Abstract
Purpose
Multiple models have attempted to predict morbidity of liver resection (LR). This study aims to determine the efficacy of American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) surgical risk calculator and the Physiological and Operative Severity Score in the enUmeration of Mortality and Morbidity (POSSUM) in predicting post-operative morbidity in patients who underwent LR.
Methods
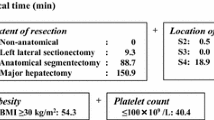
A retrospective analysis was conducted on patients who underwent elective LR. Morbidity risk was calculated with the ACS-NSQIP surgical risk calculator and POSSUM equation. Two models were then constructed for both ACS-NSQIP and POSSUM—(1) the original risk probabilities from each scoring system and (2) a model derived from logistic regression of variables. Discrimination, calibration, and overall performance for ACS-NSQIP and POSSUM were compared. Sub-group analysis was performed for both primary and secondary liver malignancies.
Results
Two hundred forty-five patients underwent LR. Two hundred twenty-three (91%) had malignant liver pathologies. The post-operative morbidity, 90-day mortality, and 30-day mortality rate were 38.3%, 3.7%, and 2.4% respectively. ACS-NSQIP showed superior discriminative ability, calibration, and performance to POSSUM (p = 0.03). Hosmer-Lemeshow plot demonstrated better fit of the ACS-NSQIP model than POSSUM in predicting morbidity.
Conclusion
In patients undergoing LR, the ACS-NSQIP surgical risk calculator was superior to POSSUM in predicting morbidity risk.


Similar content being viewed by others
References
Mirnezami R, Mirnezami A, Chandrakumaran K, Abu Hilal M, Pearce N, Primrose J et al (2011) Short- and long-term outcomes after laparoscopic and open hepatic resection: systematic review and meta-analysis. HPB 13(5):295–308. https://doi.org/10.1111/j.1477-2574.2011.00295.x
Shelat V, Serin K, Samim M, Besselink M, Al Saati H, Gioia P et al (2014) Outcomes of repeat laparoscopic liver resection compared to the primary resection. World J Surg 38(12):3175–3180. https://doi.org/10.1007/s00268-014-2728-3
Shelat V, Cipriani F, Basseres T, Armstrong T, Takhar A, Pearce N et al (2014) Pure laparoscopic liver resection for large malignant tumors: does size matter? Ann Surg Oncol 22:1288–1293
Tsao J, Loftus J, Nagorney D, Adson M, Ilstrup D (1994) Trends in morbidity and mortality of hepatic resection for malignancy. A matched comparative analysis. Ann Surg 220(2):199–205. https://doi.org/10.1097/00000658-199408000-00012
Jin S (2013) Management of post-hepatectomy complications. World J Gastroenterol 19(44):7983–7991. https://doi.org/10.3748/wjg.v19.i44.7983
Spolverato G, Ejaz A, Hyder O, Kim Y, Pawlik T (2014) Failure to rescue as a source of variation in hospital mortality after hepatic surgery. Br J Surg 101(7):836–846. https://doi.org/10.1002/bjs.9492
Birkmeyer N, Goodney P, Stukel T, Hillner B, Birkmeyer J (2005) Do cancer centers designated by the National Cancer Institute have better surgical outcomes? Cancer 103(3):435–441. https://doi.org/10.1002/cncr.20785
Zhu L, Li J, Dong X, Liu X, Bao Z, Feng J, Yu Y, Zhang Y, Wang Z, Wang Z (2011) Hospital costs and length of hospital stay for hepatectomy in patients with hepatocellular carcinoma: results of a prospective case series. Hepato-Gastroenterology 58(112):2052–2057. https://doi.org/10.5754/hge10149
Hsia CY, Chau GY, King KL, Loong CC, Lui WY, Wu CW (2003) Factors for prolonged length of stay after elective hepatectomy for hepatocellular carcinoma. The surgeon’s role in the managed care era. Hepato-Gastroenterology 50(51):798–804
Copeland G, Jones D, Walters M (1991) POSSUM: a scoring system for surgical audit. Br J Surg 78(3):355–360. https://doi.org/10.1002/bjs.1800780327
Wang H, Chen T, Wang H, Song Y, Li X, Wang J (2013) A systematic review of the Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity and its Portsmouth modification as predictors of post-operative morbidity and mortality in patients undergoing pancreatic surgery. Am J Surg 205(4):466–472. https://doi.org/10.1016/j.amjsurg.2012.06.011
Richards C, Leitch F, Horgan P, McMillan D (2010) A systematic review of POSSUM and its related models as predictors of post-operative mortality and morbidity in patients undergoing surgery for colorectal cancer. J Gastrointest Surg 14(10):1511–1520. https://doi.org/10.1007/s11605-010-1333-5
