven AC. Should operations be regionalized? The empirical relation between surgical volume and mortality. N Engl J Med 1979;301:1364–9. https://doi.org/10.1056/NEJM197912203012503.
Birkmeyer JD, Siewers AE, Finlayson EVA, Stukel TA, Lucas FL, Batista I, et al. Hospital Volume and Surgical Mortality in the United States. N Engl J Med 2002;346:1128–37. https://doi.org/10.1056/NEJMsa012337.
McPhee JT, Hill JS, Whalen GF, Zayaruzny M, Litwin DE, Sullivan ME, et al. Perioperative Mortality for Pancreatectomy. Ann Surg 2007;246:246–53. https://doi.org/10.1097/01.sla.0000259993.17350.3a.
Leapfrog. Leapfrog n.d. http://www.leapfroggroup.org/. Accessed January 22, 2018.
Milstein A, Galvin RS, Delbanco SF, Salber P, Buck CR. Improving the safety of health care: the leapfrog initiative. Eff Clin Pract ECP 2000;3:313–6.
Finks JF, Osborne NH, Birkmeyer JD. Trends in Hospital Volume and Operative Mortality for High-Risk Surgery. N Engl J Med 2011;364:2128–37. https://doi.org/10.1056/NEJMsa1010705.
Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Med Care 2011;49:1076–81. https://doi.org/10.1097/MLR.0b013e3182329b97.
Reames BN, Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital Volume and Operative Mortality in the Modern Era. Ann Surg 2014;260:244–51. https://doi.org/10.1097/SLA.0000000000000375.
Sahni NR, Dalton M, Cutler DM, Birkmeyer JD, Chandra A. Surgeon specialization and operative mortality in United States: retrospective analysis. BMJ 2016;354. https://doi.org/10.1136/bmj.i3571.
Kagedan DJ, Goyert N, Li Q, Paszat L, Kiss A, Earle CC, et al. The Impact of Increasing Hospital Volume on 90-Day Postoperative Outcomes Following Pancreaticoduodenectomy. J Gastrointest Surg Off J Soc Surg Aliment Tract 2017;21:506–15. https://doi.org/10.1007/s11605-016-3346-1.
Nimptsch U, Krautz C, Weber GF, Mansky T, Grützmann R. Nationwide In-hospital Mortality Following Pancreatic Surgery in Germany is Higher than Anticipated. Ann Surg 2016;264:1082–90. https://doi.org/10.1097/SLA.0000000000001693.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151:264–9, W64.
Tebé C, Pla R, Espinàs JA, Corral J, Puigdomenech E, Borràs JM, et al. Towards the centralization of digestive oncologic surgery: changes in activity, techniques and outcome. Rev Espanola Enfermedades Dig Organo Of Soc Espanola Patol Dig 2017;109:634–42. https://doi.org/10.17235/reed.2017.4710/2016.
Pérez-López P, Baré M, Touma-Fernández Á, Sarría-Santamera A. Relationship between volume and in-hospital mortality in digestive oncological surgery. Cirugia Espanola 2016;94:151–8. https://doi.org/10.1016/j.ciresp.2015.09.005.
Topal B, Van de Sande S, Fieuws S, Penninckx F. Effect of centralization of pancreaticoduodenectomy on nationwide hospital mortality and length of stay. Br J Surg 2007;94:1377–81. https://doi.org/10.1002/bjs.5861.
Güller U, Warschkow R, Ackermann CJ, Schmied BM, Cerny T, Ess S. Lower hospital volume is associated with higher mortality after oesophageal, gastric, pancreatic and rectal cancer resection n.d.. https://doi.org/10.4414/smw.2017.14473.
Skipworth RJE, Parks RW, Stephens NA, Graham C, Brewster DH, Garden OJ, et al. The relationship between hospital volume and post-operative mortality rates for upper gastrointestinal cancer resections: Scotland 1982–2003. Eur J Surg Oncol EJSO 2010;36:141–7. https://doi.org/10.1016/j.ejso.2009.10.004.
