Abstract
Background
Chemo-immunotherapy (CIT) is the standard of care for advanced non-small cell lung cancer (NSCLC), but the impact of routinely available histo-molecular biomarkers on its efficacy has not yet been fully assessed.
Objective
The purpose of this multicenter study was to evaluate the clinical activity of CIT according to oncogenic drivers, STK11 and TP53 mutations, and MET overexpression.
Patients and methods
Patients receiving CIT for advanced NSCLC with available comprehensive molecular profile were included. The primary endpoint was progression-free survival (PFS), adjusted on main confounding factors, and secondary endpoints were overall survival (OS) and objective response rate.
Results
Among the 195 patients included between September 2018 and October 2021, 88 (41%) had a KRAS mutation, 16 (8.2%) an EGFR mutation or an ALK, ROS1, or RET rearrangement, 11 (5.6%) a BRAF mutation, 6 (3.1%) a MET exon 14 mutation or MET amplification, and 5 (2.6%) a HER2 mutation. Seventy-seven patients (39.5%) had none of these alterations. The median PFS was 6.4 months (95% CI 5.3–7.3). Per subgroup, the median PFS was 7.1 months (5.4–8.9) for KRAS, 5.5 months (2.5–15.3) for EGFR/ALK/ROS1/RET, 12.9 months (2.6–not reached [NR]) for BRAF, 1.5 months (0.6–NR) for MET, 3.9 months (2.6–NR) for HER2, and 5.6 months (4.7–7.8) for patients without any oncogenic alteration. No difference in PFS was observed between the KRAS, BRAF, EGFR/ALK/ROS1/RET, and no-driver subgroups.
STK11 mutations were associated with poor PFS (HR 1.59 [95% CI 1.01–2.51]) whereas TP53 mutations had no impact. MET overexpression was associated with longer PFS (HR 0.59 [95% CI 0.35–0.99]).
Conclusion
This study suggests that the efficacy of combining pembrolizumab with pemetrexed and platinum-based chemotherapy differs according to the histo-molecular biomarkers, which may help to identify patients liable to benefit from CIT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
EGFR mutations or rearrangements were not associated with poor outcomes. |
BRAF-mutated patients seemed to benefit most from chemo-immunotherapy. |
STK11 mutations were associated with poor survival and patients with MET overexpression showed increased survival. |
1 Introduction
Over the past 15 years, treatment of advanced non-small cell lung cancer (NSCLC) has undergone profound changes, with the development of targeted therapies and immune checkpoint inhibitors (ICIs). These therapeutics offer the possibility of long-term disease control. Meanwhile, histo-molecular profiling has become part of routine care, its aim being to detect targetable oncogenic alterations and biomarkers predictive of response to both targeted therapies and immunotherapy [1].
Inhibitors of programmed cell death-1 (PD1) or programmed cell death ligand-1 (PDL1) have significantly improved the prognosis of patients with advanced NSCLC, but their efficacy is in fact variable, and only a subset of patients actually derives a prolonged benefit from immunotherapy [2, 3]. Several potential biomarkers, reflecting the balance between the pro-inflammatory anti-tumor immune response and immune evasion mechanisms, may allow more accurate prediction of the clinical response to immunotherapy, but only the PDL1 tumor proportion score (TPS) is currently used in clinical practice [4].
Testing for a driver oncogene alteration may help determine which patients may benefit from ICI treatment as monotherapy. Anti-PD(L)1 agents are associated with poor outcomes in patients with EGFR mutations and ALK rearrangements [5,6,7,8]. This lack of sensitivity may be related to an uninflamed tumor micro-environment and a low tumor mutational burden (TMB) [9, 10]. As a consequence, patients with EGFR mutations or ALK rearrangements have been excluded from most clinical trials evaluating anti-PD(L)1 as first-line therapy. In contrast, KRAS mutations appear to be predictive of a good response to ICI treatment, which can be explained by their association with an inflammatory tumor microenvironment and a high PDL1 TPS, a high CD8+ T-cell infiltration, and a high TMB, which may reflect the strong epidemiological link with smoking [11, 12]. However, interactions between anti-PD(L)1 agents, tumor cells, and host immunity are complex, and co-mutations may impact the efficacy of ICI treatment. For example, STK11 mutations correlate with a poor response rate [13].
