Abstract
The use of pre-exposure prophylaxis (PrEP) for HIV prevention within the U.S. military is low. Implementing preference-based alternative modalities of PrEP delivery, however, can be an innovative strategy to address the specific barriers to PrEP uptake among military MSM. We sought to identify population-based, segment-specific preferences for longer-acting and alternative PrEP delivery modalities to guide patient-centered strategies to optimize uptake within military-serving healthcare systems. HIV-negative military men who have sex with men (MSM) completed an anonymous, adaptive choice-based conjoint (ACBC) analysis survey consisting of five key attributes of interest (dosing method, provider type, visit location, lab work evaluation location, and dispensing venue). Relative importance and part-worth utility scores were generated using Hierarchical Bayes (HB) estimation, and cluster ensemble analysis grouped participants into “phenotype” segments by preference similarity. The randomized first-choice model was then used to examine changes in program interest rates among segments through market simulation. The 429 participants were segmented into five preference groups. The dosing method attribute was found to be the most important to nearly all segments. Simulations revealed that PrEP program interest among two segments with low interest levels increased when smartphone, civilian-based, and long-acting injectable PrEP options were involved. Findings also suggested a need for clinics to be responsive and sensitive to sexual practices, risk perception, and functional PrEP knowledge. Responsiveness to segment-specific preferences in the design of military PrEP programs and acting on the importance of clinical relationships within the context of PrEP engagement within a military setting may contribute to increasing PrEP uptake.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Within the U.S. military, there are approximately 350 new HIV infections diagnosed each year; disproportionally affecting those who are younger, Black, and men who have sex with men (MSM) [1,2,3,4,5]. The use of pre-exposure prophylaxis (PrEP) effectively prevents HIV infection [6,7,8,9], and PrEP-related services and medications are currently covered by the Department of Defense’s TRICARE medical insurance program [10]. Yet a military pharmacy analysis reveals that only 2000 of the estimated 12,000 PrEP-eligible individuals in the military have accessed PrEP, with access primarily based on the member’s geographic location relative to a military PrEP-prescribing facility [2]. Military MSM have experienced distinct barriers to PrEP delivery and HIV preventative services when serving within the military healthcare system, such as restricted healthcare access [11], heightened stigma [11, 12], and disclosure discomfort [13]. This low uptake of PrEP, however, cannot be attributed to a lack of interest, as the broader literature has demonstrated high levels of interest and acceptability to a variety of PrEP delivery solutions [14,15,16,17]. Therefore, innovative strategies that can guide the rapid scale-up of PrEP services that are tailored to address the unique needs and challenges of military MSM are needed within the U.S. military healthcare system. It has been shown that health services that match individual treatment preferences positively affect treatment outcomes and uptake [18,19,20]. Thus, our objective was to identify the most preferred attributes of alternative PrEP delivery modalities that are most likely to influence uptake among this population.
Stated preference methods, such as conjoint analysis, are market research strategies particularly suited to quantify consumer preference data of new market products and programs, including for PrEP [17, 21,22,23,24,25,26,27]. Originating from mathematical psychology, the foundational theory of conjoint analysis is that consumers view products and interventions as a composition of various attributes and will place a certain amount of value (part-worth utility score) on each of the attributes. These values can then be entered into market simulation models to predict how consumers might respond to any potential combination of attribute levels [17, 21, 23,24,25,26,27].
While examining utility scores can provide many insights on population-level preferences, large full-sample data can sometimes mask subtle or hidden preference relationships between smaller subgroups of interest—i.e., segments [28]. Therefore, segmenting respondents into homogenous clusters based on similar preferences can reveal nuanced preference data for alternative PrEP delivery models that differ from standard, currently available PrEP programs [29,30,31]. While PrEP is most commonly available as a daily tablet regimen [6,7,8,9], its efficacy can be reduced by pill fatigue, disclosure discomfort, and non-adherence [32, 33]. Thus, alternative modalities of PrEP have been explored to address the barriers that affect the uptake and adherence to a daily tablet regimen. Studies examining tablet regimens on an intermittent, “on-demand” dosing schedule have demonstrated high efficacy among men who have sex with men [34, 35]. Additionally, new Phase III trials of long-acting, injectable formulations of PrEP (HPTN 083/084) found them to have a superior protective effect against HIV acquisition compared to daily oral PrEP among cisgender MSM and transgender women [36], as well as cisgender women [37]. Furthermore, the feasibility and acceptability of conceptual PrEP modalities through implants and rectal douches have also been explored [38,39,40,41]. As long-acting injectable (LAI-PrEP) and alternative modalities of PrEP delivery transition towards real-world implementation, it will be crucial to characterize how U.S. military MSM cluster by preferences for various PrEP delivery programs.
Methods
Between March and April 2020, we partnered with a non-profit organization that supports the needs of LGBTQ military and veteran members to recruit U.S. military MSM and trans-individuals through a closed online social media group comprised of over 7000 self-reported LGBTQ U.S. military members [42]. Organization administrators disseminated weekly advertisements for the study within the group, and interested participants could access the anonymous survey with a “click to consent” procedure if eligible. Participants were provided an option to receive $5 compensation for questionnaire completion, and the study was approved by the Yale University Institutional Review Board.
