Abstract
Tear film thinning, hyperosmolarity, and breakup can cause irritation and damage to the human eye, and these form an area of active investigation for dry eye syndrome research. Recent research demonstrates that deficiencies in the lipid layer may cause locally increased evaporation, inducing conditions for breakup. In this paper, we explore the conditions for tear film breakup by considering a model for tear film dynamics with two mobile fluid layers, the aqueous and lipid layers. In addition, we include the effects of osmosis, evaporation as modified by the lipid, and the polar portion of the lipid layer. We solve the system numerically for reasonable parameter values and initial conditions and analyze how shifts in these cause changes to the system’s dynamics.














Similar content being viewed by others
References
Anonymous (2007) The definition and classification of dry eye disease. Ocul Surf 5(2):75–92
Aydemir E, Breward CJW, Witelski TP (2011) The effect of polar lipids on tear film dynamics. Bull Math Biol 73(6):1171–1201
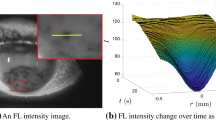
Begley CG, Simpson T, Liu H, Salvo E, Wu Z, Bradley A, Situ P (2013) Quantative analysis of tear film fluorescence and discomfort during tear film instability and thinning. Invest Ophthalmol Vis Sci 54:26452653
Benedetto DA, Clinch TE, Laibson PR (1986) In vivo observations of tear dynamics using fluorophotometry. Arch Ophthalmol 102:410–412
Berger RE, Corrsin S (1974) A surface tension gradient mechanism for driving the pre-corneal tear film after a blink. J Biomech 7:225–238
Bitton E, Lovasik JV (1998) Longitudinal analysis of precorneal tear film rupture patterns. In: Sullivan DA, Dartt DA, Meneray MA (eds) Advances in experimental medicine and biology, vol 438. Lacrimal gland, tear film, and dry eye syndromes 2. Springer, Berlin, pp 381–389
Braun RJ (2012) Dynamics of the tear film. Annu Rev Fluid Mech 44:267–297
Braun RJ, Gewecke NR, Begley CG, King-Smith PE, Siddique JI (2014) A model for tear film thinning with osmolarity and fluorescein. Invest Ophthalmol Vis Sci 55(2):1133
Braun RJ, King-Smith PE, Begley CG, Li L, Gewecke NR (2015) Dynamics and function of the tear film in relation to the blink cycle. Prog Ret Eye Res 45:132–164
Braun RJ, Driscoll TA, Begley CG, King-Smith PE, Siddique JI (2017) On tear film breakup (TBU): Dynamics and imaging. Math Med Biol. doi:10.1093/imammb/dqw023
Bron AJ, Tiffany JM, Gouveia SM, Yokoi N, Voon LW (2004) Functional aspects of the tear film lipid layer. Exp Eye Res 78(3):347–360
Bruna M, Breward CJW (2014) The influence of non-polar lipids on tear film dynamics. J Fluid Mech 746:565–605
Buck AL (1981) New equations for computing vapor pressure and enhancement factor. J Appl Meteorol 20(12):1527–1532
Cerretani CF, Radke CJ (2014) Tear dynamics in healthy and dry eyes. Curr Eye Res 39:580–595
Cerretani CF, Ho NH, Radke CJ (2013) Water-evaporation reduction by duplex films: application to the human tear film. Adv Colloid Interface Sci 197:33–57
Craster RV, Matar OK (2009) Dynamics and stability of thin liquid films. Rev Mod Phys 81(3):1131
Doane MG (1981) Blinking and the mechanics of the lacrimal drainage system. Ophthalmology 88:844–51
Doane MG (1989) An instrument for in vivo tear film interferometry. Optom Vis Sci 66:383–388
Gilbard JP, Farris RL II, Santamaria J (1978) Osmolarity of tear microvolumes in keratoconjunctivitis sicca. Arch Ophthalmol 96:677–681
Gipson IK (2004) Distribution of mucins at the ocular surface. Exp Eye Res 78(3):379–388