Other predictive markers of the efficacy of ICIs have been gradually explored from the tumor immune microenvironment (phenotype of tumor infiltrating lymphocytes, T-cell receptor repertoire diversity) to the exploration of circulating and host systemic markers (peripheral blood cells, inflammatory circulating proteins, Human Leukocyte Antigen-I variability, intestinal commensal microbiota) but are not yet integrated into clinical practice [14].
It has been demonstrated that adding anti-PD(L)1 to standard chemotherapy increases the chances of response and prolongs survival [12, 15]. Consequently, the combination of chemotherapy with immunotherapy (chemo-immunotherapy, CIT) has become a standard of care for advanced NSCLC [1]. The benefits observed with this combination may result from synergy between the immune response induced by ICIs and the immunogenic effects of chemotherapy, such as an increased release of tumor antigens (immune cell death), inhibition of myeloid-derived suppressor cells, or an increased ratio of cytotoxic lymphocytes to regulatory T cells [16]. Given the specificities of the mechanism of action of CIT, the usual biomarkers of response to PD(L)1 pathway inhibition might not be relevant to CIT. In particular, it remains to be seen whether the poor sensitivity to immunotherapy observed in patients with oncogene addiction holds true when chemotherapy is added. On the basis of the anti-tumor immunological effects of chemotherapy, one can hypothesize that adding chemotherapy to immunotherapy might promote recovery of immunosurveillance function and restore the activity of ICIs in ‘cold’ tumors. We thus conducted a multicenter observational study to describe the efficacy of CIT according to histo-molecular factors.
2 Methods
2.1 Study Design and Population
This real-world observational study was carried out in five centers. All successive patients with non-squamous NSCLC, aged 18 years or older, and for whom molecular profiling was performed and interpretable at baseline were included if they had received a combination of platinum-based chemotherapy and anti-PD(L)1 agent, regardless of the treatment line. Patients were identified through a systematic search with prescription software.
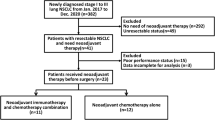
We excluded progression-free patients who had received only one cycle of CIT followed by chemotherapy or immunotherapy alone and patients who directly switched from chemo-immunotherapy to targeted therapy before any progression, when the results of molecular profiling were received. Patients treated as part of a clinical trial were also excluded (Supplementary Figure A, see electronic supplementary material [ESM]).
Patients were divided into subgroups according to their oncogenic alterations: KRAS mutations, EGFR mutations or ALK/ROS1/RET rearrangements, BRAF mutations, MET exon 14 skipping mutations or MET amplification, HER2 mutations, or no oncogenic driver alterations (Fig. 1). EGFR and key rearrangements were grouped together, as they share common clinical characteristics (especially regarding smoking status) and a lack of sensitivity to immunotherapy and as they allow the use of first-line targeted therapies [7, 8, 17].
Kaplan-Meier curves of progression-free survival in each oncogenic driver subgroup. Shown are Kaplan–Meier estimates of progression-free survival in patients without oncogenic alteration, with KRAS mutations, with EGFR mutations or ALK, ROS1 or RET rearrangements, with BRAF mutations, with MET exon 14 skipping mutations or MET amplifications and with HER2 mutations. Tick marks indicate censoring of data.
2.2 Data Collection and Assessments
Patient demographics (sex, age, smoking history, Eastern Cooperative Oncology Group performance status [ECOG PS], previous therapeutic regimens) and tumor characteristics (staging [8th edition TNM classification], molecular profiling, PDL1 TPS, MET expression) were collected at baseline.
ALK rearrangement testing and PDL1 TPS were carried out at each center by immunohistochemistry (IHC) assay, according to local procedures. In case of inconclusive results, the presence of ALK rearrangement was confirmed by fluorescent in situ hybridization (FISH). ROS1 fusion screening was centralized at Lille University Hospital and was assessed by IHC assay with D4D6 antibody followed by a FISH test for confirmation. Mutational testing was performed at Lille University Hospital with DNA-based Ampliseq NGS multiplex panels (Ion AmpliSeq custom panel or Colon and Lung V2, Thermofisher Scientific) [18, 19]. MET IHC was centrally performed at Lille University Hospital with SP44 antibody and was graded from 0 to 3+ according to the intensity of the staining and the proportion of stained cells (1+: ≥ 50% of cells with low-intensity marking; 2+: ≥ 50% of cells with moderate-intensity marking; 3+: ≥ 50% of cells with high-intensity marking) [20]. In the case of MET IHC 3+, gene copy number was investigated by FISH with the ZytoLight SPEC MET/CEN 7 Dual Color assay. MET amplification was defined as a MET/CEP7 ratio ≥ 1.8, mean MET gene copy number ≥ 6, or the presence of clusters [21].