Clustering participants by preferences first begins with identifying individual-level part-worth utilities from a conjoint experiment [29,30,31]. With a focus on modifiable PrEP program attributes and levels, an adaptive choice-based conjoint (ACBC) analysis survey was developed based on a review of the literature and in-depth, qualitative interviews from PrEP experts and active-duty military MSM [2,3,4,5, 11,12,13, 34, 39, 40, 43,44,45,46,47,48,49,50,51,52,53]. The final survey design was composed of five different PrEP program delivery attributes (and associated levels) that included dosing method (daily tablet, on-demand [before sex] tablet regimen, rectal douche [before sex], injection [every 2 months], implant [once a year]), provider type (military, civilian), visit location (on-base, off-base, smartphone app), dispensing venue (on-base, off-base, mail delivery), and lab evaluation (on-base, off-base, home-based mail-in kit). Before implementation, the survey was piloted and revised with 11 military MSM to ensure that attributes and associated levels were understood, logical, and relevant to a military PrEP program. Additional demographical data was also collected to include age, race, ethnicity, rank type, military branch, geographic region, PrEP experience (“Have you ever used PrEP [Pre-Exposure Prophylaxis]?”), HIV protection satisfaction level, disclosure discomfort, and the HIV Incidence Risk Index for MSM (HIRI-MSM) score [54].
Analysis
The final survey instrument was loaded into Lighthouse Studio 9 and pre-tested for choice task configuration. To achieve a high degree of individual-level precision, the final survey design displayed each attribute level to respondents at least 3 times, had a standard of error of < 0.03, and reported efficiencies were all 1.000 [55].
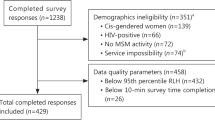
Multiple quality control strategies were employed to protect data integrity. First, security features within the Sawtooth software prevent repeat survey submissions through internet browser cookies and IP addresses [56]. Next, extensive pilot testing revealed that the survey could not be taken in less than 10 to 15 min, thus omitting responses completed in less than 10 min. Additionally, the root likelihood (RLH) fit statistic for each respondent was analyzed to evaluate whether respondents that answered choice questions consistently or randomly at the 95% percentile (0.5178 RLH) [57]. Thus, survey respondents with an RLH below this score were omitted to ensure a 95% confidence level that random responders will fall below this cut-off level [57].
Data analysis began with generating descriptive statistics of the aggregate sample, to include frequencies and measures of central tendency. For conjoint data, part-worth utility scores of all 16 attribute levels were generated using Hierarchical Bayes (HB) estimation [58, 59]. The resulting part-worth utility scores are zero-centered, meaning that scores that are further away from zero indicate a stronger positive or negative preference for the level choice in relation to the other level choices under the same attribute [53, 55, 59]. The attribute relative importance scores, which reflect the amount of influence each attribute has on the respondent’s decision-making, were also calculated by dividing the range of part-worth utility scores for each attribute by the sum of the ranges and multiplying by 100 [60, 61].
Next, cluster ensemble analysis was used to group respondents by individual preferences. For this study, we utilized the “K-Means” method and performed 30 replications with mixed starting points [29]. A five-group cluster solution was achieved with a reproducibility of 82.4% within all clustering algorithms. Reproducibility standard norm within ensemble analysis for a five-segment cluster solution with 10 to 20 basis variables is 76% [30], indicating that this final five-group cluster solution of 82.4% reproducibility was robust and of high validity [29]. Non-parametric tests were then applied to identify significant variance between segments.
Finally, each group’s part-worth utility scores were used to predict the share of preference (program interest rates) to several combinations of PrEP program scenarios through market simulations. Program interest rates for these PrEP scenarios were generated utilizing the randomized first-choice model [60, 61]. This approach assumes that respondents or consumers will prefer a product with the highest composite part-worth utility score (or value), adjusting for both attribute and program variability [60]. All data analyses were performed using XLSTAT and Sawtooth Lighthouse Studio 9.0.
Results
Participants
Tables 1 and 2 in the Appendix display the descriptive statistics of the 429 respondents by preference group. The mean age was 30 years old and 96.7% identified as cis-gendered male. Overall, participants were mostly white (72%), non-Hispanic (72.5%), of officer rank (46.4%), had at least a bachelor’s degree or above (54.1%), and were within the U.S. Army branch (48.7%). Among the aggregate sample, 89.3% received HIRI-MSM scores that defined them as having a high objective risk for acquiring HIV [54]. Cluster ensemble analysis generated five phenotype groups that clustered by preferences and revealed a variety of statistically significant differences. Each phenotype was then labeled with a descriptor based on a defining value.
Group 1 members (N = 156, 36.3%), the largest group, tend to have a higher frequency of condomless, receptive anal sex (CRAS) than their peers, with 88.4% of members reporting an episode of CRAS within the past 6 months, and 33.3% reporting CRAS at a frequency of once a week or more. They are also less likely to report consistent condom use (“every time” or “often”) with regular or casual partners within the last 6 months and are the least likely to have had previous use or experience with PrEP. Additionally, they are more likely to feel uncomfortable discussing their sex life with their primary care provider (PCP) (“extremely” or “somewhat” uncomfortable, 39.1%), and are more likely to have a high degree of anticipated stigma from their PCP (“very” or “somewhat” fearful of judgement from their PCP, 48.7%). This group can be labeled [Least PrEP Experience].