Balzano G, Zerbi A, Capretti G, Rocchetti S, Capitanio V, Di Carlo V. Effect of hospital volume on outcome of pancreaticoduodenectomy in Italy. Br J Surg 2008;95:357–62. https://doi.org/10.1002/bjs.5982.
Krautz C, Nimptsch U, Weber GF, Mansky T, Grützmann R. Effect of Hospital Volume on In-hospital Morbidity and Mortality Following Pancreatic Surgery in Germany. Ann Surg 2017. https://doi.org/10.1097/SLA.0000000000002248.
Pal N, Axisa B, Yusof S, Newcombe RG, Wemyss-Holden S, Rhodes M, et al. Volume and Outcome for Major Upper GI Surgery in England. J Gastrointest Surg 2008;12:353–7. https://doi.org/10.1007/s11605-007-0288-7.
van der Geest LGM, van Rijssen LB, Molenaar IQ, de Hingh IH, Groot Koerkamp B, Busch ORC, et al. Volume-outcome relationships in pancreatoduodenectomy for cancer. HPB 2016;18:317–24. https://doi.org/10.1016/j.hpb.2016.01.515.
Gooiker GA, Lemmens VEPP, Besselink MG, Busch OR, Bonsing BA, Molenaar IQ, et al. Impact of centralization of pancreatic cancer surgery on resection rates and survival. Br J Surg 2014;101:1000–5. https://doi.org/10.1002/bjs.9468.
Ahola R, Siiki A, Vasama K, Vornanen M, Sand J, Laukkarinen J. Effect of centralization on long-term survival after resection of pancreatic ductal adenocarcinoma. Br J Surg 2017;104:1532–8. https://doi.org/10.1002/bjs.10560.
Farges O, Bendersky N, Truant S, Delpero JR, Pruvot FR, Sauvanet A. The Theory and Practice of Pancreatic Surgery in France. Ann Surg 2017;266:797–804. https://doi.org/10.1097/SLA.0000000000002399.
Alsfasser G, Leicht H, Günster C, Rau BM, Schillinger G, Klar E. Volume-outcome relationship in pancreatic surgery. Br J Surg 2016;103:136–43. https://doi.org/10.1002/bjs.9958.
Derogar M, Blomberg J, Sadr-Azodi O. Hospital teaching status and volume related to mortality after pancreatic cancer surgery in a national cohort. Br J Surg 2015;102:548–57. https://doi.org/10.1002/bjs.9754.
van Heek NT, Kuhlmann KFD, Scholten RJ, de Castro SMM, Busch ORC, van Gulik TM, et al. Hospital volume and mortality after pancreatic resection: a systematic review and an evaluation of intervention in the Netherlands. Ann Surg 2005;242:781–8, discussion 788-790.
Gooiker GA, van Gijn W, Wouters MWJM, Post PN, van de Velde CJH, Tollenaar R EM, et al. Systematic review and meta-analysis of the volume-outcome relationship in pancreatic surgery. Br J Surg 2011;98:485–94. https://doi.org/10.1002/bjs.7413.
Krautz C, Denz A, Weber GF, Grützmann R. Influence of Hospital Volume Effects and Minimum Caseload Requirements on Quality of Care in Pancreatic Surgery in Germany. Visc Med 2017;33:131–4. https://doi.org/10.1159/000456042.
La Torre M, Nigri G, Ferrari L, Cosenza G, Ravaioli M. Hospital volume, margin status, and long-term survival after pancreaticoduodenectomy for pancreatic adenocarcinoma. Am Surg 2012;78:225–9.
Killeen SD, O’Sullivan MJ, Coffey JC, Kirwan WO, Redmond HP. Provider volume and outcomes for oncological procedures. Br J Surg 2005;92:389–402. https://doi.org/10.1002/bjs.4954.
Hata T, Motoi F, Ishida M, Naitoh T, Katayose Y, Egawa S, et al. Effect of Hospital Volume on Surgical Outcomes After Pancreaticoduodenectomy: A Systematic Review and Meta-analysis. Ann Surg 2016;263:664–72. https://doi.org/10.1097/SLA.0000000000001437.
