Abstract
Background
Centralisation of highly specialised medicine (HSM) has changed practice and outcome in pancreatic surgery (PS) also in Switzerland. Fewer hospitals are allowed to perform pancreatic surgery according to nationally defined cut-offs.
Objective
We aimed to examine trends in PS in Switzerland. First, to assess opinions and expected trends among Swiss pancreatic surgeons in regard of PS practice and second, to assess the evolution of PS performance in Switzerland by a nationwide retrospective analysis.
Methods
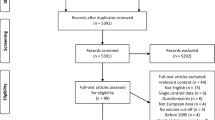
First, a 26-item survey among all surgeons who performed PS in 2016 in Switzerland was performed. Then, nationwide data from 1998 to 2018 from all hospitals performing PS was analysed including centre volume, perioperative morbidity and mortality, surgical indications and utilisation of minimally invasive pancreatic surgery (MIPS). The national cut-off for regulatory accredited volume centres (AVC) was ≥ 12. Additionally, an international benchmark definition for high volume (≥ 20 surgeries/year) was used.
Results
Among 25 surgeons from 15 centres (response rate 51%), the survey revealed agreement that centralisation is important to improve perioperative outcomes. Respondents agreed on a minimum case load per surgeon or centre. Within the nationwide database, 8534 pancreatic resections were identified. Most resections were performed for pancreatic ductal adenocarcinoma (58.9%). There was a significant trend towards centralisation of PS with fewer non-accredited volume centres (nAVC) (36 in 1998 and 17 in 2018, p < 0.001) and more AVC (2 in 1998 and 18 in 2018, p < 0.001). A significantly higher adjusted mortality after pancreatoduodenectomy (PD) was observed in low-volume compared to high-volume hospitals (OR 1.45 [95% CI 1.15–1.84], p = 0.002) and a similar trend compared among AVC and nAVC (OR 1.25 [95% CI 0.98–1.60], p = 0.072), while mortality after distal pancreatectomy (DP) was not influenced by centre volume.
Conclusions
Over the last two decades, centralisation of PS towards higher-volume centres was observed in Switzerland with a decrease of mortality after PD and low mortality after DP. Further centralisation is supported by most pancreatic surgeons. However, the ideal metric and outcome measures for the allocation of highly specialised medicine need further discussion to allow a fair and outcome-focused allocation.





Similar content being viewed by others
Data availability
The Swiss Federal Statistical Office’s (BFS, Neuchatel, Switzerland) databases covering the mandatory, nationwide reporting of all stationary hospitalisations (≥ 24 h) in Swiss hospitals starting from 1998 was used for the current analyses. These databases contain anonymised patient-level data including the main diagnosis responsible for hospitalisation and up to 49 secondary diagnoses for comorbidities and complications coded via International Classification of Diseases (ICD-10 German modification) definitions. Procedures are coded by national Swiss surgical classification codes (CHOP), issued annually by the BFS classifying all medical interventions. The national database covering hospitalisations is available from the BFS upon signature of a research and data protection agreement for a fee of 712 Swiss francs. All other data used in this study are freely available under the given links. All codes used for filtering, analyses and graphics are available from the first author upon reasonable request.
Code availability
Not applicable.
Abbreviations
- AVC:
-
Accredited volume centre
- CHOP:
-
Swiss classification of operations
- DP:
-
Distal pancreatectomy
- FSO:
-
Federal Statistical Office of Switzerland
- HSM:
-
Highly specialised medicine
- HVC:
-
High-volume centre
- ICD:
-
International Classification of Diseases
- IPMN:
-
Intraductal papillary mucinous neoplasms
- IQR:
-
Interquartile range
- LVC:
-
Low-volume centre
- MIPS:
-
Minimally invasive pancreatic surgery
- nAVC:
-
Non-accredited volume centre
- PD:
-
Pancreatoduodenectomy
- PROMs:
-
Patient-reported outcome measures
- PDAC:
-
Pancreatic ductal adenocarcinoma
- PS:
-
Pancreatic surgery
References
Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I et al (2002) Hospital volume and surgical mortality in the United States. N Engl J Med 346(15):1128–1137. https://doi.org/10.1056/NEJMsa012337
Birkmeyer JD, Finlayson SR, Tosteson AN, Sharp SM, Warshaw AL, Fisher ES (1999) Effect of hospital volume on in-hospital mortality with pancreaticoduodenectomy. Surgery 125(3):250–256. https://doi.org/10.1016/S0039-6060(99)70234-5
Krautz C, Nimptsch U, Weber GF, Mansky T, Grützmann R (2018) Effect of hospital volume on in-hospital morbidity and mortality following pancreatic surgery in Germany. Ann Surg 267(3):411–417. https://doi.org/10.1097/sla.0000000000002248