Goto E, Tseng SCG (2003) Kinetic analysis of tear interference images in aqueous tear deficiency dry eye before and after punctal occlusion. Invest Ophthalmol Vis Sci 44:1897–1905
Govindarajan B, Gipson IK (2010) Membrane-tethered mucins have multiple functions on the ocular surface. Exp Eye Res 90(6):655–663
Hogan MJ, Alvarado JA, Weddell JE (1971) Histology of the human eye. An atlas and textbook. W. B.Saunders, Philadelphia
Jones MB, McElwain DLS, Fulford GR, Collins MJ, Roberts AP (2006) The effect of the lipid layer on tear film behavior. Bull Math Biol 68:1355–1381
Kimball SH, King-Smith PE, Nichols JJ (2010) Evidence for the major contribution of evaporation to tear film thinning between blinks. Invest Opthalmol Vis Sci 51:6294–6297
King-Smith PE, Fink B, Hill R, Koelling K, Tiffany JM (2004) The thickness of the tear film. Curr Eye Res 29(4–5):357–368
King-Smith PE, Fink BA, Nichols JJ, Nichols KK, Braun RJ, McFadden GB (2009) The contribution of lipid layer movement to tear film thinning and breakup. Invest Ophthalmol Vis Sci 50:2747–2756
King-Smith PE, Hinel EA, Nichols JJ (2010) Application of a novel interferometric method to investigate the relation between lipid layer thickness and tear film thinning. Invest Ophthalmol Vis Sci 51(5):2418–2423
King-Smith PE, Nichols JJ, Nichols KK, Braun RJ (2011) A high resolution microscope for imaging the lipid layer of the tear film. Ocul Surf 9(4):197–211
King-Smith PE, Bailey MD, Braun RJ (2013a) Four characteristics and a model of an effective tear film lipid layer (TFLL). Ocul Surf 11(4):236–245
King-Smith PE, Ramamoorthy P, Braun RJ, Nichols JJ (2013b) Tear film images and breakup analyzed using fluorescent quenching. Invest Ophthalmol Vis Sci 54:6003–6011
King-Smith PE, Reuter KS, Braun RJ, Nichols JJ, Nichols KK (2013c) Tear film breakup and structure studied by simultaneous video recording of fluorescence and tear film lipid layer, TFLL, images. Invest Ophthalmol Vis Sci 54(7):4900–4909
Leiske DL, Leiske CI, Leiske DR, Toney MF, Senchyna M, Ketelson HA, Meadows DL, Fuller GG (2011) Temperature-induced transitions in the structure and interfacial rheology of human meibum. Biophys J 102:369–376
Leiske DL, Miller CE, Rosenfeld L, Cerretani C, Ayzner A, Lin B, Meron M, Senchyna M, Ketelson HA, Meadows D, Srinivasan S, Jones L, Radke CJ, Toney MF, Fuller GG (2012) Molecular structure of interfacial human meibum films. Langmuir 28:11858–11865
Lemp MA, Bron AJ, Baudouin C, del Castillo JMB, Geffen D, Tauber J, Foulks GN, Pepose JS, Sullivan BD (2011) Tear osmolarity in the diagnosis and management of dry eye disease. Am J Ophthalmol 151(5):792–798
Li L, Braun RJ, Maki KL, Henshaw WD, King-Smith PE (2014) Tear film dynamics with evaporation, wetting, and time-dependent flux boundary condition on an eye-shaped domain. Phys Fluids 26(5):052101
Li L, Braun RJ, Driscoll TA, Henshaw WD, Banks JW, King-Smith PE (2016) Computed tear film and osmolarity dynamics on an eye-shaped domain. Math Med Biol 33:123–157
Liu H, Begley CG, Chalmers R, Wilson G, Srinivas SP, Wilkinson JA (2006) Temporal progression and spatial repeatability of tear breakup. Optom Vis Sci 83(10):723–730
Liu H, Begley C, Chen M, Bradley A, Bonanno J, McNamara NA, Nelson JD, Simpson T (2009) A link between tear instability and hyperosmolarity in dry eye. Invest Ophthalmol Vis Sci 50(8):3671–3679
Matar OK, Craster RV, Warner MRE (2002) Surfactant transport on highly viscous surface films. J Fluid Mech 466:85–111
Mishima S, Maurice DM (1961) The oily layer of the tear film and evaporation from the corneal surface. Exp Eye Res 1:39–45