Hidalgo M, Álvarez R, Gallego J, Guillén-Ponce C, Laquente B, Macarulla T, et al. Consensus guidelines for diagnosis, treatment and follow-up of patients with pancreatic cancer in Spain. Clin Transl Oncol 2017;19:667–81. https://doi.org/10.1007/s12094-016-1594-x.
Cronin-Fenton DP, Erichsen R, Mortensen FV, Dikinis S, Nørgaard M, Jacobsen J. Pancreatic cancer survival in central and northern Denmark from 1998 through 2009: a population-based cohort study. Clin Epidemiol 2011;3 Suppl 1:19–25. https://doi.org/10.2147/CLEP.S20611.
Storm HH, Gislum M, Engholm G. [Cancer survival before and after initiating the Danish Cancer Control plan]. Ugeskr Laeger 2008;170:3065–9.
Søreide JA, Sandvik OM, Søreide K. Improving pancreas surgery over time: Performance factors related to transition of care and patient volume. Int J Surg 2016;32:116–22. https://doi.org/10.1016/j.ijsu.2016.06.046.
Jonsdottir SB, Juliusson G, Kristinsson JÖ, Hreinsson JP, Jonasson JG, Björnsson ES. Incidence, diagnostic, treatment and outcome of patients diagnosed with cancer of the pancreas during 1986-2009: a population-based study. Scand J Gastroenterol 2018;53:100–6. https://doi.org/10.1080/00365521.2017.1390598.
Bramhall SR, Allum WH, Jones AG, Allwood A, Cummins C, Neoptolemos JP. Treatment and survival in 13,560 patients with pancreatic cancer, and incidence of the disease, in the West Midlands: an epidemiological study. Br J Surg 1995;82:111–5.
Watanapa P, Williamson RC. Surgical palliation for pancreatic cancer: developments during the past two decades. Br J Surg 1992;79:8–20.
Young J, Thompson A, Tait I, Waugh L, McPhillips G. Centralization of Services and Reduction of Adverse Events in Pancreatic Cancer Surgery. World J Surg 2013;37:2229–33. https://doi.org/10.1007/s00268-013-2108-4.
GDK - Schweizerische Konferenz der kantonalen Gesundheitsdirektorinnen und -direktoren: Hochspezialisierte Medizin n.d. https://www.gdk-cds.ch/index.php?id=822. Accessed January 30, 2018.
Gangl O, Sahora K, Kornprat P, Margreiter C, Primavesi F, Bareck E, et al. Preparing for Prospective Clinical Trials: A National Initiative of an Excellence Registry for Consecutive Pancreatic Cancer Resections. World J Surg 2014;38:456–62. https://doi.org/10.1007/s00268-013-2283-3.
Nienhuijs SW, Rutten HJT, Luiten EJT, van Driel OJR, Reemst PHM, Lemmens VEPP, et al. Reduction of in-hospital mortality following regionalisation of pancreatic surgery in the south-east of the Netherlands. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 2010;36:652–6. https://doi.org/10.1016/j.ejso.2010.05.008.
.Lemmens VEPP, Bosscha K, van der Schelling G, Brenninkmeijer S, Coebergh JWW, de Hingh IHJT. Improving outcome for patients with pancreatic cancer through centralization. Br J Surg 2011;98:1455–62. https://doi.org/10.1002/bjs.7581.
Gooiker GA, van der Geest LGM, Wouters MWJM, Vonk M, Karsten TM, Tollenaar RAEM, et al. Quality improvement of pancreatic surgery by centralization in the western part of the Netherlands. Ann Surg Oncol 2011;18:1821–9. https://doi.org/10.1245/s10434-010-1511-4.
de Wilde RF, Besselink MGH, van der Tweel I, de Hingh IHJT, van Eijck CHJ, Dejong CHC, et al. Impact of nationwide centralization of pancreaticoduodenectomy on hospital mortality. Br J Surg 2012;99:404–10. https://doi.org/10.1002/bjs.8664.
van der Geest LGM, Besselink MGH, Busch ORC, de Hingh IHJT, van Eijck CHJ, Dejong CHC, et al. Elderly Patients Strongly Benefit from Centralization of Pancreatic Cancer Surgery: A Population-Based Study. Ann Surg Oncol 2016;23:2002–9. https://doi.org/10.1245/s10434-016-5089-3.
van Rijssen LB, Koerkamp BG, Zwart MJ, Bonsing BA, Bosscha K, van Dam RM, et al. Nationwide prospective audit of pancreatic surgery: design, accuracy, and outcomes of the Dutch Pancreatic Cancer Audit. HPB 2017;19:919–26. https://doi.org/10.1016/j.hpb.2017.06.010.
