Abstract
We sought to determine preferences for oral versus long-acting injectable (LAI) PrEP among gay and bisexual men (GBM). We surveyed a national U.S. sample of 1071 GBM about forms of PrEP. LAI PrEP was found to be acceptable among 43.2 % of men when injected monthly compared with 53.6 % of men when injected every 3 months. When asked to choose between forms of PrEP, 46.0 % preferred LAI, 14.3 % oral, 21.7 % whichever was most effective, 10.1 % had no preference, and 7.8 % would not take PrEP. There were no differences in PrEP preferences by race/ethnicity, income, region of residence, or relationship status. Those unwilling to take PrEP were significantly older than those who preferred LAI PrEP and those who would take either. Those who preferred the most effective form were younger, had less education, and reported more recent club drug use. Those who reported condomless anal sex and those who thought they were good PrEP candidates were more willing to take PrEP. Long-term health and side effects were of the greatest concern for both LAI and oral PrEP. The availability of LAI PrEP has the potential to increase uptake among GBM. The results of ongoing clinical trials of LAI PrEP will need to demonstrate similar or greater efficacy as daily Truvada for uptake to be maximized.
Resumen
Buscamos determinar preferencias sobre PrEP por vía oral en comparación con PrEP inyectable de acción prolongada (LAI; siglas en Inglés) entre hombres gays y bisexuales (GBM; siglas en Inglés). Encuestamos a una muestra nacional de 1,071 GBM en los EE.UU. sobre tipos de PrEP. Se encontró que el PrEP-LAI es más aceptable entre el 43.2 % de los hombres cuando es inyectado mensualmente, en comparación al 53.6 % de los hombres cuando es inyectado cada 3 meses. En comparación al PrEP por vía oral, el 46.0 % prefirió LAI, el 14.3 % por vía oral, el 21.7 % el que fuese más eficaz, el 10.1 % no tuvo preferencia, y el 7.8 % no tomaría PrEP. No hubo diferencias en las preferencias de PrEP por raza/origen étnico, ingresos, región de residencia, o estado civil. Los que no tomarían PrEP eran significativamente mayores que los que prefirieron PrEP-LAI y que los que tomarían cualquiera de los dos. Los que prefirieron la forma más eficaz eran más jóvenes, tenían menos educación e informaron uso reciente de drogas de “club”. Los que reportaron sexo anal sin condón y los que pensaban que eran buenos candidatos para PrEP, estaban más dispuestos a tomar PrEP. Los efectos secundarios y de salud a largo plazo fueron la mayor preocupación tanto para el PrEP-LAI y para el PrEP por vía oral. La disponibilidad de PrEP-LAI tiene el potencial de aumentar su uso entre GBM. Los resultados de estudios clínicos actuales sobre PrEP-LAI, deberán demostrar una eficacia similar o mayor a la Truvada diaria para que su uso sea maximizado.
Similar content being viewed by others
References
CDC. Estimated HIV incidence in the United States, 2007–2010. HIV surveillance supplemental report. 2012;17(4).
CDC. HIV surveillance—epidemiology of hiv infection (through 2013). Atlanta: US Department of Health and Human Services. http://www.cdc.gov/HIV/library/slidesets/index.html (2015).
CDC. Pre-exposure prophylaxis (PrEP). http://www.cdc.gov/hiv/prevention/research/prep/ (2015). Accessed 23 July 2015.
CDC. Preexposure prophylaxis for the prevention of HIV infection in the United States—2014: a clinical practice guideline. http://www.cdc.gov/hiv/pdf/guidelines/PrEPguidelines2014.pdf (2014). Accessed 17 May 2014.
USFDA. FDA approves first drug for reducing the risk of sexually acquired HIV infection. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm312210.htm (2012). Accessed 15 July 2015.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410.
Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34.
Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–90.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Mugo PM, Sanders EJ, Mutua G, van der Elst E, Anzala O, Barin B, et al. Understanding adherence to daily and intermittent regimens of oral HIV pre-exposure prophylaxis among men who have sex with men in Kenya. AIDS Behav. 2015;19(5):794–801.