Group 2 members (N = 42, 9.8%) are more racially and ethnically diverse with a membership that is 38.1% non-white race and 45.2% Hispanic ethnicity, and are most likely to report higher levels of education (“bachelors” or “graduate/professional” degree, 69%). They have more members who report being “tops” (anal insertive position preference, 38.1%), are least likely to have engaged in CRAS within the past 6 months (“none,” 35.7%), and are more likely than their peers to report consistent condom use (“every time” or “often”) with regular and casual partners within the last 6 months. While they are more likely to be satisfied with their current level of HIV protection (97.6%), they are also more likely to feel uncomfortable discussing their sex life with their PCP (“extremely” or “somewhat” uncomfortable, 57.1%). This group can be labeled [Least Comfortable Discussing Sex].
Group 3 members (N = 106, 24.7%) tend to be white (82.1%), are more likely to report an education level below a bachelor’s degree (“high school” or “associate degree or some college,” 51.9%), and are more likely to be stationed in the Southern region of the U.S.A (50%). They also tend to prefer anal receptive positions (“versatile” or “exclusively/more bottom,” 84.9%) and are more likely to have had at least one episode of CRAS within the last 6 months (92.5%). Compared to their peers, they are less likely to report consistent condom use with their regular and casual partners within the last 6 months. These members tend to report higher levels of satisfaction with their current level of HIV protection yet are also less likely to have previous use or experience with PrEP. While these members tend to be more comfortable in discussing their sex life with their PCP (“mostly” or “extremely” comfortable, 66.1%), they are also more likely to fear being judged by their PCP for being MSM (“very” or “somewhat” fearful, 60.4%). This group can be labeled [Most Condomless Sex].
Group 4 members (N = 91, 21.2%) tend to report an education level below a bachelor’s degree (“high school” or “associate degree or some college,” 53.9%). While these members report higher levels of previous PrEP experience and are less fearful of judgement from their PCP, they are also less likely to be satisfied with their current level of HIV protection. This group can be labeled [Less HIV Protection Satisfaction].
Group 5 members (N = 34, 7.9%) are more likely to be stationed in the Northeast region of the U.S.A (38.2%), have the highest membership of individuals who identify as Black (26.5%), and are more likely to report an education level of at least a bachelor’s degree (61.8%). They are also more likely to prefer anal receptive positions (“versatile” or “exclusively/more bottom,” 76.5%), are less likely to have engaged in CRAS within the past 6 months (“none,” 26.5%), and are more likely to report consistent condom use (“every time” or “often”) with regular and casual partners within the last 6 months. Out of all groups, these members report the most experience with PrEP (97.1%) yet are also least likely to be satisfied with their current level or HIV protection (73.5%). Compared to their peers, Group 5 members tend to be more comfortable in discussing their sex life with their PCP and are less fearful of being judged by their PCP for being MSM. This group can be labeled [Most PrEP Experience].
Relative Importance Scores and Part-Worth Utilities
Tables 3 and 4 in the Appendix show the relative importance and part-worth utility scores of the five attributes stratified by group. Within this population, dosing method was the most important attribute for Groups 1, 3, 4, and 5, and the provider type was the most important attribute for Group 2.
Group 1 [Least PrEP Experience] had a near equal preference for the PrEP implant and LAI-PrEP and had the strongest preference to see a military provider through a smartphone app for their visits. This large group represents military MSM who want the least demands on their time in terms of taking medications or seeing a provider in person. Group 2 [Least Comfortable Discussing Sex] also strongly preferred the PrEP implant option but were even more influenced by the provider type attribute, with a strong preference to see a civilian healthcare provider in an off-base location for their PrEP visits instead. Group 3 [Most Condomless Sex] had the strongest preference for the daily tablet option and also preferred on-base locations for the other aspects of PrEP services. Group 4 [Less HIV Protection Satisfaction] also preferred on-base locations for PrEP services, but instead preferred the on-demand tablet regimen within the dosing method attribute. Finally, Group 5 [Most PrEP Experience] most strongly preferred the rectal PrEP douche option with a civilian provider preference in an off-base location, yet also preferred to provide labs and receive PrEP medication in a location on-base.
A separate “none” parameter score was also calculated for each of the five-segment groups through respondent selections within the screening task portion of the ACBC survey. The “none” score represents how likely an individual will select “none” or no PrEP program option versus the hypothetical PrEP program scenarios offered within the exercise. Thus, members who possess a higher or positive “none” score will require a PrEP program to possess attributes that are more closely aligned with their preferences before indicating program interest when compared to individuals with a lower or negative “none” score [55]. Within this study, members within Group 2 [Least Comfortable Discussing Sex] had the highest “none” score, and Group 3 respondents [Most Condomless Sex] had the lowest “none” score.
Preferences for PrEP Programs
Tables 5 and 6 in the Appendix present the descriptions and share of preference (program interest) rates of the eight PrEP program scenarios that were constructed to examine program interest among the five groups. Table 7 in the Appendix displays the cross-elasticity effects in program interest rates when offering multiple PrEP program options at once within market simulations.