Dutta S, Horgan P, McMillan D (2010) POSSUM and its related models as predictors of postoperative mortality and morbidity in patients undergoing surgery for gastro-oesophageal cancer: a systematic review. World J Surg 34(9):2076–2082. https://doi.org/10.1007/s00268-010-0685-z
Chen T, Wang H, Wang H, Song Y, Li X, Wang J (2013) POSSUM and P-POSSUM as predictors of postoperative morbidity and mortality in patients undergoing hepato-biliary-pancreatic surgery: a meta-analysis. Ann Surg Oncol 20(8):2501–2510. https://doi.org/10.1245/s10434-013-2893-x
Schroeder R, Marroquin C, Bute B, Khuri S, Henderson W, Kuo P (2006) Predictive indices of morbidity and mortality after liver resection. Ann Surg 243(3):373–379. https://doi.org/10.1097/01.sla.0000201483.95911.08
Banz V, Studer P, Inderbitzin D, Candinas D (2009) Validation of the Estimation of Physiologic Ability and Surgical Stress (E-PASS) score in liver surgery. World J Surg 33(6):1259–1265. https://doi.org/10.1007/s00268-009-9989-2
Anbalakan K, Chua D, Pandya G, Shelat V (2015) Five year experience in management of perforated peptic ulcer and validation of common mortality risk prediction models—are existing models sufficient? A retrospective cohort study. Int J Surg 14:38–44. https://doi.org/10.1016/j.ijsu.2014.12.022
Mansmann U, Rieger A, Strahwald B, Crispin A (2016) Risk calculators—methods, development, implementation, and validation. Int J Color Dis 31(6):1111–1116. https://doi.org/10.1007/s00384-016-2589-3
Bilimoria K, Liu Y, Paruch J, Zhou L, Kmiecik T, Ko C et al (2013) Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg 217(5):833–842. https://doi.org/10.1016/j.jamcollsurg.2013.07.385
Edelstein A, Kwasny M, Suleiman L, Khakhkhar R, Moore M, Beal M et al (2015) Can the American College of Surgeons risk calculator predict 30-day complications after knee and hip arthroplasty? J Arthroplast 30(9):5–10. https://doi.org/10.1016/j.arth.2015.01.057
Rivard C, Nahum R, Slagle E, Duininck M, Isaksson Vogel R, Teoh D (2016) Evaluation of the performance of the ACS NSQIP surgical risk calculator in gynecologic oncology patients undergoing laparotomy. Gynecol Oncol 141(2):281–286. https://doi.org/10.1016/j.ygyno.2016.02.015
Lyle B, Landercasper J, Johnson J, Al-Hamadani M, Vang C, Groshek J et al (2016) Is the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator applicable for breast cancer patients undergoing breast-conserving surgery? Am J Surg 211(4):820–823. https://doi.org/10.1016/j.amjsurg.2015.07.013
Ford J, Coughlin K, Van Dorp D, Berri R (2015) Validation of the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) risk calculator to estimate serious complications in patients undergoing major gastrointestinal oncologic resection. J Am Coll Surg 221(4):e135–e136. https://doi.org/10.1016/j.jamcollsurg.2015.08.263
Yahya M, Blackwood S, Kontonicolas F, McGregor A, Fukumoto R, Dietzek A (2014) Accuracy of the NSQIP universal risk calculator using a vascular surgery cohort in a community teaching hospital. J Vasc Surg 60(3):822–823. https://doi.org/10.1016/j.jvs.2014.06.054
Zaydfudim V, Kerwin M, Turrentine F, Bauer T, Adams R, Stukenborg G (2016) The impact of chronic liver disease on the risk assessment of ACS NSQIP morbidity and mortality after hepatic resection. Surg 159(5):1308–1315. https://doi.org/10.1016/j.surg.2015.11.020
Older P, Hall A (2004) Clinical review: how to identify high-risk surgical patients. Crit Care 8(5):369–372. https://doi.org/10.1186/cc2848
Lau H, Man K, Fan S, Yu W, Lo C, Wong J (1997) Evaluation of preoperative hepatic function in patients with hepatocellular carcinoma undergoing hepatectomy. Br J Surg 84(9):1255–1259. https://doi.org/10.1002/bjs.1800840917
Vauthey J, Dixon E, Abdalla E, Helton W, Pawlik T, Taouli B et al (2010) Pretreatment assessment of hepatocellular carcinoma: expert consensus statement. HPB 12(5):289–299. https://doi.org/10.1111/j.1477-2574.2010.00181.x
Terminology Committee of the IHPBA (2000) Terminology of liver anatomy and resections. HPB 2:333–339
Dindo D, Demartines N, Clavien P (2004) Classification of surgical complications. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Søreide K, Kørner H, Søreide J (2011) Diagnostic accuracy and receiver-operating characteristics curve analysis in surgical research and decision making. Ann Surg 253(1):27–34. https://doi.org/10.1097/SLA.0b013e318204a892