Celum C, Baeten JM. Tenofovir-based pre-exposure prophylaxis for HIV prevention: evolving evidence. Curr Opin Infect Dis. 2012;25(1):51–7.
Van Damme L, Corneli A, Ahmed K, Agot K, Lombaard J, Kapiga S, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367(5):411–22.
Molina J, Capitant C, Spire B, Pialoux G, Chidiac C, Charreau I, et al., editors. On demand PrEP with oral TDF-FTC in MSM: results of the ANRS Ipergay trial. Conference on retroviruses and opportunistic infections; 2015.
Van der Elst EM, Mbogua J, Operario D, Mutua G, Kuo C, Mugo P, et al. High acceptability of HIV pre-exposure prophylaxis but challenges in adherence and use: qualitative insights from a phase I trial of intermittent and daily PrEP in at-risk populations in Kenya. AIDS Behav. 2013;17(6):2162–72.
Kibengo FM, Ruzagira E, Katende D, Bwanika AN, Bahemuka U, Haberer JE, et al. Safety, adherence and acceptability of intermittent tenofovir/emtricitabine as HIV pre-exposure prophylaxis (PrEP) among HIV-uninfected Ugandan volunteers living in HIV-serodiscordant relationships: a randomized, clinical trial. PLoS One. 2013;8(9):e74314.
Parsons JT, Rendina HJ, Grov C, Ventuneac A, Mustanski B. Accuracy of highly sexually active gay and bisexual men’s predictions of their daily likelihood of anal sex and its relevance for intermittent event-driven HIV pre-exposure prophylaxis. JAIDS J Acquir Immun Defic Syndr. 2015;68(4):449–55.
Kirby T, Thornber-Dunwell M. Uptake of PrEP for HIV slow among MSM. Lancet. 2014;383(9915):399–400.
Mayer KH, Hosek S, Cohen S, Liu A, Pickett J, Warren M, et al. Antiretroviral pre-exposure prophylaxis implementation in the United States: a work in progress. J Int AIDS Soc. 2015;18(4Suppl 3):19980.
Mayer KH, Levine K, Grasso C, Krakower D, Mimiaga MJ, editors. Recent increases in PrEP utilization at a Boston Community Health Center among men who have sex with men, 2011–2014: transition from research to clinical practice. Conference on retroviruses and opportunistic infections (CROI), Seattle; 2015.
Grov C, Whitfield TH, Rendina HJ, Ventuneac A, Parsons JT. Willingness to take PrEP and potential for risk compensation among highly sexually active gay and bisexual men. AIDS Behav. 2015;19:1–11.
Krakower DS, Mayer KH. Pre-exposure prophylaxis to prevent HIV infection: current status, future opportunities and challenges. Drugs. 2015;75(3):243–51.
Levy S. Truvada for PrEP: experts weigh in on the newest way to prevent HIV/AIDS: healthline. http://www.healthline.com/health-news/hiv-truvada-for-hiv-prevention-experts-weight-in-020714#2 (2015). Accessed 15 Oct 2014.
Marcus JL, Glidden DV, Mayer KH, Liu AY, Buchbinder SP, Amico KR, et al. No evidence of sexual risk compensation in the iPrEx trial of daily oral HIV preexposure prophylaxis. PLoS One. 2013;8(12):e81997.
Pérez-Figueroa RE, Kapadia F, Barton SC, Eddy JA, Halkitis PN. Acceptability of PrEP uptake among racially/ethnically diverse young men who have sex with men: the P18 study. AIDS Educ Prev. 2015;27(2):112–25.
Gallagher T, Link L, Ramos M, Bottger E, Aberg J, Daskalakis D. Self-perception of HIV risk and candidacy for pre-exposure prophylaxis among men who have sex with men testing for HIV at commercial sex venues in New York City. LGBT Health. 2014;1:1–7.
Smith DK, Toledo L, Smith DJ, Adams MA, Rothenberg R. Attitudes and program preferences of African-American Urban young adults about pre-exposure prophylaxis (PrEP). AIDS Educ Prev. 2012;24(5):408–21.
Eaton LA, Driffin DD, Bauermeister J, Smith H, Conway-Washington C. Minimal awareness and stalled uptake of pre-exposure prophylaxis (PrEP) among at risk, HIV-negative, black men who have sex with men. AIDS Patient Care STDS. 2015;29:423–9.