Differences in program interest rates are observed when multiple program scenarios are offered together as available options, as opposed to being offered as a single choice. Scenario 1 (On-Base Military Daily Tablet) best represents the current policy and structure of a standard, daily tablet PrEP program within the military healthcare system [2, 62]. When this PrEP scenario is offered alone, it has an overall total sample program interest rate of 66.4%, with higher program interest rates among Groups 1, 3, and 4 (71.1%, 92.2%, and 69.1%, respectively) and substantially lower program interest rates among Groups 2 and 5 (2.9% and 35.4%, respectively). In a hypothetical market simulation where Scenario 1 (On-Base Military Daily Tablet) was offered in addition to Scenario 2 (Smartphone Military Daily Tablet) and Scenario 6 (Civilian Daily Tablet), then the overall program interest rate increases to 81.1% among the aggregate sample [PrEP Program Grouping #1, Table 7 in the Appendix], with significant gains in program interest rates among Groups 2 and 5 (64.9% and 52.9%, respectively). Overall program interest rates are further increased to 90.6% among the aggregate sample [PrEP Program Grouping #2, Table 7 in the Appendix] when LAI-PrEP (Scenario 4, Smartphone Military Injection) and implants (Scenario 5, Smartphone Military Implant and Scenario 7, Off-Base Civilian Implants) are also accessible in addition to military- and civilian-based daily tablet PrEP programs. When offering the daily tablet and LAI-PrEP programs together, overall program interest is increased from substantial new member gains occurring within Group 1 [Least PrEP Experience], Group 2 [Least Comfortable Discussing Sex], and Group 5 [Most PrEP Experience]. Most program trade-off within these three groups occurred from members shifting away from daily tablet PrEP programs to the newly introduced scenarios featuring LAI-PrEP and implants.
Discussion
This study’s major findings reveal five unique segments, or phenotypes, within U.S. military MSM with distinct differences among key preference attributes, demographics, sexual practices, PrEP experience, protection satisfaction, provider-related fear, and disclosure discomfort that can significantly influence interest with a PrEP program. Results from the cluster analysis and market simulation demonstrates that maximizing PrEP engagement among segments with lower PrEP program interest must move beyond a “one-size-fits-all” approach and prioritize the availability of additional LAI-PrEP and implant delivery programs. Additionally, segment-specific discomfort and provider-related fear underlines the importance of clinical relationships within a PrEP delivery program. The demonstrated preference for PrEP engagement through different, non-military settings (i.e., civilian provider, off-base setting) within two segments (Groups 2 and 4) compels us to speculate whether the preference to access PrEP through alternative means is a marker of irretrievable distrust of the clinical environment. Either way, the data suggest that the importance of clinical relationships, the design of programs that are responsive to group-specific preferences, and the widest flexibility of options should command more attention.
Overall, the data suggest that the most important factors to consider when designing a PrEP delivery program for military MSM are the dosing method for Groups 1, 3, 4, 5 and provider type for Group 2. While individuals varied in preferences within other attributes, the highest increase in segment-specific PrEP program interest rates occurred when scenarios featured the PrEP implant for Group 1 [Least PrEP Experience], the civilian healthcare provider for Group 2 [Least Comfortable Discussing Sex], the daily tablet for Group 3 [Most Condomless Sex], the on-demand regimen for Group 4 [Less HIV Protection Satisfaction], and the rectal PrEP douche for Group 5 [Most PrEP Experience]. Out of all the groups, members in Group 2 possess the highest “none” utility scores, which means that these individuals are less likely to express an interest in a PrEP program scenario. This is relevant as the preferred PrEP delivery characteristics for this group—a civilian provider and the PrEP implant—are not likely to be widely available for all military members in the near future. These preferences may be explained by higher levels of discomfort when discussing sex among Group 2 members, but ultimately these preferences result in lower program interest rates within scenarios that tend to do best within the aggregate population (e.g., Scenario 2, Smartphone Military Daily Tablet). In contrast, members of Groups 1 and 3 are less likely to be sensitive to incongruence between PrEP program attributes and their preferences, with most of these individuals reporting higher program interest rates to a wider variety of program configurations.
The data also show that augmenting standard military daily tablet PrEP programs with additional PrEP program options that use a smartphone app and civilian providers will reduce clinical demands on patients and increase the overall program interest rate by over 11%. Total program interest rates can be increased even further by offering members LAI-PrEP and implant options through military and civilian platforms (Table 7 in the Appendix). Utilizing smartphone and telehealth strategies is a particularly salient strategy given the limited access to PrEP that service members face today. Currently, PrEP access within the military healthcare system is uneven and appears mostly dependent on geographic proximity to a major military medical center [63]. Accessing PrEP through smartphones or telehealth to more remote areas could markedly increase access. Previous research, however, has shown that telehealth strategies have successfully circumvented geographic challenges to expand access to expert consultation [64], and that distance-based and home, self-testing options are highly accepted and in-demand for future use [63]. Additionally, the use of LAI-PrEP and implants may be a suitable answer for military members with an unpredictable work or deployment schedule that can inhibit adherence to the medication and follow-up requirements of a standard daily tablet PrEP regimen. As LAI-PrEP and implants move from clinical phase trials to routine practice [41, 65,66,67], the high level of interest for these LAI-PrEP agents suggests a substantial potential market for improved, future PrEP engagement among military MSM. Therefore, key stakeholders and policymakers within the Department of Defense should make a concerted effort to expand access to PrEP-prescribing medical facilities through the use of smartphone and telehealth visits, and to incorporate the use of LAI-PrEP and implants as they become available.