Montés-Micó R, Cervino A, Ferrer-Blasco T, García-Lázaro S, Madrid-Costa D (2010) The tear film and the optical quality of the eye. Ocul Surf 8(4):185–192
Nagyova B, Tiffany JM (1999) Components responsible for the surface tension of human tears. Curr Eye Res 19(1):4–11
Naire S, Braun RJ, Snow SA (2000) Limiting cases of gravitational drainage of a vertical free film for evaluating surfactants. SIAM J Appl Math 61:889913
Nichols B, Dawson CR, Togni B (1983) Surface features of the conjunctiva and cornea. Invest Ophthalmol Vis Sci 24(5):570–576
Nichols JJ, King-Smith PE, Hinel EA, Thangavelu M, Nichols KK (2012) The use of fluorescent quenching in studying the contribution of evaporation to tear thinning. Invest Ophthalmol Vis Sci 53:54265432
Norn MS (1969) Dessication of the precorneal film I. Corneal wetting time. Acta Ophthalmol 4:865–880
Oron A, Davis SH, Bankoff SG (1997) Long-scale evolution of thin liquid films. Rev Mod Phys 69(3):931
Owens H, Phillips J (2001) Spreading of the tears after a blink: velocity and stabilization time in healthy eyes. Cornea 20:484–487
Peng C, Cerretani C, Braun RJ, Radke CJ (2014) Evaporation-driven instability of the precorneal tear film. Adv Colloid Interface Sci 206:250–264
Riquelme R, Lira I, Pérez-López C, Rayas JA, Rodríguez-Vera R (2007) Interferometric measurement of a diffusion coefficient: comparison of two methods and uncertainty analysis. J Phys D Appl Phys 40(9):2769
Rosenfeld L, Cerretani C, Leiske DL, Toney MF, Radke CJ, Fuller GG (2013) Structural and rheological properties of meibomian lipid. Invest Ophthalmol Vis Sci 54:2720–2732
Sharma A (1998) Surface-chemical pathways of the tear film breakup. In: Sullivan DA, Dartt DA, Meneray MA (eds) Advances in experimental medicine and biology, vol 438. Lacrimal Gland, Tear Film, and Dry Eye Syndromes 2. Springer, Berlin, pp 361–370
Sharma A, Ruckenstein E (1985) Mechanism of tear film rupture and formation of dry spots on cornea. J Colloid Interface Sci 106(1):12–27
Siddique JI, Braun RJ (2015) Tear film dynamics with evaporation, osmolarity and surfactant transport. Appl Math Model 39:255–269
Stebe KJ, Maldarelli C (1994) Remobilizing surfactant retarded fluid particle interfaces: II. Controlling the surface mobility at interface of solutions containing surface active components. J Colloid Interface Sci 163:177–189
Tietz NW (1995) Clinical guide to laboratory tests. W. B. Saunders, Philadelphia
Tiffany JM (1987) The lipid secretion of the meibomian glands. Adv Lipid Res 22(1):1–62
Tiffany JM (1991) The viscosity of human tears. Int Ophthalmol 15(6):371–376
Tomlinson A, Khanal S, Ramaesh K, Diaper C, McFadyen A (2006) Tear film osmolarity: determination of a referent for dry eye diagnosis. Invest Ophthalmol Vis Sci 47(10):4309–4315
Tomlinson A, Doane MG, McFayden A (2009) Inputs and outputs of the lacrimal system: review of production and evaporative loss. Ocul Surf 7:17–29
Trefethen LN (2000) Spectral methods in MATLAB. SIAM, Philadelphia
Weast RC (ed) (1977) CRC handbook of chemistry and physics, 58th edn. Chemical Rubber Company, West Palm Beach
Yanez-Soto B, Mannis MJ, Schwab IR, Li JY, Leonard BC, Abbott NL, Murphy CJ (2014) Interfacial phenomena and the ocular surface. Ocul Surf 12:178–201
Yokoi N, Georgiev GA (2013a) Tear dynamics and dry eye disease (Chapter 7). In: Benitez del Castilo JM, Lemp MA (eds) Ocular surface disorders. JP Medical Ltd., London, pp 47–54
Yokoi N, Georgiev GA (2013b) Tear-film-oriented diagnosis and therapy for dry eye. In: Dry eye syndrome: basic and clinical perspectives, pp 96–108