Gengiah TN, Moosa A, Naidoo A, Mansoor LE. Adherence challenges with drugs for pre-exposure prophylaxis to prevent HIV infection. Int J Clin Pharm. 2014;36(1):70–85.
Amico KR, Stirratt MJ. Adherence to preexposure prophylaxis: current, emerging, and anticipated bases of evidence. Clin Infect Dis. 2014;59(suppl 1):S55–60.
Grant RM, Anderson P, McMahan V, Liu A, Amico KR, Mehrotra M, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14(9):820–9.
Veilleux Z. Long-acting drug effectively prevents HIV-like infection in monkeys: The Rockefeller University. http://www.newswire.rockefeller.edu/2015/01/15/long-acting-drug-effectively-prevents-hiv-like-infection-in-monkeys/ (2015). Accessed 16 July 2015.
Andrews CD, Yueh YL, Spreen WR, Bernard LS, Boente-Carrera M, Rodriguez K, et al. A long-acting integrase inhibitor protects female macaques from repeated high-dose intravaginal SHIV challenge. Sci Transl Med. 2015;7(270):270ra4.
Andrews CD, Spreen WR, Mohri H, Moss L, Ford S, Gettie A, et al. Long-acting integrase inhibitor protects macaques from intrarectal simian/human immunodeficiency virus. Science. 2014;343(6175):1151–4.
NIH. NIH-supported clinical trials to evaluate long-acting, injectable antiretroviral drugs to prevent HIV infection. http://www.niaid.nih.gov/news/newsreleases/2015/Pages/HPTN076-077.aspx (2015). Accessed 16 July 2015.
Study to Evaluate the Safety Tolerability and Acceptability of Long Acting Injections of the Human Immunodeficiency Virus (HIV) Integrase Inhibitor, GSK1265744, in HIV Uninfected Men (ECLAIR). https://www.clinicaltrials.gov/ct2/show/NCT02076178 (2014). Accessed 12 Jan 2015.
Galea JT, Kinsler JJ, Salazar X, Lee S-J, Giron M, Sayles JN, et al. Acceptability of pre-exposure prophylaxis as an HIV prevention strategy: barriers and facilitators to pre-exposure prophylaxis uptake among at-risk Peruvian populations. Int J STD AIDS. 2011;22(5):256–62.
Ayala G, Makofane K, Santos G-M, Beck J, Do TD, Hebert P, et al. Access to basic HIV-related services and PrEP acceptability among men who have sex with men worldwide: barriers, facilitators, and implications for combination prevention. J Sex Transm Dis. 2013. doi:10.1155/2013/953123.
King HL, Keller SB, Giancola MA, Rodriguez DA, Chau JJ, Young JA, et al. Pre-exposure prophylaxis accessibility research and evaluation (PrEPARE Study). AIDS Behav. 2014;18(9):1722–5.
Mimiaga MJ, Case P, Johnson CV, Safren SA, Mayer KH. Preexposure antiretroviral prophylaxis attitudes in high-risk Boston area men who report having sex with men: limited knowledge and experience but potential for increased utilization after education. J Acquir immune Defic Syndr. 1999;50(1):77–83.
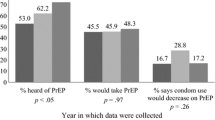
Grov C, Rendina HJ, Whitfield THF, Ventuneac A, Parsons JT. Changes in familiarity with and willingness to take PrEP: results from a longitudinal study of highly sexually active gay and bisexual men. LGBT Health (in press).
Golub SA, Kowalczyk W, Weinberger CL, Parsons JT. Preexposure prophylaxis and predicted condom use among high-risk men who have sex with men. J Acquir Immune Defic Syndr. 2010;54(5):548–55.
Barash EA, Golden M. Awareness and use of HIV pre-exposure prophylaxis among attendees of a Seattle gay pride event and sexually transmitted disease clinic. AIDS Patient Care STDS. 2010;24(11):689–91.
