Abstract
Objective
At present, there is no appropriate system to evaluate the severe complications of liver surgery through the preoperative factors. This study aimed to design and verify a risk assessment system for the prediction of severe post-operative complications after a hepatectomy based on the preoperative parameters.
Methods
A retrospective analysis was performed on 1732 patients who had undergone liver surgery. The severity of the complications was graded by Accordion Severity Grading of post-operative complications. The variables were screened by multivariate analysis, and graded scores were assigned to the selected variables. A logistic regression equation was used to form the liver operation risk formula (LORF) for the prediction of severe post-operative complications. The LORF was verified by the receiver operating characteristic (ROC) curve.
Results
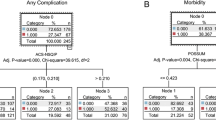
The multivariate correlation analysis revealed the independent influencing factors of the severe post-operative complications of liver surgery were Child-Pugh grade (OR=4.127; P<0.001), medical diseases requiring drug treatment (OR=3.092; P<0.001), the number of liver segments to be removed (OR=2.209; P=0.006), organ invasion (OR=4.538; P=0.024), and pathological type (OR=4.023; P=0.002). The binomial logistic regression model was established to obtain the calculation formula (LORF) of the severe complication risk. The area under the ROC curve (AUC) of the LORF was 0.815. The cut-off value of the expected probability of severe complications was 0.3225 (32.25%). Furthermore, in the validation data set, the corresponding AUC of the LORF was 0.829.
Conclusion
As a novel and simplified assessment system, the LORF could effectively predict the severe post-operative complications of liver surgery through the preoperative factors, and therefore it could be used to evaluate the risk of severe liver surgical complications before surgery.
Similar content being viewed by others
References
Agarwal V, Divatia JV. Enhanced recovery after surgery in liver resection: current concepts and controversies. Korean J Anesthesiol, 2019,72(2):119–129
Glantzounis GK, Karampa A, Peristeri DV, et al. Recent advances in the surgical management of hepatocellular carcinoma. Ann Gastroenterol, 2021,34(4):453–465
Marques HP, Barros I, Li J, et al. Current update in domino liver transplantation. Int J Surg, 2020,82S:163–168
Huang ZQ, Xu LN, Yang T, et al. Hepatic resection: an analysis of the impact of operative and perioperative factors on morbidity and mortality rates in 2008 consecutive hepatectomy cases. Chin Med J (Engl), 2009,122(19):2268–2277
Nanashima A, Tobinaga S, Abo T, et al. Reducing the incidence of post-hepatectomy hepatic complications by preoperatively applying parameters predictive of liver function. J Hepatobiliary Pancreat Sci, 2010,17(6):871–878
Chin KM, Allen JC, Teo JY, et al. Predictors of post-hepatectomy liver failure in patients undergoing extensive liver resections for hepatocellular carcinoma. Ann Hepatobiliary Pancreat Surg, 2018,22(3):185–196
Jackson NR, Hauch A, Hu T, et al. The safety and efficacy of approaches to liver resection: a meta-analysis. JSLS, 2015,19(1):e2014.00186
Yamazaki S, Takayama T. Current topics in liver surgery. Ann Gastroenterol Surg, 2019,3(2):146–159
Xu LN, Xu YY, Gao DW. Impact of operative and peri-operative factors on the long-term prognosis of primary liver cancer patients undergoing hepatectomy. J Huazhong Unrv Sci Technolog Med Sci, 2016,36(4):523–528
Chen L, Wang YB, Zhang YH, et al. Effective prediction of postoperative complications for patients after open hepatectomy: a simplified scoring system based on perioperative parameters. BMC Surg, 2019,19(1):128
Wang YK, Bi XY, Li ZY, et al. A new prognostic score system of hepatocellular carcinoma following hepatectomy. Zhonghua Zhong Liu Za Zhi (Chinese), 2017,39(12):903–909
Donadon M, Fontana A, Palmisano A, et al. Individualized risk estimation for postoperative morbidity after hepatectomy: the Humanitas score. HPB (Oxford), 2017,19(10):910–918
Xu LN, Yang B, Li GP, et al. Assessment of complications after liver surgery: Two novel grading systems applied to patients undergoing hepatectomy. J Huazhong Univ Sci Technolog Med Sci, 2017,37(3):352–356
Søreide JA, Deshpande R. Post hepatectomy liver failure (PHLF) — Recent advances in prevention and clinical management. Eur J Surg Oncol, 2021,47(2):216–224
Tomassini F, Giglio MC, De Simone G, et al. Hepatic function assessment to predict post-hepatectomy liver failure: what can we trust? A systematic review. Updates Surg, 2020,72(4):925–938
Rimini M, Rovesti G, Casadei-Gardini A. Child Pugh and ALBI grade: past, present or future? Ann Transl Med, 2020,8(17):1044
Russell MC. Complications following hepatectomy. Surg Oncol Clin N Am, 2015,24(1):73–96
Aucoin S, McIsaac DI. Emergency General Surgery in Older Adults: A Review. Anesthesiol Clin, 2019,37(3):493–505
Gillis C, Carli F. Promoting Perioperative Metabolic and Nutritional Care. Anesthesiology, 2015,123(6):1455–1472
Liu X, Yang Z, Tan H, et al. Characteristics and operative treatment of extremely giant liver hemangioma >20 cm. Surgery, 2017,161(6):1514–1524
Khan AS, Garcia-Aroz S, Ansari MA, et al. Assessment and optimization of liver volume before major hepatic resection: Current guidelines and a narrative review. Int J Surg, 2018,52:74–81
Cunningham AJ, Howell B, Polites S, et al. Establishing best practices for structured NSQIP review. Am J Surg, 2020,219(5):865–868
Sahara K, Paredes AZ, Merath K, et al. Evaluation of the ACS NSQIP Surgical Risk Calculator in Elderly Patients Undergoing Hepatectomy for Hepatocellular Carcinoma. J Gastrointest Surg, 2020,24(3):551–559
Acknowledgments
We thank Mrs. Ai-qun ZHANG for her assistance in the data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Xu, Ln., Xu, Yy., Li, Gp. et al. Establishment of an Assessment System for the Prediction of Severe Post-operative Complications after Hepatectomy Based on Preoperative Parameters. CURR MED SCI 42, 1088–1093 (2022). https://doi.org/10.1007/s11596-022-2629-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-022-2629-x