Yokoi N, Takehisa Y, Kinoshita S (1996) Correlation of tear lipid layer interference patterns with the diagnosis and severity of dry eye. Am J Ophthalmol 122:818824
Zhong L, Ketelaar C, Braun RJ, King-Smith PE, Begley CG (2017) A mathematical model for glob-driven tear break up (TBU) (submitted)
Zubkov VS, Breward CJ, Gaffney EA (2012) Coupling fluid and solute dynamics within the ocular surface tear film: a modelling study of black line osmolarity. Bull Math Biol 74:2062–2093
Acknowledgements
This work was supported by National Science Foundation Grant DMS 1412085 (MS, RJB, PEKS). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NSF.
Author information
Authors and Affiliations
Corresponding author
Appendix A
Appendix A
1.1 A.1 Fluid Model Derivation
The derivation for this fluid model follows closely to the work of Bruna and Breward (2014), while making use of lubrication theory techniques covered in a different context in Oron et al. (1997) and Craster and Matar (2009). We let numerical subscripts indicate the domain we are working in, or the surface we are considering, with \(j=1\) corresponding to the aqueous domain, and \(j=2\) corresponding to the lipid domain. We let \(\mathbf {s}_{j}\) be the position on the upper interface of domain j, with corresponding unit normal and tangential vectors \(\hat{n}_{j}\) and \(\hat{t}_j\). We use letter subscripts x and t to indicate derivatives with respect to those variables.
At the aqueous–corneal interface, mass conservation and velocity continuity require the velocity is equal to the flux of water through the boundary from osmosis.
Inside the aqueous domain, we conserve mass and momentum, and so we use the incompressible Navier–Stokes equation.
At the aqueous–lipid boundary, velocity continuity requires that the horizontal aqueous and lipid velocities be equal. Meanwhile, the difference between a fluid’s velocity, \(\mathbf {u}_{j}\), and the velocity of the film’s surface, \(\mathbf {s}_{jt}(x)\), determines the mass flux through that surface. The position of the surface is governed by its movement due to surface forces, requiring a balance between the aqueous and lipid stresses with the effects of surface tension. Note that the surface tension at the aqueous–lipid boundary may vary.
As with the aqueous domain, we use the incompressible Navier–Stokes equation to govern the lipid domain.
At the lipid–air interface, we have no mass flux, and so the fluid velocity must equal the surface velocity. For surface forces, surface stress must balance with the effects of surface tension, but unlike the aqueous–lipid boundary, we will take this surface tension to be a constant, \(\gamma _2\).
In addition to the usual fluid dynamics, we will require several additional equations governing the transport and effects of surfactants in the polar portion of the lipid, the transport of salts in the aqueous domain, evaporation, and osmosis. The polar portion of the lipid acts as a surfactant with a linear reduction from the base surface tension, and we take the concentration of these surfactants to be governed by advection–diffusion along the surface of the aqueous–lipid interface, where \(\partial _{s_1}\) in Equation (24) indicates a derivative taken along the \(\mathbf {s}_1\) surface.
Salts are transported in the aqueous layer according to the advection diffusion equation. For no salt flux conditions at the top and aqueous–lipid and corneal interfaces, we require the salts transported away from the boundary by diffusion to equal those incident by advection.