Descriptive statistics highlight several significant differences between groups that warrant exclusive assessment. Group 1 [Least PrEP Experience] and Group 3 [Most Condomless Sex] are less likely to have previous use or experience with PrEP, less likely to consistently use condoms with regular and casual partners, and report the highest amounts of condomless receptive anal sex out of all groups. Groups 1 and 3 members are also more likely to fear being judged for their gay/MSM identity by their PCP, which is not an unfounded finding given the history of Don’t Ask, Don’t Tell (DADT), a since-repealed policy that previously discharged military members for disclosing a same-sex orientation [68]. Despite this heightened fear of anticipated stigma, members in both Groups 1 and 3 also have strong preferences for a PrEP program that includes a visit with a military provider. This finding suggests an opportunity for further research to investigate if the fear of anticipated stigma from a PCP is related to military providers on-base or to civilian providers off-base as Group 3 members are more likely to be stationed in the South; a region historically known for lower PrEP uptake and higher HIV-related stigma [69, 70]. Regardless, the combination of higher frequency of CRAS, less consistent use of condoms, and lower previous experience with PrEP can place these members among those with the highest risk for acquiring HIV [54]. Thus, a priority should be made to ensure that these higher risk members have seamless access to PrEP services within the military healthcare system that are responsive to their preferences, as well as healthcare visits that are respectful and non-judgmental to sexual practices and behaviors to further enhance the interaction experience. While members in Group 2 [Least Comfortable Discussing Sex] and Group 5 [Most PrEP Experience] report higher levels of education, are less likely to engage in CRAS, and are more likely to report consistent condom use with regular and casual partners, they both report HIRI-MSM scores that define the majority of their members as having high objective risk for acquiring HIV [54]. Literature on self-perceived risk and PrEP uptake among at-risk individuals continues to expand, with uptake impacted by factors that include beliefs on medication side-effects [71], low perceived personal risk [72], and low PrEP functional knowledge [73]. Therefore, strategies to increase PrEP uptake should include assessing members to determine if barriers or resistance to uptake are rooted in modifiable knowledge and beliefs. With respect to PrEP experience and HIV satisfaction levels, members in Group 4 [Less HIV Protection Satisfaction] and Group 5 both report the highest proportion of previous PrEP use, yet also the lowest amount of satisfaction with their current level of HIV protection. As members within Groups 4 and 5 have dominating preferences for alternative PrEP dosing methods, such as on-demand regimens, PrEP implants, and rectal douches, further research should explore if a member’s satisfaction with their current level of HIV protection is associated with a preferred PrEP delivery model that may not yet be currently available.
Despite the many new and important findings, this study is not without limitations. The anonymous survey relied on self-reported measures for participation eligibility, and thus we must consider the potential for respondent bias as actual military status of the participants cannot be confirmed. As this study identifies and reports on preference data only, future studies will need to examine how preference data translates into actual behavior once implemented into practice. As there is no real “lived” experience with some PrEP delivery options (e.g., implants, rectal douche), interest in these attributes may change as more individuals report on their satisfaction and safety. Additionally, the survey was drawn from a convenience sample recruited from an online social media group, which raises concerns about generalizability and responder bias. Military members who participate in this online LGBT social media group may be more forthcoming with their sexual identity and preferences. Hence, these findings may not be generalizable to at-risk military members who do not identify as being MSM or LGBT.
Conclusion
Preferences and interest for PrEP by at-risk U.S. military service members differ by subgroups, all of which could benefit from PrEP if its delivery were aligned with patient preferences. Five preference groups emerged and suggested that PrEP uptake can be optimized when PrEP delivery programs are designed around the diverse preferences among this population. Models predicted the extent to which the addition of distinct options could translate to a higher level of interest for PrEP engagement. These data can be informative in tailoring the design of PrEP programs to lower participating groups, ultimately improving the overall uptake rate of PrEP within the U.S. military population.
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code Availability
All data analyses were performed using XLSTAT and Sawtooth Lighthouse Studio 9.0.
Abbreviations
- PrEP:
-
Pre-exposure prophylaxis
- MSM:
-
Men who have sex with men
- HIV:
-
Human immunodeficiency virus
- LGBT:
-
Lesbian, gay, bi and transgender
- HB:
-
Hierarchical Bayes
- ACBC:
-
Adaptive choice-based conjoint
- HIRI-MSM:
-
HIV Incidence Risk Index for men who have sex with men
- IP:
-
Internet protocol
- RLH:
-
Root likelihood
- PWUS:
-
Part-worth utility scores
- RIS:
-
Relative importance score
- PCP:
-
Primary care provider
References
Armed Forces Health Surveillance B. Update: Routine screening for antibodies to human immunodeficiency virus, civilian applicants for U.S. military service and U.S. Armed Forces, active and reserve components, January 2013-June 2018. MSMR. 2018;25(9):2–8.
Blaylock JM, Hakre S, Okulicz JF, Garges E, Wilson K, Lay J, et al. HIV preexposure prophylaxis in the U.S. military services - 2014–2016. MMWR Morb Mortal Wkly Rep. 2018;67(20):569–74.
Hakre S, Scoville SL, Pacha LA, Peel SA, Kim JH, Michael NL, et al. Brief report: sexual risk behaviors of HIV seroconverters in the US Army, 2012–2014. J Acquir Immune Defic Syndr. 2015;70(4):456–61.
Patterson SB, Rivera D, Sunil TS, Okulicz JF. Evaluation of extragenital screening for gonorrhea and chlamydia in HIV-infected active duty Air Force members. MSMR. 2014;21(11):7–9.