2.3 Endpoints
The primary endpoint was real-world progression-free survival (PFS). The secondary endpoints were overall survival (OS) and real-world objective response rate (ORR). PFS was defined as the interval between treatment initiation and the date of either death or documented progression according to the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1. OS was defined as the interval between treatment initiation and the date of either death or the last follow-up. The ORR refers to the percentage of patients with a complete or partial response according to RECIST version 1.1.
2.4 Statistical Analysis
Categorical variables are expressed in terms of frequency, and percentage and quantitative variables in terms of mean and standard deviation (in case of normal distribution) or median and interquartile range (IQR) (in case of non-normal distribution).
Median follow-up time was estimated by a reverse Kaplan Meier method counting patients who died as censored.
PFS and OS were estimated by the Kaplan-Meier method and compared with the Log-rank test. The Cox proportional hazards model was used to estimate hazard ratios (HR) and their 95% confidence intervals (95% CI). Patients still on treatment at last update were censored at the date of last follow-up. The MET mutations and HER2 mutations subgroups had to be excluded from comparative analyses because of the small number of patients involved.
Comparisons of survival analyses according to oncogenic driver subgroups were adjusted for prespecified confounders (age ≥ 70 years [22], performance status [0–1 vs 2], smoking status [never-smoker vs ever-smoker], disease stage [IV-B vs other], and number of previous lines) with a multivariable Cox proportional hazards model. We also investigated the independent association of TP53 mutations, STK11 mutations, and PDL1 TPS (< 1% vs ≥ 1%) with a multivariate Cox proportional hazards model, including prespecified confounders as covariates. We did not include MET overexpression in the multivariate model because of the amount of missing data (63%). Proportionality hazard assumptions were assessed by examining the Schoenfeld residuals plots, and no strong deviations were found (data not shown).
Median duration of treatment was estimated by the Kalbfleisch and Prentice method. Statistical testing was done at the two-tailed α level of 0.05, without adjustment for multiple comparison issues.
Statistical analyses were carried out with SAS software (SAS Institute, Cary, NC, USA; version 9.4).
2.5 Ethical Disclosures
This retrospective, non-interventional study was conducted in compliance with GDPR (EU General Data Protection Regulation) and MR004 (Reference Methodology 004 for data protection). The data were collected from local medical files and processed anonymously for analysis. The patients were informed, by a mention in medical letters, of treatment of their data for research purposes. The local databases and medical files were searched for any potential refusal of additional data treatment.
3 Results
3.1 Baseline Characteristics
In total, 261 patients with locally advanced or metastatic non-squamous NSCLC treated with platinum-based chemotherapy and an anti-PD(L)1 agent were identified between September 2018 and October 2021. Sixty-six patients were excluded, mainly because no NGS testing had been performed (Supplementary Figure A, see ESM). Overall, 195 patients were included. All of them had received treatment with pembrolizumab, platinum, and pemetrexed.
The demographics and clinical characteristics of the patients at baseline are described in Table 1. Median age was 62 years. One hundred and twenty-four patients (64%) were men. Most patients had a favorable PS of 0 or 1 (87%), were current or former smokers (88%), and had metastatic disease (96%).
Twenty-five patients (12.8%) had received prior treatment for advanced disease. Among these patients, nine had received more than one prior line of treatment. Respectively, 20 patients (10.3%), 12 patients (6.2%), and 7 patients (3.6%) had received prior chemotherapy, targeted therapy, or ICI treatment. Three patients with EGFR mutation (out of 8), one patient with ALK rearrangement (out of 5) and one patient with ROS1 rearrangement (out of 2) received CIT in first line, before any targeted therapy.