Kass G (1980) An exploratory technique for investigating large quantities of categorical data. Appl Stat 29(2):119–127. https://doi.org/10.2307/2986296
Helling T, Blondeau B (2005) Anatomic segmental resection compared to major hepatectomy in the treatment of liver neoplasms. HPB 7(3):222–225. https://doi.org/10.1080/13651820510028828
Karanjia N, Lordan J, Quiney N, Fawcett W, Worthington T, Remington J (2009) A comparison of right and extended right hepatectomy with all other hepatic resections for colorectal liver metastases: a ten-year study. Eur J Surg Oncol 35(1):65–70. https://doi.org/10.1016/j.ejso.2007.12.002
Pitt H, Kilbane M, Strasberg S, Pawlik T, Dixon E, Zyromski N et al (2009) ACS-NSQIP has the potential to create an HPB-NSQIP option. HPB 11(5):405–413. https://doi.org/10.1111/j.1477-2574.2009.00074.x
Kuhan G, Abidia A, Wijesinghe L, Chetter I, Johnson B, Wilkinson A et al (2002) POSSUM and P-POSSUM overpredict mortality for carotid endarterectomy. Eur J Vasc Endovasc Surg 23(3):209–211. https://doi.org/10.1053/ejvs.2001.1557
Prytherch, Whiteley, Higgins, Weaver, Prout, Powell (1998) POSSUM and Portsmouth POSSUM for predicting mortality. Br J Surg 85(9):1217–1220. https://doi.org/10.1046/j.1365-2168.1998.00840.x
Leung E, Ferjani A, Stellard N, Wong L (2009) Predicting post-operative mortality in patients undergoing colorectal surgery using P-POSSUM and CR-POSSUM scores: a prospective study. Int J Color Dis 24(12):1459–1464. https://doi.org/10.1007/s00384-009-0781-4
Nagabhushan J, Srinath S, Weir F, Angerson W, Sugden B, Morran C (2007) Comparison of P-POSSUM and O-POSSUM in predicting mortality after oesophagogastric resections. Postgrad Med J 83(979):355–358. https://doi.org/10.1136/pgmj.2006.053223
Hyder J, Reznor G, Wakeam E, Nguyen L, Lipsitz S, Havens J (2016) Risk prediction accuracy differs for emergency versus elective cases in the ACS-NSQIP. Ann Surg 264(6):959–965. https://doi.org/10.1097/SLA.0000000000001558
Shubert C, Habermann E, Bergquist J, Thiels C, Thomsen K, Kremers W et al (2015) A NSQIP review of major morbidity and mortality of synchronous liver resection for colorectal metastasis stratified by extent of liver resection and type of colorectal resection. J Gastrointest Surg 19(11):1982–1994. https://doi.org/10.1007/s11605-015-2895-z
Markus P, Martell J, Leister I, Horstmann O, Brinker J, Becker H (2005) Predicting postoperative morbidity by clinical assessment. Br J Surg 92(1):101–106. https://doi.org/10.1002/bjs.4608
Woodfield J, Pettigrew R, Plank L, Landmann M, van Rij A (2007) Accuracy of the surgeons’ clinical prediction of perioperative complications using a visual analog scale. World J Surg 31(10):1912–1920. https://doi.org/10.1007/s00268-007-9178-0
Pettigrew R, Burns H, Carter D (1987) Evaluating surgical risk: the importance of technical factors in determining outcome. Br J Surg 74:791–794
Pettigrew R, Hill G (1986) Indicators of surgical risk and clinical judgement. Br J Surg 73(1):47–51. https://doi.org/10.1002/bjs.1800730121
Acknowledgements
The authors would like to thank Ms. Wang Bei for contributing to the data collection, Dr. Ma Thin Mar-Win for her preliminary organization and analysis of the data, and Dr. Chan Siew-Pang for his aid in the decision tree analysis.
Author information
Authors and Affiliations
Contributions
Sameer P. Junnarkar, Sudharsan Madhavan, Vishal G. Shelat, and Winston W.L. Woon participated in study conception and design. Sudharsan Madhavan and Su-Lin Soong participated in acquisition of data. Yiong H. Chan and Sudharsan Madhavan participated in analysis and interpretation of data. Sudharsan Madhavan and Vishal G. Shelat participated in drafting of the manuscript. Terence Huey and Sameer P. Junnarkar participated in critical revision of the manuscript.
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Permissions: All tables and figures are original works and have not been published elsewhere before.
Rights and permissions
About this article
Cite this article
Madhavan, S., Shelat, V.G., Soong, SL. et al. Predicting morbidity of liver resection. Langenbecks Arch Surg 403, 359–369 (2018). https://doi.org/10.1007/s00423-018-1656-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-018-1656-3