Hakre S, Mydlarz DG, Dawson P, Danaher PJ, Gould PL, Witkop CT, et al. Epidemiology of HIV among US Air Force Military Personne, 1996-2011. PLoS One. 2015;10(5):e0126700.
Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410.
TRICARE. Is this drug covered? Formulary Search: Truvada. 2022. [Available from: https://www.express-scripts.com/frontend/open-enrollment/tricare/fst/#/formularyPricing/results]. Accessed 8 March 2022.
Russell T. An examination of stigma in the military. Pacific University; 2013. [Available from: https://commons.pacificu.edu/spp/1104]. Accessed 21 Dec 2021.
Anderson CW, Smith HR. Stigma and honor: Gay, lesbian, and bisexual people in the US military. In Homosexual issues in the workplace. 2018 Oct 24 (pp. 65-89). Taylor & Francis.
Biddix JM, Fogel CI, Perry BB. Comfort levels of active duty gay/bisexual male service members in the military healthcare system. Mil Med. 2013;178(12):1335–40.
Sullivan PS, Siegler AJ. Getting pre-exposure prophylaxis (PrEP) to the people: opportunities, challenges and emerging models of PrEP implementation. Sexual health. 2018;15(6):522–7.
Jalil EM, Grinsztejn B, Velasque L, Ramos Makkeda A, Luz PM, Moreira RI, et al. Awareness, willingness, and PrEP eligibility among transgender women in Rio de Janeiro, Brazil. J Acquired Immune Defic Syndr (1999). 2018;79(4):445–52.
Parsons JT, Rendina HJ, Whitfield THF, Grov C. Familiarity with and preferences for oral and long-acting injectable HIV pre-exposure prophylaxis (PrEP) in a national sample of gay and bisexual men in the U.S. AIDS Behav. 2016;20(7):1390–9.
Dubov A, Ogunbajo A, Altice FL, Fraenkel L. Optimizing access to PrEP based on MSM preferences: results of a discrete choice experiment. AIDS care. 2019 May 4;31(5):545-53.
Swift JK, Callahan JL. The impact of client treatment preferences on outcome: a meta-analysis. J Clin Psychol. 2009;65(4):368–81.
Group PC. Patients’ preferences within randomised trials: systematic review and patient level meta-analysis. BMJ (Clinical research ed.). 2008 Oct 31;337:a1864.
Graff FS, Morgan TJ, Epstein EE, McCrady BS, Cook SM, Jensen NK, et al. Engagement and retention in outpatient alcoholism treatment for women. Am J Addiction. 2009;18(4):277–88.
Dubov A, Fraenkel L, Yorick R, Ogunbajo A, Altice FL. Strategies to implement pre-exposure prophylaxis with men who have sex with men in Ukraine. AIDS Behav. 2018;22(4):1100–12.
Dubov A, Ogunbajo A, Altice FL, Fraenkel L. Optimizing access to PrEP based on MSM preferences: results of a discrete choice experiment. AIDS Care. 2019;31(5):545–53.
Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. BMJ. 2000;320(7248):1530–3.
Phillips KA, Maddala T, Johnson FR. Measuring preferences for health care interventions using conjoint analysis: an application to HIV testing. Health Serv Res. 2002;37(6):1681–705.
Viney R, Lancsar E, Louviere J. Discrete choice experiments to measure consumer preferences for health and healthcare. Expert Rev Pharmacoecon Outcomes Res. 2002;2(4):319–26.
Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–77.
Opuni M, Bishai D, Gray GE, McIntyre JA, Martinson NA. Preferences for characteristics of antiretroviral therapy provision in Johannesburg, South Africa: results of a conjoint analysis. AIDS Behav. 2010;14(4):807–15.
Desarbo WS, Jedidi K, Sinha I. Customer value analysis in a heterogeneous market. Strateg Manag J. 2001;22(9):845–57.
Orme B, Johnson R. Improving K-means cluster analysis: ensemble analysis instead of highest reproducibility replicates. Sawtooth Software Research Paper Series. 2008:1–11. Retrieved from: https://sawtoothsoftware.com/resources/technical-papers/ccea-technical-paper
Software S. CCEA v3, Software for Convergent Cluster & Ensemble Analysis. Orem: Sawtooth Software; 2008.
Strehl A, Ghosh J. Cluster ensembles–-a knowledge reuse framework for combining multiple partitions. J Mach Learn Res. 2002;3(Dec):583–617.
Rael CT, Martinez M, Giguere R, Bockting W, MacCrate C, Mellman W, et al. Barriers and facilitators to oral PrEP use among transgender women in New York City. AIDS Behav. 2018;22(11):3627–36.
Gombe MM, Cakouros BE, Ncube G, Zwangobani N, Mareke P, Mkwamba A, et al. Key barriers and enablers associated with uptake and continuation of oral pre-exposure prophylaxis (PrEP) in the public sector in Zimbabwe: qualitative perspectives of general population clients at high risk for HIV. PLoS One. 2020;15(1):e0227632.
Molina JM, Charreau I, Spire B, Cotte L, Chas J, Capitant C, et al. Efficacy, safety, and effect on sexual behaviour of on-demand pre-exposure prophylaxis for HIV in men who have sex with men: an observational cohort study. Lancet HIV. 2017;4(9):e402–10.