PDL1 TPS was available in 183 patients (94%). Sixty-eight patients (35%) had a PDL1 TPS < 1%, 60 patients (31%) had a PDL1 TPS of 1–49%, and 55 patients (28%) had a PDL1 TPS ≥ 50%. MET expression was assessed in 72 patients (37%). Thirty-three patients (46%) had a moderate or high (2+ or 3+) MET expression score.
3.2 Molecular Profiling
One hundred and eighteen patients (60.5%) had at least one oncogenic driver alteration, including 80 patients (41%) with KRAS mutations (G12C, n = 38), 8 patients (4.1%) with EGFR mutations (exon19del or Leu858R, n = 5; exon 20 insertion, n = 2; other, n = 1), 5 patients (2.6%) with ALK rearrangements, 2 patients (1%) with ROS1 rearrangements, 1 patient (0.5%) with a RET rearrangement, 11 patients (5.6%) with BRAF mutations (V600E, n = 6; non-V600E, n = 5), 4 patients (2.1%) with MET exon 14 mutations, 2 patients (1%) with MET amplification, and 5 (2.6%) patients with HER2 mutations (Supplementary Figure A, see ESM). TP53 mutations were found in 102 patients (52%) and STK11 mutations in 37 patients (19%). Among the oncogenic drivers, only KRAS (n = 16) and BRAF (n = 1, non-V600E) mutations were associated with SKT11 mutations (Table 1).
3.3 Treatment Characteristics
Forty-one patients received cisplatin (21%) and the others received carboplatin. Maintenance was conducted for 131 patients (67%). The median number of cycles administered was 8 (IQR 4–13). The main reasons for discontinuing treatment were progressive disease (n = 163, 84%), toxicity (n = 21, 11%), and death (n = 13, 6.7%). Thirty-two patients (16%) were still on treatment at the time of data cutoff.
3.4 Progression-Free Survival
With a median follow-up of 20.2 months (IQR 15.7–25.2), 151 events were recorded. In the entire cohort, median PFS was 6.4 months (95% CI 5.3–7.3). The proportions of patients who were progression free and alive at 6, 12, and 18 months were 51%, 29%, and 22%, respectively.
Regarding driver subgroups, median PFS (mPFS) was 7.1 months (95% CI 5.4–8.9) for KRAS, 5.5 months (95% CI 2.5–15.3) for EGFR/ALK/ROS1/RET, 12.9 months (95% CI 2.6–not reached [NR]) for BRAF, 1.5 months (95% CI 0.6–NR) for MET, 3.9 months (95% CI 2.6–NR) for HER2, and 5.6 months (95% CI 4.7–7.8) for the no-driver subgroup (Fig. 1, Table 2). After adjustment for age, PS, smoking status, disease stage, and number of previous lines, PFS did not differ between the KRAS, EGFR/ALK/ROS1/RET, BRAF, and no-driver subgroups (p = 0.70). Initial stage (IV-B) was the only variable associated with PFS (p = 0.012).
In univariate analysis, PFS did not differ either between the EGFR/ALK/ROS1/RET subgroup and the others (HR 1.00 [95% CI 0.55–1.80]; p = 0.99), between the KRAS subgroup and the others (HR 0.83 [95% CI 0.60–1.14]; p = 0.24), or between the BRAF subgroup and the others (HR 0.63 [95% CI 0.34–1.16]; p = 0.22), although a trend was observed in favor of KRAS and BRAF patients (Supplementary Figures B–D, see ESM).
In an exploratory analysis, median PFS did not appear to differ between the EGFR patients and those harboring rearrangements (5.6 months [95% CI 0.82–15.35] and 4.7 months [2.6–5.6], respectively). Among the BRAF-mutated patients, median PFS appeared to be higher in case of V600E mutations as compared with non-V600E mutations (20.3 months [95% CI 2.6–NR] vs 8.4 months [0.7–NR]).
Among the patients with PFS ≥ 12 months, two had EGFR mutations (including 1 L858R mutation) (out of eight), two had ALK rearrangements (out of five), four had BRAF V600E mutations (out of 11), 21 had KRAS mutations (ouf of 80), and none had a MET alteration or HER2 mutation.