Ghadban T, Reeh M, Bockhorn M, Grotelueschen R, Bachmann K, Grupp K et al (2019) Decentralized colorectal cancer care in Germany over the last decade is associated with high in-hospital morbidity and mortality. Cancer Manag Res 11:2101–2107. https://doi.org/10.2147/cmar.S197865
Filmann N, Walter D, Schadde E, Bruns C, Keck T, Lang H et al (2019) Mortality after liver surgery in Germany. Br J Surg 106(11):1523–1529. https://doi.org/10.1002/bjs.11236
de Wilde RF, Besselink MG, van der Tweel I, de Hingh IH, van Eijck CH, Dejong CH et al (2012) Impact of nationwide centralization of pancreaticoduodenectomy on hospital mortality. Br J Surg 99(3):404–410. https://doi.org/10.1002/bjs.8664
Sheetz KH, Dimick JB, Nathan H (2019) Centralization of high-risk cancer surgery within existing hospital systems. J Clin Oncol 37(34):3234–3242. https://doi.org/10.1200/jco.18.02035
van Heek NT, Kuhlmann KF, Scholten RJ, de Castro SM, Busch OR, van Gulik TM et al (2005) Hospital volume and mortality after pancreatic resection: a systematic review and an evaluation of intervention in the Netherlands. Ann Surg. 242(6):781–788. https://doi.org/10.1097/01.sla.0000188462.00249.36 (discussion 8-90)
Gooiker GA, van Gijn W, Wouters MW, Post PN, van de Velde CJ, Tollenaar RA (2011) Systematic review and meta-analysis of the volume-outcome relationship in pancreatic surgery. Br J Surg 98(4):485–494. https://doi.org/10.1002/bjs.7413
Polonski A, Izbicki JR, Uzunoglu FG (2019) Centralization of pancreatic surgery in Europe. J Gastrointest Surg Off J Soc Surg Alimentary Tract 23(10):2081–2092. https://doi.org/10.1007/s11605-019-04215-y
Ahola R, Sand J, Laukkarinen J (2020) Centralization of pancreatic surgery improves results: review. Scand J Surg 109(1):4–10. https://doi.org/10.1177/1457496919900411
Vonlanthen R, Lodge P, Barkun JS, Farges O, Rogiers X, Soreide K et al (2018) Toward a consensus on centralization in surgery. Ann Surg 268(5):712–724. https://doi.org/10.1097/sla.0000000000002965
HSM-Fachorgan. Komplexe hochspezialisierte Viszeralchirurgie. Erläuternder Bericht für die Leistungszuteilung.: Konferenz der kantonalen Gesundheitsdirektorinnen und ‑direktoren (GDK); 2019.
Dudekula A, Munigala S, Zureikat AH, Yadav D (2016) Operative trends for pancreatic diseases in the USA: analysis of the nationwide inpatient sample from 1998–2011. J Gastrointest Surg Off J Soc Surg Alimentary Tract 20(4):803–811. https://doi.org/10.1007/s11605-015-3067-x
Liu R, Wakabayashi G, Palanivelu C, Tsung A, Yang K, Goh BKP et al (2019) International consensus statement on robotic pancreatic surgery. Hepatobiliary Surg Nutr 8(4):345–360. https://doi.org/10.21037/hbsn.2019.07.08
Cheng Y, Briarava M, Lai M, Wang X, Tu B, Cheng N et al (2017) Pancreaticojejunostomy versus pancreaticogastrostomy reconstruction for the prevention of postoperative pancreatic fistula following pancreaticoduodenectomy. Cochrane Database Syst Rev 12(9):CD012257. https://doi.org/10.1002/14651858.CD012257.pub2.
Lyu Y, Cheng Y, Wang B, Zhao S, Chen L.(2019) Peritoneal drainage or no drainage after pancreaticoduodenectomy and/or distal pancreatectomy: a meta-analysis and systematic review. Surg Endosc. https://doi.org/10.1007/s00464-019-07293-w.
Maggino L, Malleo G, Salvia R, Bassi C, Vollmer CM Jr (2019) Defining the practice of distal pancreatectomy around the world. HPB (Oxford) 21(10):1277–1287. https://doi.org/10.1016/j.hpb.2019.02.016
Bundesamt für Statistik (2020) Swiss surgical classification codes (CHOP). https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/nomenklaturen/medkk.html. Accessed 12 Oct 2021
Probst P, Hüttner FJ, Meydan Ö, Abu Hilal M, Adham M, Barreto SG et al (2021) Evidence map of pancreatic surgery-a living systematic review with meta-analyses by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 170(5):1517–1524. https://doi.org/10.1016/j.surg.2021.04.023
Kovoor JG, Ma N, Tivey DR, Vandepeer M, Jacobsen JHW, Scarfe A et al (2022) In-hospital survival after pancreatoduodenectomy is greater in high-volume hospitals versus lower-volume hospitals: a meta-analysis. ANZ J Surg 92(1–2):77–85. https://doi.org/10.1111/ans.17293
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36(1):8–27. https://doi.org/10.1097/00005650-199801000-00004
Baum P, Lenzi J, Diers J, Rust C, Eichhorn ME, Taber S et al (2022) Risk-adjusted mortality rates as a quality proxy outperform volume in surgical oncology-a new perspective on hospital centralization using national population-based data. J Clin Oncol 40(10):1041–1050. https://doi.org/10.1200/jco.21.01488
Casciani F, Trudeau MT, Asbun HJ, Ball CG, Bassi C, Behrman SW, et al. (2020) Surgeon experience contributes to improved outcomes in pancreatoduodenectomies at high risk for fistula development. Surgery. https://doi.org/10.1016/j.surg.2020.11.022.
