Summary
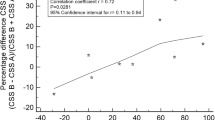
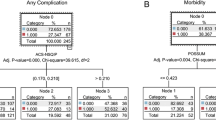
Although quality assessment is gaining increasing attention, there is still no consensus on how to define and grade postoperative complications. The absence of a definition and a widely accepted ranking system to classify surgical complications has hampered proper interpretation of the surgical outcome. This study aimed to define and search the simple and reproducible classification of complications following hepatectomy based on two therapy-oriented severity grading system: Clavien-Dindo classification of surgical complications and Accordion severity grading of postoperative complications. Two classifications were tested in a cohort of 2008 patients who underwent elective liver surgery at our institution between January 1986 and December 2005. Univariate and multivariate analyses were performed to link respective complications with perioperative parameters, length of hospital stay and the quality of life. A total of 1716 (85.46%) patients did not develop any complication, while 292 (14.54%) patients had at least one complication. According to Clavien-Dindo classification of surgical complications system, grade I complications occurred in 150 patients (7.47%), grade II in 47 patients (2.34%), grade IIIa in 59 patients (2.94%), grade IIIb in 13 patients (0.65%), grade IVa in 7 patients (0.35%), grade IVb in 1 patient (0.05%), and grade V in 15 patients (0.75%). According to Accordion severity grading of postoperative complications system, mild complications occurred in 160 patients (7.97%), moderate complications in 48 patients (2.39%), severe complications (invasive procedure/no general anesthesia) in 48 patients (2.39%), severe complications (invasive procedure under general anesthesia or single organ system failure) in 20 patients (1.00%), severe complications (organ system failure and invasive procedure under general anesthesia or multisystem organ failure) in 1 patient (0.05%), and mortality was 0.75% (n=15). Complication severity of Clavien-Dindo system and Accordion system were all correlated with the length of hospital stay, the number of hepatic segments resected, the blood transfusion and the Hospital Anxiety and Depression Scale-Anxiety (HADS-A). The Clavien-Dindo classification system and Accordion classification system are the simple ways of reporting all complications following the liver surgery.
Similar content being viewed by others
References
Andreou A, Vauthey JN, Cherqui D, et al. International Cooperative Study Group on Hepatocellular Carcinoma. Improved long-term survival after major resection for hepatocellular carcinoma: a multicenter analysis based on a new definition of major hepatectomy. J Gastrointest Surg, 2013,17(1):66–77
Jin S, Fu Q, Wuyun G, et al. Management of post-hepatectomy complications. World J Gastroenterol, 2013,19(44):7983–7991
Hardy KJ. Liver surgery: the past 2000 years. Aust N Z J Surg, 1990,60(10):811–817
Tanabe KK. The past 60 years in liver surgery. Cancer, 2008,113(7 Suppl):1888–1896
Ris F, Majno P, Morel P, et al. Complex liver resections: where are the limits? Rev Med Suisse (French), 2008,4(163):1558–1562
DeOliveira ML, Winter JM, Schafer M, et al. Assessment of complications after pancreatic surgery: A novel grading system applied to 633 patients undergoing pancreaticoduodenectomy. Ann Surg, 2006,244(6):931–937
Huang ZQ, Xu LN, Yang T, et al. Hepatic resection: an analysis of the impact of operative and perioperative factors on the morbidity and mortality rate. Chin Med J, 2009,122(19):2268–2277
Koch M, Garden OJ, Padbury R, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery, 2011,149(5):680–688
Mentula PJ, Leppäniemi AK. Applicability of the Clavien-Dindo classification to emergency surgical procedures: a retrospective cohort study on 444 consecutive patients. Patient Saf Surg, 2014,8(1):31
Porembka MR, Hall BL, Hirbe M, et al. Quantitative weighting of postoperative complications based on the accordion severity grading system: demonstration of potential impact using the american college of surgeons national surgical quality improvement program. J Am Coll Surg, 2010,210(3):286–298
Vollmer CM Jr, Lewis RS, Hall BL, et al. Establishing a quantitative benchmark for morbidity in pancreatoduodenectomy using ACS-NSQIP, the Accordion Severity Grading System, and the Postoperative Morbidity Index. Ann Surg, 2015,261(3):527–536
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg, 2004,240(2):205–213
Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Ann Surg, 2009,250(2):177–186
Strasberg SM, Hall BL. Postoperative morbidity index: a quantitative measure of severity of postoperative complications. J Am Coll Surg, 2011,213(5):616–626
de Vries EN, Prins HA, Crolla RM, et al. SURPASS Collaborative Group. Effect of a comprehensive surgical safety system on patient outcomes. N Engl J Med, 2010,363(20):1928–1937
Cescon M, Vetrone G, Grazi GL, et al. Trends in perioperative outcome after hepatic resection: analysis of 1500 consecutive unselected cases over 20 years. Ann Surg, 2009,249(6):995–1002
Yang T, Zhang J, Lu JH, et al. Risk factors influencing postoperative outcomes of major hepatic resection of hepatocellular carcinoma for patients with underlying liver diseases. World J Surg, 2011,35(9):2073–2082
Sajid MS, Iftikhar M, Rimple J, et al. Use of health-related quality of life tools in hepatobiliary surgery. Hepatobiliary Pancreat Dis Int, 2008,7(2):135–137
Gandhi S, Khubchandani S, Iyer R. Quality of life and hepatocellular carcinoma. J Gastrointest Oncol, 2014,5(4):296–317
dos Santos DC, Limongi V, de Oliveira da Silva AM, et al. Evaluation of functional status, pulmonary capacity, body composition, and quality of life of end-stage liver disease patients who are candidates for liver surgery. Transplant Proc, 2014,46(6):1771–1774
Toro A, Pulvirenti E, Palermo F, et al. Health-related quality of life in patients with hepatocellular carcinoma after hepatic resection, transcatheter arterial chemoembolization, radiofrequency ablation or no treatment. Surg Oncol, 2012, 21(1):e23–e30
Kamphues C, Engel S, Denecke T, et al. Safety of liver resection and effect on quality of life in patients with benign hepatic disease: single center experience. BMC Surg, 2011,11:16
Bruns H, Krätschmer K, Hinz U, et al. Quality of life after curative liver resection: a single center analysis. World J Gastroenterol 2010,16(19):2388–2395
Pritchard MJ. Using the hospital anxiety and depression scale in surgical patients. Nurs Stand, 2011,25(34):35–41
Fong TC, Ho RT. Factor analyses of the Hospital Anxiety and Depression Scale: a Bayesian structural equation modeling approach. Qual Life Res, 2013,22(10):2857–2863
Acknowledgements
We are deeply grateful to Ai-qun LI, Chong-hui LI, Li-jie GAO, Guang YANG, Zhen-yu ZHU, Han-sheng LIU, and Can-hong XIANG for their help in data collection.
Author information
Authors and Affiliations
Corresponding authors
Additional information
The authors contributed equally to this work.
Rights and permissions
About this article
Cite this article
Xu, Ln., Yang, B., Li, Gp. et al. Assessment of complications after liver surgery: Two novel grading systems applied to patients undergoing hepatectomy. J. Huazhong Univ. Sci. Technol. [Med. Sci.] 37, 352–356 (2017). https://doi.org/10.1007/s11596-017-1739-3
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-017-1739-3