Regarding the other histo-molecular markers, median PFS was 3.0 months (95% CI 2.5–5.8) for STK11-mutated patients (Fig. 2A), 6.6 months (95% CI 6.0–7.8) for TP53-mutated patients (Supplementary Figure E1, see ESM), 6.9 months (95% CI 4.6–9.9) for patients with MET expression ≥ 2 (Fig. 3A) and 8.6 months (95% CI 6.9–11.0) for patients with PDL1 TPS ≥ 1%. After adjustment for age, PS, smoking status, disease stage, number of previous lines, and STK11, TP53, and PDL1 status, PFS was significantly shorter for patients with STK11 mutations (HR 1.59 [95% CI 1.01–2.51]; p = 0.049), or with an advanced stage (IV-B) (p = 0.009) and significantly longer for patients with PDL1 ≥ 1% (HR 0.62 [95% CI 0.42–0.91]; p = 0.014).
Kaplan-Meier curves of progression-free survival and overall survival according to SK11 mutational status in the overall population (A, B) and in the KRAS sub-group (C, D). Shown are Kaplan–Meier estimates of progression-free survival and overall survival in patients with inactivating STK11 mutations and in patients without inactivating STK11 mutation in the overall population (A, B) and in KRAS-mutated patients (C, D). Tick marks indicate censoring of data. HR hazard ratio, KRASm KRAS mutation, KRASwt KRAS wild-type, mOS median overall survival, mPFS median progression-free survival, STK11m STK11 mutation, STK11wt STK11 wild-type, 95% CI 95% confidence interval
Kaplan-Meier curves of progression-free survival (A) and overall survival (B) according to MET expression score. Shown are Kaplan–Meier estimates of progression-free survival and overall survival in patients harboring MET overexpression (immunohistochemistry staining scores of 2+ or 3+) and in patients without MET overexpression (immunohistochemistry staining scores of 0+ or 1+). Tick marks indicate censoring of data. HR hazard ratio, mOS median overall survival, mPFS median progression-free survival, NR not reached, 95% CI 95% confidence interval
In univariate analysis, the negative impact of STK11 mutations was stronger among KRAS-mutated patients (mPFS of 2.6 months [95% CI 1.4–10.0] for KRAS patients with a SKT11 co-mutation versus 7.5 months [6.5–9.8] for KRAS patients without a STK11 co-mutation; HR 2.38 [95% CI 1.34–4.25]; p = 0.002) (Fig. 2C).
TP53 mutations were not associated with PFS in either the KRAS subgroup (p = 0.30) or the EGFR/ALK/ROS1/RET subgroup (p = 0.88).
Expression of PDL1 ≥ 50% in the EGFR/ALK/ROS1/RET subgroup seemed associated with longer PFS (mPFS 6.4 months [95% CI 3.2–NR] for PDL1 TPS ≥ 50% vs 3.2 months [0.82–NR] for PDL1 TPS < 50%).
Regarding MET expression, which is available for 72 patients (37%), MET overexpression ≥ 2+ was significantly associated with longer PFS in univariate analyses (HR 0.59 [95% CI 0.35–0.99]; p = 0.043) (Fig. 3A).
Median PFS was 5.26 months (95% CI 2.6–9.2) in never-smokers or lighter smokers (≤ 5 pack-years) and 6.47 months (95% CI 5.3–7.9) in ever-smokers (> 5 pack-years); HR 1.18 (95% CI 0.75–1.85); p = 0.30, in univariate analysis (Supplementary Figure F, see ESM).
3.5 Response Rate
The ORR was 46% in the whole population, ranging from 17% for the MET-dysregulated subgroup to 55% for the BRAF subgroup (Fig. 4). The ORR was similar for the EGFR/ALK/ROS1/RET, KRAS, and no-driver subgroups (44%, 46%, and 48%, respectively), whereas it was only approximatively 20% in the case of HER2 mutations. Among the patients with BRAF mutations, contrasting response rates were observed, ranging from 83% for BRAF V600E NSCLC to 20% for BRAF non-V600E NSCLC.
3.6 Overall Survival
During follow-up, a total of 101 deaths were recorded. The estimated proportions of patients who were alive at 6 months, 12 months, and 18 months were 78%, 62%, and 48%, respectively. Overall, the median OS (mOS) was 16.7 months (95% CI 13.0–20.9).