Antoni G, Tremblay C, Delaugerre C, Charreau I, Cua E, Rojas Castro D, et al. On-demand pre-exposure prophylaxis with tenofovir disoproxil fumarate plus emtricitabine among men who have sex with men with less frequent sexual intercourse: a post-hoc analysis of the ANRS IPERGAY trial. Lancet HIV. 2020;7(2):e113–20.
Landovitz RJ, Donnell D, Clement ME, et al. Cabotegravir for HIV prevention in cisgender men and transgender women. N Engl J Med. 2021;385(7):595–608. https://doi.org/10.1056/NEJMoa2101016.
HPTN. HPTN 084 study demonstrates superiority of injectable cabotegravir to oral FTC/TDF for the prevention of HIV in cisgender women in Sub-Saharan Africa. 2020. [Available from: https://www.hptn.org/research/studies/hptn084]. Accessed 1 Dec 2021.
Pons-Faudoa FP, Sizovs A, Di Trani N, Paez-Mayorga J, Bruno G, Rhudy J, et al. 2-Hydroxypropyl-beta-cyclodextrin-enhanced pharmacokinetics of cabotegravir from a nanofluidic implant for HIV pre-exposure prophylaxis. J Control Release. 2019;306:89–96.
Pines HA, Gorbach PM, Weiss RE, Hess K, Murphy R, Saunders T, et al. Acceptability of potential rectal microbicide delivery systems for HIV prevention: a randomized crossover trial. AIDS Behav. 2013;17(3):1002–15.
Hendrix CW. HIV antiretroviral pre-exposure prophylaxis: development challenges and pipeline promise. Clin Pharmacol Ther. 2018;104(6):1082–97.
IAS 2019. First-in-human trial of MK-8591-eluting implants demonstrates concentrations suitable for HIV prophylaxis for at least one year. International AIDS Society; 2019. [Available from: https://programme.ias2019.org/Abstract/Abstract/4843]. Accessed 20 July 2020.
MMAM. Modern Military Association of America. 2021. [Available from: https://modernmilitary.org]. Accessed 1 Dec 2021.
Lloyd J, Papworth E, Grant L, Beyrer C, Baral S. Systematic review and meta-analysis of HIV prevalence among men in militaries in low income and middle income countries. Sex Transm Infect. 2014;90(5):382–7.
Hakre S, Blaylock JM, Dawson P, Beckett C, Garges EC, Michael NL, et al. Knowledge, attitudes, and beliefs about HIV pre-exposure prophylaxis among US Air Force Health Care Providers. Medicine (Baltimore). 2016;95(32):e4511.
Galea JT, Kinsler JJ, Salazar X, Lee SJ, Giron M, Sayles JN, et al. Acceptability of pre-exposure prophylaxis as an HIV prevention strategy: barriers and facilitators to pre-exposure prophylaxis uptake among at-risk Peruvian populations. Int J STD AIDS. 2011;22(5):256–62.
Eisingerich AB, Wheelock A, Gomez GB, Garnett GP, Dybul MR, Piot PK. Attitudes and acceptance of oral and parenteral HIV preexposure prophylaxis among potential user groups: a multinational study. PLoS One. 2012;7(1):e28238.
Wheelock A, Eisingerich AB, Ananworanich J, Gomez GB, Hallett TB, Dybul MR, et al. Are Thai MSM willing to take PrEP for HIV prevention? An analysis of attitudes, preferences and acceptance. PLoS One. 2013;8(1):e54288.
Shrestha R, Karki P, Altice FL, Dubov O, Fraenkel L, Huedo-Medina T, et al. Measuring acceptability and preferences for implementation of pre-exposure prophylaxis (PrEP) using conjoint analysis: an application to primary HIV prevention among high risk drug users. AIDS Behav. 2018;22(4):1228–38.
Lykins WR, Luecke E, Johengen D, van der Straten A, Desai TA. Long acting systemic HIV pre-exposure prophylaxis: an examination of the field. Drug Deliv Transl Res. 2017;7(6):805–16.
Shrestha R, Altice F, Karki P, Copenhaver M. Developing an integrated, brief biobehavioral HIV prevention intervention for high-risk drug users in treatment: the process and outcome of formative research. Front Immunol. 2017;8:561.
Toubia O, Hauser J, Garcia R. Probabilistic polyhedral methods for adaptive choice-based conjoint analysis: theory and application. Mark Sci. 2007;26(5):596–610.
Chapman C, Alford J, Johnson C, Weidemann R, Lahav M. CBC vs. ACBC: comparing results with real product selection. Sawtooth Software Conference Proceedings, Sequim, WA. 2009.
Cunningham CE, Deal K, Chen Y. Adaptive choice-based conjoint analysis: a new patient-centered approach to the assessment of health service preferences. Patient. 2010;3(4):257–73.
Wilton J, Kain T, Fowler S, Hart TA, Grennan T, Maxwell J, et al. Use of an HIV-risk screening tool to identify optimal candidates for PrEP scale-up among men who have sex with men in Toronto, Canada: disconnect between objective and subjective HIV risk. J Int AIDS Soc. 2016;19(1):20777.
Software S. Lighthouse Studio v9.0 (Formerly SSIWeb). Orem: Sawtooth Software; 2016.
Software S. Hosting Information. 2022. [Available from: https://sawtoothsoftware.com/hosting]. Accessed 8 March 2022.
