Abstract
Purpose
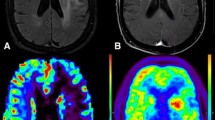
To evaluate reduced metabolism in the ipsilateral thalamus (TH) and/or contralateral cerebellum (CE) according to tumor localization and cortical metabolism around the tumor in patients with brain tumors based on FDG uptake.
Methods
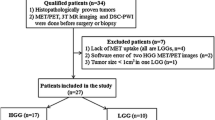
This study investigated 48 consecutive patients with solitary cerebral hemisphere parenchymal brain tumors who underwent PET/CT and MRI. Patients were divided into 4 groups (A: reduced uptake in ipsilateral TH and contralateral CE, B: reduced uptake in ipsilateral TH only, C: reduced uptake in contralateral CE only, and D: no reduced uptake in ipsilateral TH or contralateral CE). FDG uptake and MRI findings were compared among these groups.
Results
Of 48 patients, group A included 24 (50%), group B included 10 (21%), group C included 0, and group D included 14 (29%). No significant tendencies were observed between the groups regarding tumor localization. However, reduced cortical metabolism around the tumor was observed in 22 patients in group A, 7 patients in group B, and 1 patient in group D. All patients in group B showed reduced metabolism from around the tumor up to the ipsilateral TH.
Conclusion
Reduced FDG uptake in ipsilateral TH and contralateral CE usually occur simultaneously in patients with solitary brain tumors.







Similar content being viewed by others
References
Feeney DM, Baron JC. Diaschisis. Stroke. 1986;17:817–30.
Baron JC, Bousser MG, Comar D, Castaigne P. “Crossed cerebellar diaschisis” in human supratentorial brain infarction. Trans Am Neurol Assoc. 1981;105:459–61.
Kuhl DE, Phelps ME, Kowell AP, Metter EJ, Selin C, Winter J. Effects of stroke on local cerebral metabolism and perfusion: mapping by emission computed tomography of 18FDG and 13NH3. Ann Neurol. 1980;8:47–60.
Fujie W, Kirino T, Tomukai N, Iwasawa T, Tamura A. Progressive shrinkage of the thalamus following middle cerebral artery occlusion in rats. Stroke. 1990;21:1485–8.
Iizuka H, Sakatani K, Young W. Neural damage in the rat thalamus after cortical infarcts. Stroke. 1990;21:790–4.
Nagasawa H, Kogure K. Exo-focal postischemic neuronal death in the rat brain. Brain Res. 1990;524:196–202.
Tamura A, Kirino T, Sano K, Takagi K, Oka H. Atrophy of the ipsilateral substantia nigra following middle cerebral artery occlusion in the rat. Brain Res. 1990;510:154–7.
Kataoka K, Hayakawa T, Yamada K, Mushiroi T, Kuroda R, Mogami H. Neuronal network disturbance after focal ischemia in rats. Stroke. 1989;20:1226–35.
Nagasawa H, Kogure K, Fujiwara T, Itoh M, Ido T. Metabolic disturbances in exo-focal brain areas after cortical stroke studied by positron emission tomography. J Neurol Sci. 1994;123:147–53.
Ogawa T, Yoshida Y, Okudera T, Noguchi K, Kado H, Uemura K. Secondary thalamic degeneration after cerebral infarction in the middle cerebral artery distribution: evaluation with MR imaging. Radiology. 1997;204:255–62.
Patronas NJ, Di Chiro G, Smith BH, De La Paz R, Brooks RA, Milam HL, et al. Depressed cerebellar glucose metabolism in supratentorial tumors. Brain Res. 1984;291:93–101.
Calabria F, Schillaci O. Recurrent glioma and crossed cerebellar diaschisis in a patient examined with 18F-DOPA and 18F-FDG PET/CT. Clin Nucl Med. 2012;37:878–9.
Kajimoto K, Oku N, Kimura Y, Kato H, Tanaka MR, Kanai Y, et al. Crossed cerebellar diaschisis: a positron emission tomography study with L-[methyl-11C]methionine and 2-deoxy-2-[18F]fluoro-D-glucose. Ann Nucl Med. 2007;21:109–13.
Teoh EJ, Green AL, Bradley KM. Crossed cerebellar diaschisis due to cerebral diffuse large B cell lymphoma on 18F-FDG PET/CT. Int J Hematol. 2014;100:415–6.
Otte A, Roelcke U, von Ammon K, Hausmann O, Maguire RP, Missimer J, et al. Crossed cerebellar diaschisis and brain tumor biochemistry studied with positron emission tomography, [18F]fluorodeoxyglucose and [11C]methionine. J Neurol Sci. 1998;156:73–7.
Han S, Wang X, Xu K, Hu C. Crossed cerebellar diaschisis: three case reports imaging using a tri-modality PET/CT-MR system. Medicine. 2016;95:e2526.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Israel O, Delbeke D. Normal distribution, variants, pitfalls, and artifacts. In: Delbeke D, Israel O, editors. Hybrid PET/CT and SPECT/CT imaging. New York: Springer Science + Business; 2010. p. 35–96.
Brodal A. Cerebrocerebellar pathways. Anatomical data and some functional implications. Acta Neurol Scand Suppl. 1972;51:153–95.
Kang KM, Sohn CH, Kim BS, Kim YI, Choi SH, Yun TJ, et al. Correlation of asymmetry indices measured by arterial spin-labeling MR imaging and SPECT in patients with crossed cerebellar diaschisis. Am J Neuroradiol. 2015;36:1662–8.
Pantano P, Baron JC, Samson Y, Bousser MG, Derouesne C, Comar D. Crossed cerebellar diaschisis. Further studies. Brain. 1986;109:677–94.
Kushner M, Alavi A, Reivich M, Dann R, Burke A, Robinson G. Contralateral cerebellar hypometabolism following cerebral insult: a positron emission tomographic study. Ann Neurol. 1984;15:425–34.
Flint AC, Naley MC, Wright CB. Ataxic hemiparesis from strategic frontal white matter infarction with crossed cerebellar diaschisis. Stroke. 2006;37:e1–2.
Infeld B, Davis SM, Lichtenstein M, Mitchell PJ, Hopper JL. Crossed cerebellar diaschisis and brain recovery after stroke. Stroke. 1995;26:90–5.
Miyazawa N, Toyama K, Arbab AS, Koizumi K, Arai T, Nukui H. Evaluation of crossed cerebellar diaschisis in 30 patients with major cerebral artery occlusion by means of quantitative I-123 IMP SPECT. Ann Nucl Med. 2001;15:513–9.
Komaba Y, Mishina M, Utsumi K, Katayama Y, Kobayashi S, Mori O. Crossed cerebellar diaschisis in patients with cortical infarction: logistic regression analysis to control for confounding effects. Stroke. 2004;35:472–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
About this article
Cite this article
Iwasa, H., Murata, Y., Nishimori, M. et al. Remote effects in the ipsilateral thalamus and/or contralateral cerebellar hemisphere using FDG PET in patients with brain tumors. Jpn J Radiol 36, 303–311 (2018). https://doi.org/10.1007/s11604-018-0721-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-018-0721-8