Regarding the driver subgroups, the median OS was 18.6 months (95% CI 12.16–NR) for KRAS, 13.0 months (95% CI 6.7–20.6) for EGFR/ALK/ROS1/RET, 21.8 months (95% CI 6.3–NR) for BRAF, 15.8 months (95% CI 1.8–NR) for MET, and 15.0 months (95% CI 3.6–NR) for HER2. For patients without any of these oncogenic drivers, mOS was 16.7 months (95% CI 10.0–20.9). After adjustment for prespecified confounders, OS did not differ between the KRAS, EGFR/ALK/ROS1/RET, BRAF, and no-driver subgroups (p = 0.74). Initial stage (IV-B) and age ≥ 70 years old were significantly associated with PFS (p = 0.002 and p = 0.039, respectively).
Regarding other histo-molecular markers, median OS was 9.9 months [95% CI 4.8–13.7] for STK11-mutated patients (Fig. 2B), 16.8 months [95% CI 13.0–21.1] for TP53-mutated patients (Supplementary Figure E2, see ESM), not reached [95% CI 15.0–NR] for patients with MET expression ≥ 2+ (Fig. 3B), and 26.1 months [95% CI 15.9–NR] for patients with PDL1 TPS ≥ 1%. After adjustment for age, PS, smoking status, disease stage, number of previous lines, and STK11, TP53, and PDL1 status, OS was significantly shorter for patients with STK11 mutations (HR 1.88 [95% CI 1.11–3.22]; p = 0.021) and with an advanced stage (IV-B) (p = 0.009) and significantly longer for patients aged < 70 years old (p = 0.039) or with PDL1 TPS ≥ 1% (HR 0.62 [95% CI 0.42–0.91]; p = 0.014).
Like its effect on PFS, the prognostic impact of STK11 was also more pronounced in the KRAS subgroup (mOS of 5.6 months [95% CI 3.2–NR] for KRAS patients with STK11 co-mutations vs 21.1 months [14.2–NR] for KRAS patients without STK11 co-mutations; HR 2.38 [95% CI 1.33–4.25]; p = 0.003) (Fig. 2D). TP53 mutations were not likewise associated with OS in the KRAS subgroup (p = 0.68).
In univariate analyses, OS was significantly longer in patients with MET overexpression ≥ 2+ than those without (HR 0.47 [95% CI 0.24–0.92]; p = 0.028) (Fig. 3B).
4 Discussion
We have conducted a ‘real-world’ multicentric retrospective study to analyze the clinical activity of CIT according to different biomarkers identified as predictive of the response to ICI treatment. We also describe, for the first time, the impact of MET expression on the efficacy of CIT.
In our real-world study, PFS was lower than in the KEYNOTE-189 clinical trial (9.0 months) and also lower than in a retrospective study evaluating the real-word effectiveness of CIT in untreated patients (8.6 months) [15, 23]. These results might be due to the higher proportion of pre-treated patients and patients with impaired PS included in our study.
However, it does not appear to be related to the inclusion of patients with EGFR mutations or ALK rearrangements. Indeed, although the lack of statistical difference in PFS between driver subgroups may be due to the lack of power because of the low number of patients in the EGFR/ALK/ROS1/RET and BRAF subgroups, response to CIT did not appear to be impaired in patients with EGFR mutations and rearrangements in our study.
The place of CIT in patients with EGFR mutations or key rearrangements, after progression on tyrosine kinase inhibitor, is still under discussion. Whereas EGFR mutations and ALK rearrangements are associated with a lack of efficacy with immunotherapy as monotherapy [10, 24], our study did not show poor outcomes in the EGFR and rearrangements subgroups. These results are consistent with the fact that smoking was not associated with PFS in our study. However, we cannot assess whether the benefit is due to the addition of immunotherapy, synergy with the immunological effects of chemotherapy, or chemotherapy alone. Pemetrexed has indeed been shown to be associated with a favorable outcome in oncogene-addicted cancers, especially ALK-rearranged NSCLC [25]. Shen et al. and Benjamin et al. reported PFS durations close to those of our study in patients with EGFR mutations treated by CIT [26, 27].
The efficacy of CIT in NSCLC patients with EGFR mutations is uncertain. The ORIENT-31 clinical trial reported a PFS benefit with sintilimab plus chemotherapy compared with chemotherapy alone, while KEYNOTE-789 failed to demonstrate a significant improvement of PFS and OS with the addition of pembrolizumab to chemotherapy [28, 29]. The addition of bevacizumab appears to have a potentially beneficial role in some cases [29,30,31]. However, further research is needed to determine the best treatment for these patients. No patients treated with CIT plus bevacizumab were identified in our study.