Aghaizu A, Mercey D, Copas A, Johnson AM, Hart G, Nardone A. Who would use PrEP? Factors associated with intention to use among MSM in London: a community survey. Sex Transm Infect. 2013;89(3):207–11.
Holt M, Murphy DA, Callander D, Ellard J, Rosengarten M, Kippax SC, et al. Willingness to use HIV pre-exposure prophylaxis and the likelihood of decreased condom use are both associated with unprotected anal intercourse and the perceived likelihood of becoming HIV positive among Australian gay and bisexual men. Sex Transm Infect. 2012;88:258–63.
Mustanski B, Johnson AK, Garofalo R, Ryan D, Birkett M. Perceived likelihood of using HIV pre-exposure prophylaxis medications among young men who have sex with men. AIDS Behav. 2013;17(6):2173–9.
Grov C, Cain D, Whitfield TH, Rendina HJ, Pawson M, Ventuneac A, et al. Recruiting a US National sample of HIV-negative gay and bisexual men to complete at-home self-administered HIV/STI testing and surveys: challenges and opportunities. Sex Res Soc Policy. 2015;13:1–21.
Greene M, Justice AC, Lampiris HW, Valcour V. Management of human immunodeficiency virus infection in advanced age. JAMA. 2013;309(13):1397–405.
CDC. Diagnosis of HIV infection among adults aged 50 years and older in the United States and dependent areas, 2007–2011. HIV Surveillance Supplemental Report. 2013;18(3).
Kojima N, Klausner JD, editors. Is emtricitabine-tenofovir disoproxil fumarate pre-exposure prophylaxis for the prevention of HIV infection safer than aspirin? Open forum infectious diseases. Oxford: Oxford University Press; 2016.
Gandhi M, Glidden DV, Liu A, Horng H, Amico KR, Mulligan K, et al. Higher cumulative TFV/FTC levels in PrEP associated with decline in renal function. 23rd annual conference on retroviruses and opportunistic infections (CROI 2016), Boston; 2016.
Liu A, Vittinghoff E, Anderson PL, Cohen S, Doblecki-Lewis S, Bacon O, et al. Changes in renal function associated with TDF/FTC PrEP use in the US demo project. 23rd annual conference on retroviruses and opportunistic infections (CROI 2016), Boston; 2016.
Markowitz M, Frank I, Grant R, Mayer KH, Margolis DA, Hudson KJ, et al. ÉCLAIR: Phase 2A safety and PK study of Cabotegravir LA in HIV-uninfected men. 23rd annual conference on retroviruses and opportunistic infections (CROI 2016), Boston; 2016.
Acknowledgments
One Thousand Strong was funded by a research grant from the National Institute on Drug Abuse (R01-DA036466: Jeffrey T. Parsons and Christian Grov, MPIs). H. Jonathon Rendina was supported by a Career Development Award from the National Institute on Drug Abuse (K01-DA039030; H. Jonathon Rendina, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would like to acknowledge the contributions of the other members of the One Thousand Strong Study Team (Tyrel Starks, Ana Ventuneac, Demetria Cain, Mark Pawson, Michael Castro, Ruben Jimenez, Chloe Mirzayi, Brett Millar, Raymond Moody, and Jonathan Lassiter) and other staff from the Center for HIV/AIDS Educational Studies and Training (Chris Hietikko, Andrew Cortopassi, Brian Salfas, Doug Keeler, Qurrat-Ul Ain, Chris Murphy, and Carlos Ponton). We would also like to thank the staff at Community Marketing Inc (David Paisley, Heather Torch, and Thomas Roth) as well as Patrick Sullivan, Jessica Ingersoll, Deborah Abdul-Ali, and Doris Igwe at the Emory Center for AIDS Research (P30 - AI050409). Finally, we thank Jeffrey Schulden at NIDA and all of our participants in One Thousand Strong.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parsons, J.T., Rendina, H.J., Whitfield, T.H.F. et al. Familiarity with and Preferences for Oral and Long-Acting Injectable HIV Pre-exposure Prophylaxis (PrEP) in a National Sample of Gay and Bisexual Men in the U.S.. AIDS Behav 20, 1390–1399 (2016). https://doi.org/10.1007/s10461-016-1370-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1370-5