Derivation for the evaporation model is given extensively in Appendix A.3. Lastly, osmotic flux is determined by the concentration difference between the aqueous layer and the cornea.
1.2 A.2 Reduction by Lubrication Theory
In order to drastically simplify this system, we will be applying the methods of lubrication theory, reducing this system as much as possible to leading-order terms in this thin film parameter \(\displaystyle ~\epsilon ~=~\frac{H_1}{L}~\ll ~1\). We will dimensionally scale this system, define all relevant parameters, expand the velocities in orders of \(\epsilon ^2\),
and finally group in orders of \(\epsilon ^2\). The dimensional scalings are given below. We assume the lipid viscosity is much larger than the aqueous viscosity (Rosenfeld et al. 2013). This requires a different pressure scales in the two layers, and establishes a shear balance in the aqueous layer and an extensional balance in the lipid layer at leading order.
\(x^* \rightarrow L x\) | \(h_1^* \rightarrow \epsilon L h_1\) | \(h_2^* \rightarrow \delta \epsilon L h_2\) |
\(y^* \rightarrow \epsilon L y\) | \(u_1^* \rightarrow U u_1\) | \(u_2^* \rightarrow U u_2\) |
\(\displaystyle t^* \rightarrow \frac{L}{U} t\) | \(v_1^* \rightarrow \epsilon U v_1\) | \(v_2^* \rightarrow \epsilon U v_2\) |
\(J^* \rightarrow \rho _1 \epsilon U J\) | \(\displaystyle p_1^* \rightarrow \frac{\mu _1 U}{\epsilon ^2 L} p_1\) | \(\displaystyle p_2^* \rightarrow \frac{\mu _2 U}{L} p_2\) |
\(\varGamma ^* \rightarrow \varGamma _0 \varGamma \) |
The parameters chosen are based on commonly used fluids parameters. We require our nondimensional parameters be on the order of 1 in comparison to \(\epsilon \), and so we include factors of \(\epsilon \) to keep the parameters near unit sized. The parameters are defined below.
\(\displaystyle \epsilon = \frac{H_1}{L}\) | \(\displaystyle \mathcal {C}_1 = \epsilon ^3 \frac{\gamma _1}{\mu _1 U}\) | \(\displaystyle \mathrm{Pe}_1 = \frac{UL}{D_1}\) |
\(\displaystyle \delta = \frac{H_2}{H_1}\) | \(\displaystyle \mathcal {C}_2 = \epsilon \frac{ \gamma _2}{\mu _2 U}\) | \(\displaystyle \mathrm{Pe}_2 = \frac{UL}{D_2}\) |
\(\displaystyle \varUpsilon = \epsilon ^2 \frac{\mu _2}{\mu _1}\) | \(\displaystyle \mathrm {Re}_1 = \frac{\rho _1 U L}{\mu _1}\) | \(\displaystyle \mathcal {E} = \frac{k_m}{\epsilon \rho _1 U} \frac{M_1}{R} \left( \frac{p_0}{T_0} - \frac{ R_h p_\infty }{T_\infty } \right) \) |
\(\displaystyle \mathcal {M} = \epsilon \frac{RT \varGamma _0}{\mu _1 U}\) | \(\displaystyle \mathcal {R}_2 = \epsilon ^{-2} \frac{\rho _2 U L}{\mu _2}\) | \(\displaystyle \mathcal {R} = \frac{k_m H_2}{Dk}\) |
\(\displaystyle \mathcal {P} = \frac{C P_c}{\epsilon U}\). |
After performing the above substitutions, expanding via perturbation theory, and grouping at leading orders, the number of terms in each of these equations is greatly reduced. We may now summarize these more simplified equations by region.