Bassi C, Balzano G, Zerbi A, Ramera M. Pancreatic surgery in Italy. Criteria to identify the hospital units and the tertiary referral centers entitled to perform it. Updat Surg 2016;68:117–22. https://doi.org/10.1007/s13304-016-0371-2.
Maggino L, Vollmer CM. Recent Advances in Pancreatic Cancer Surgery. Curr Treat Options Gastroenterol 2017;15:520–37. https://doi.org/10.1007/s11938-017-0150-2.
Stella M, Bissolati M, Gentile D, Arriciati A. Impact of surgical experience on management and outcome of pancreatic surgery performed in high- and low-volume centers. Updat Surg 2017;69:351–8. https://doi.org/10.1007/s13304-017-0422-3.
Geraedts M, Kühnen C, Cruppé W de, Blum K, Ohmann C. [Hospitals failing minimum volumes in 2004: reasons and consequences]. Gesundheitswesen Bundesverb Arzte Offentlichen Gesundheitsdienstes Ger 2008;70:63–7. https://doi.org/10.1055/s-2007-1022522.
Jeganathan R, Kinnear H, Campbell J, Jordan S, Graham A, Gavin A, et al. A surgeon’s case volume of oesophagectomy for cancer does not influence patient outcome in a high volume hospital. Interact Cardiovasc Thorac Surg 2009;9:66–9. https://doi.org/10.1510/icvts.2008.195461.
Migliore M, Choong CK, Lim E, Goldsmith KA, Ritchie A, Wells FC. A surgeon’s case volume of oesophagectomy for cancer strongly influences the operative mortality rate. Eur J Cardiothorac Surg 2007;32:375–80. https://doi.org/10.1016/j.ejcts.2007.04.014.
Pecorelli N, Balzano G, Capretti G, Zerbi A, Di Carlo V, Braga M. Effect of surgeon volume on outcome following pancreaticoduodenectomy in a high-volume hospital. J Gastrointest Surg Off J Soc Surg Aliment Tract 2012;16:518–23. https://doi.org/10.1007/s11605-011-1777-2.
Mamidanna R, Ni Z, Anderson O, Spiegelhalter SD, Bottle A, Aylin P, et al. Surgeon Volume and Cancer Esophagectomy, Gastrectomy, and Pancreatectomy: A Population-based Study in England. Ann Surg 2016;263:727–32. https://doi.org/10.1097/SLA.0000000000001490.
Capretti G, Balzano G, Gianotti L, Stella M, Ferrari G, Baccari P, et al. Management and Outcomes of Pancreatic Resections Performed in High-Volume Referral and Low-Volume Community Hospitals Lead by Surgeons Who Shared the Same Mentor: The Importance of Training. Dig Surg 2018;35:42–8. https://doi.org/10.1159/000464412.
Lassen K, Coolsen MME, Slim K, Carli F, Aguilar-Nascimento JE de, Schäfer M, et al. Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin Nutr 2012;31:817–30. https://doi.org/10.1016/j.clnu.2012.08.011.
Vonlanthen R, Lodge P, Barkun JS, Farges O, Rogiers X, Soreide K, et al. Toward a Consensus on Centralization in Surgery. Ann Surg 2018;268:712–24. https://doi.org/10.1097/SLA.0000000000002965.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Polonski, A., Izbicki, J.R. & Uzunoglu, F.G. Centralization of Pancreatic Surgery in Europe. J Gastrointest Surg 23, 2081–2092 (2019). https://doi.org/10.1007/s11605-019-04215-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04215-y