Krautz C, Haase E, Elshafei M, Saeger HD, Distler M, Grützmann R et al (2019) The impact of surgical experience and frequency of practice on perioperative outcomes in pancreatic surgery. BMC Surg 19(1):108. https://doi.org/10.1186/s12893-019-0577-6
Strobel O, Neoptolemos J, Jäger D, Büchler MW (2019) Optimizing the outcomes of pancreatic cancer surgery. Nat Rev Clin Oncol 16(1):11–26. https://doi.org/10.1038/s41571-018-0112-1
El Amrani M, Clement G, Lenne X, Farges O, Delpero JR, Theis D et al (2018) Failure-to-rescue in patients undergoing pancreatectomy: is hospital volume a standard for quality improvement programs? Nationwide Analysis of 12,333 Patients. Ann Surg 268(5):799–807. https://doi.org/10.1097/sla.0000000000002945
Güller U, Warschkow R, Ackermann CJ, Schmied B, Cerny T, Ess S (2017) Lower hospital volume is associated with higher mortality after oesophageal, gastric, pancreatic and rectal cancer resection. Swiss Med Wkly. 147:w14473. https://doi.org/10.4414/smw.2017.14473
Cools KS, Sanoff HK, Kim HJ, Yeh JJ, Stitzenberg KB (2018) Impact of neoadjuvant therapy on postoperative outcomes after pancreaticoduodenectomy. J Surg Oncol 118(3):455–462. https://doi.org/10.1002/jso.25183
Marchegiani G, Andrianello S, Nessi C, Sandini M, Maggino L, Malleo G et al (2018) Neoadjuvant therapy versus upfront resection for pancreatic cancer: the actual spectrum and clinical burden of postoperative complications. Ann Surg Oncol 25(3):626–637. https://doi.org/10.1245/s10434-017-6281-9
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Sánchez-Velázquez P, Muller X, Malleo G, Park JS, Hwang HK, Napoli N et al (2019) Benchmarks in pancreatic surgery: a novel tool for unbiased outcome comparisons. Ann Surg 270(2):211–218. https://doi.org/10.1097/sla.0000000000003223
Wacker J, Zwahlen M (2019) Uncertain progress in Swiss perioperative mortality 1998–2014 for 22 operation groups. Swiss Med Wkly 149:w20034. https://doi.org/10.4414/smw.2019.20034
van Hilst J, de Rooij T, Bosscha K, Brinkman DJ, van Dieren S, Dijkgraaf MG et al (2019) Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol 4(3):199–207. https://doi.org/10.1016/s2468-1253(19)30004-4
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13. https://doi.org/10.1016/j.surg.2005.05.001
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M et al (2017) The 2016 update of the international study group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161(3):584–591. https://doi.org/10.1016/j.surg.2016.11.014
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ et al (2007) Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142(1):20–25. https://doi.org/10.1016/j.surg.2007.02.001
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR et al (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142(5):761–768. https://doi.org/10.1016/j.surg.2007.05.005
Halm EA, Lee C, Chassin MR (2002) Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med 137(6):511–520. https://doi.org/10.7326/0003-4819-137-6-200209170-00012
Glanville J, Paisley S (2010) Identifying economic evaluations for health technology assessment. Int J Technol Assess Health Care 26(4):436–440. https://doi.org/10.1017/s0266462310000991
Or Z, Renaud T. Is there a relationship between volume of activity and quality of care in France. http://www.irdes.fr/EspaceAnglais/Publications//Qes149.pdf. Accessed 15 Jan 2022
Universtiy Hospital Zurich (2022). Available from: https://www.outcome4medicine.ch/
Acknowledgements
We thank Christian Oberkofler and Philipp Müller, both Department of Surgery and Transplantation, University Hospital Zurich, for their help with the design and distribution of the survey.
Funding
This study was supported by the Swiss Pancreas Foundation.
Author information
Authors and Affiliations
Contributions
Study conception and design: Christoph Kuemmerli, Marcel Schneider, Mathias Worni, Martin Bolli and Dominique Birrer. Acquisition of data: Marcel Schneider, Christoph Kuemmerli and Dominique Birrer. Analysis and interpretation of data: all authors. Drafting of manuscript: Christoph Kuemmerli and Dominique Birrer. Critical revision of manuscript: all authors.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. According to the cantonal ethics committee (BASEC-Nr. Req-2020–00493) all criteria were met, and the waiver of consent granted.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kuemmerli, C., Schneider, M.A., Joliat, GR. et al. Trends in pancreatic surgery in Switzerland: a survey and nationwide analysis over two decades. Langenbecks Arch Surg 407, 3423–3435 (2022). https://doi.org/10.1007/s00423-022-02679-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02679-2