Orme B. Consistency cutoffs to identify "bad" respondents in CBC, ACBC, and MaxDiff. Sawtooth Software Research Paper Series. 2019. Retrieved from: https://content.sawtoothsoftware.com/assets/48af48f3-c01e-42ff-8447-6c8551a6d94f
Lenk P, Desarbo W, Green P, Young M. Hierarchical Bayes conjoint analysis: recovery of partworth heterogeneity from reduced experimental designs. Mark Sci. 1996;15:173–91.
Rao VR. Applied conjoint analysis. New York: Springer; 2014 Mar.
Gustafsson A, Herrmann A, Huber F, editors. Conjoint measurement: methods and applications. Springer, Berlin, Heidelberg: Springer Science & Business Media; 2007.
Orme B. Getting started with conjoint analysis: strategies for product design and pricing research. 2nd ed. Madison: Research Publishers LLC; 2010.
Blaylock JM, Hakre S, Decker CF, Wilson B, Bianchi E, Michael N, et al. HIV PrEP in the military: experience at a tertiary care military medical center. Mil Med. 2018;183(suppl_1):445–9.
Siegler AJ, Mayer KH, Liu AY, Patel RR, Ahlschlager LM, Kraft CS, et al. Developing and assessing the feasibility of a home-based preexposure prophylaxis monitoring and support program. Clin Infect Dis. 2018;68(3):501–4.
Touger R, Wood BR. A review of telehealth innovations for HIV pre-exposure prophylaxis (PrEP). Curr HIV/AIDS Rep. 2019;16(1):113–9.
Smith JA, Garnett GP, Hallett TB. The potential impact of long-acting cabotegravir for HIV prevention in South Africa: a mathematical modeling study. The Journal of infectious diseases. 2021 Oct 1;224(7):1179-86.
Greene GJ, Swann G, Fought AJ, Carballo-Dieguez A, Hope TJ, Kiser PF, et al. Preferences for long-acting pre-exposure prophylaxis (PrEP), daily oral PrEP, or condoms for HIV prevention among U.S. men who have sex with men. AIDS Behav. 2017;21(5):1336–49.
Tolley EE, Zangeneh SZ, Chau G, Eron J, Grinsztejn B, Humphries H, et al. Acceptability of long-acting injectable cabotegravir (CAB LA) in HIV-uninfected individuals: hPTN 077. AIDS Behav. 2020;24(9):2520–31.
Lee JL. The comprehensive review working group and Don’t Ask, Don’t Tell repeal at the Department of Defense. Journal of Homosexuality. 2013 Feb 1;60(2-3):282-311.
Oldenburg CE, Perez-Brumer AG, Hatzenbuehler ML, Krakower D, Novak DS, Mimiaga MJ, et al. State-level structural sexual stigma and HIV prevention in a national online sample of HIV-uninfected MSM in the United States. AIDS. 2015;29(7):837–45.
Kerr JC, Valois RF, Diclemente RJ, Fletcher F, Carey MP, Romer D, et al. HIV-related stigma among African-American youth in the Northeast and Southeast US. AIDS Behav. 2014;18(6):1063–7.
From efficacy to effectiveness. facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS Patient Care STDS. 2013;27(4):248–54.
Gallagher T, Link L, Ramos M, Bottger E, Aberg J, Daskalakis D. Self-perception of HIV risk and candidacy for pre-exposure prophylaxis among men who have sex with men testing for HIV at commercial sex venues in New York City. LGBT health. 2014 Sep 1;1(3):218-24.
Kahle EM, Sullivan S, Stephenson R. Functional knowledge of pre-exposure prophylaxis for HIV prevention among participants in a web-based survey of sexually active gay, bisexual, and other men who have sex with men: cross-sectional study. JMIR Public Health Surveill. 2018;4(1):e13.
Acknowledgements
This study was supported by F31 grant number F31NR018620 by the National Institute of Nursing Research (NINR), and the National Institute of Mental Health (NIMH), Center for HIV Identification, Prevention, and Treatment Services (CHIPTS) under award number P30MH059107. The authors would like to thank Carmen Portillo and Nancy R. Reynolds for providing review on earlier versions of this manuscript, and Jennifer Dane and the Modern Military Association of America for assistance with survey distribution.
Funding
This study was supported by F31 grant number F31NR018620 by the National Institute of Nursing Research (NINR), and the National Institute of Mental Health (NIMH), Center for HIV Identification, Prevention, and Treatment Services (CHIPTS) under award number P30MH059107.
Author information
Authors and Affiliations
Contributions
JG, AD, and FLA analyzed and interpreted the preference data regarding PrEP delivery program preferences, as well as demographical descriptive statistics. JG, AD, DV, and FLA were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The study was approved by the Yale University Institutional Review Board (IRB Protocol ID: 2000024612). Social media group administrators placed monthly advertisement links describing the study on the group’s main forum. Interested participants could click on a link to access an online study disclosure form with a ‘click to consent’ procedure.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Tables 1, 2, 3, 4, 5. 6, and 7.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gutierrez, J.I., Vlahov, D., Dubov, A. et al. Preferences for Long-Acting and Alternative Modalities for PrEP among Military Men Who Have Sex with Men: Segmentation Results of an Adaptive Choice-Based Conjoint Analysis Study. J Urban Health 99, 277–292 (2022). https://doi.org/10.1007/s11524-022-00615-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-022-00615-9