At the corneal–aqueous interface, we have
Inside the aqueous layer,
At the aqueous–lipid interface,
Inside the lipid layer,
At the lipid–air interface,
The leading-order equations governing salt transport are given by
And for auxiliary equations,
Lastly, we require second-order terms to determine the velocity of the lipid layer extensional flow as well as the salt transport equations. The second-order lipid layer equations, with corresponding variable \(u_2^{(2)}\), are given by
The second-order equations for salt transport, with corresponding variable \(c^{(2)}\), are given by
Next, we apply the methods of lubrication theory, with a shear balance in the aqueous layer and an extensional balance in the lipid, in order to eliminate the vertical dimension in this problem, giving us this system to be modeled. After significant algebraic manipulation, this system simplifies to an evolution equation for aqueous thickness, an evolution equation for lipid thickness, a transport equation for salt concentration, a transport equation for surfactants, and an extensional equation that determines the horizontal lipid velocity. This system is given by
The above system contains a few direct equations which have been left to improve the system’s readability.
1.3 A.3 Evaporation Model Derivation
For evaporation, we use a modified boundary layer model where mass transfer is driven by the chemical potential difference across the liquid gas interface, as expressed by a concentration difference.
Here, k is a kinetic mass transfer coefficient. We may then use the molar mass M to convert to molar concentration to partial pressure via the ideal gas law. This results in the mass flux equation
where subscripts 0 and \(\infty \) correspond to liquid and gas, respectively. Next, we then express \(p_0\) and \(p_\infty \) more naturally in terms of saturation vapor pressure. The liquid water layer will be at saturation vapor pressure, while the water vapor pressure \(p_0\) is expressed by the saturation vapor pressure and relative humidity \(R_h\). We use the saturation vapor pressure model given in Buck (1981) to express saturation vapor pressure p(T).
For calculating saturation vapor pressure, we use the values chosen in Buck (1981) for environmental conditions closest to our simulations.
Based on the values given in Buck (1981), the input temperature is in C, while the output pressure is in Pa. Lastly, we modify this boundary layer model by altering the boundary layer resistance to include a second layer, representing the resistance to permeation applied by the lipid layer in series with the evaporative resistance. As is done in Bruna and Breward (2014), Cerretani et al. (2013), Peng et al. (2014), we assign the lipid layer a resistance based on its thickness and permeability (given by Dk),
Many models simplify this one step further, grouping \(k_m\) with the concentration terms on the right. They may also express evaporation in terms of a thinning rate, rather than mass flux term. Performing this simplification reduces all environmental terms on the right to a single evaporative thinning rate constant, \(E_0\).
Comparison of the lipid resistance versus evaporation rate profiles with the experimental data from King-Smith et al. (2010). (A) Cerretani et al. (2013) experimental estimate. (B) Peng et al. (2014). (C) NLS fit to King-Smith et al. (2010). (D) Cerretani et al. (2013) estimate for in vivo results found in the literature. (E) Bruna and Breward (2014)
For the constants relating to concentration and saturation vapor pressure, we have used values given in Table 5. However, there is a significant variation in the values relating to boundary layer resistances, \(k_m\) and Dk. To resolve this, we determine suitable values for \(k_m\) and Dk using nonlinear least squares fitting to data from the simultaneous aqueous thinning rate and lipid thickness measurements found in King-Smith et al. (2010). Due to the constraints of the original measurement method, there is no data for lipid thicknesses near 0 \(\upmu \)m, and so we have augmented the data with one additional data point for peak observed evaporation rates in the human eye. We use a peak rate of 38 \(\upmu \)m/min, as used in Peng et al. (2014). We consider the thinning rate \(J_{\text {thinning}}\) in \(\upmu \)m/min as a function of lipid thickness \(h_2\) in nm,
and perform the nonlinear least squares (NLS) fit using MATLAB’s lsqcurvefit command. This results in the values for \(k_m\) and Dk given in Table 6. In addition, in Fig. 15, we provide a comparison to the raw data, as well as to the evaporation profiles from several other sources (Bruna and Breward 2014; Cerretani et al. 2013; Peng et al. 2014).
Rights and permissions
About this article
Cite this article
Stapf, M.R., Braun, R.J. & King-Smith, P.E. Duplex Tear Film Evaporation Analysis. Bull Math Biol 79, 2814–2846 (2017). https://doi.org/10.1007/s11538-017-0351-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11538-017-0351-9