Despite close clinical and pathophysiological characteristics and similar profiles of response to immunotherapy as monotherapy [7, 8, 32], HER2-mutated patients seemed, in our study, to have derived less benefit from CIT than those with EGFR mutations. Yang et al. reported that CIT did not improve PFS compared with chemotherapy alone in a retrospective cohort of 210 HER2-mutated patients (mPFS: 5.2 months vs 4.0 months, HR 0.77 [95% CI 0.52–1.14]) [33]. Saalfeld et al. showed better outcomes with CIT (mPFS: 6 months; ORR: 52%) than with ICI alone (mPFS: 4 months; ORR: 16%) in 61 HER2-mutated patients [34]. We report poorer results in these patients, but the number of patients was very small, which may have led to sampling variance. Additional studies are needed to better assess the impact of HER2 mutations on the efficacy of CIT.
In our study, patients with BRAF mutations derived the greatest benefit from CIT. These results are mainly driven by BRAF V600E patients, although most of these were never-smokers (67%) and only one had high expression of PDL1 ≥ 50%. A case report has also shown a prolonged response to CIT in a never-smoker BRAF V600E NSCLC patient [35]. Retrospective studies having investigated the efficacy of immunotherapy alone in patients with BRAF mutations have reported a mPFS in the range of 1.5–5.3 months [36]. These results, if confirmed, would raise the question of the best therapeutic sequence between CIT and targeted therapies, as already discussed for BRAF-mutated melanoma patients.
Patients with MET exon 14 mutations or MET amplification showed the poorest outcomes. Median PFS was similar in the two patients with MET amplification (1.5 and 1.6 months) but varied markedly among the four patients with MET exon 14 skipping, from 0.6 to 8.6 months. Biological studies suggest that the MET/HGF axis plays an immunomodulatory role in the tumor microenvironment [37, 38], but favorable outcomes have been reported in several studies evaluating ICI as monotherapy in the case of MET alterations [36]. Given these discrepant results and the small number of patients with MET alterations included, further studies are needed to specify the role of these alterations in responses to CIT. However, the advanced age of patients with MET alterations may partly explain these poor results [39].
Two meta-analyses have shown that KRAS mutations are a potential biomarker of a survival benefit from ICI treatment, because they promote a proinflammatory tumor micro-environment [40, 41]. In our study, PFS did not differ statistically between the KRAS subgroup and other patients, but the Kaplan-Meir curves seem to be in favor of the KRAS patients. These results are consistent with an exploratory analysis of the KEYNOTE-189 trial [42]. In the IMPOWER-150 trial, however, survival with ACP (atezolizumab plus carboplatin plus paclitaxel) was shorter in KRAS-mutated patients compared with patients without KRAS mutation [43]. On the basis of these findings, the role of KRAS mutations as predictive biomarkers of response is less clear with CIT than with immunotherapy alone.
STK11 mutations appeared to be a factor of poor prognosis in the whole cohort and particularly in the KRAS subgroup. They have likewise been shown previously to be associated with poor prognosis in patients receiving ICI treatment [43, 44]. Although strongly associated with smoking, STK11 inactivation has been shown to result in a cold immunosuppressive environment characterized by low PDL1 TPS and a low density of T CD8+ lymphocytes [44]. Accordingly, among the STK11-mutated patients included in our study, 51% had PDL1 TPS < 1% and only one had PDL1 TPS ≥ 50%. Yet, low PDL1 expression is insufficient to explain the fact that STK11-mutated patients do not benefit from the synergistic immunological effects of CIT. Further investigations are needed to understand the pathways underlying impairment of the antitumor immune response in the case of STK11 mutations, but several potentially interrelated mechanisms have already been outlined: downregulation of chemokines and interferons α and β, increased immunosuppressive cytokines, metabolic competition with immune effector cells, enhanced prostaglandin production, and impairment of dendritic cell recruitment [13].
Another tumor suppressor, p53, leads to accumulated DNA damage and thus to increased tumor immunogenicity. In two reported series, TP53 mutations were found to correlate positively with ICI efficacy [45, 46]. In the IMPOWER-150 trial, TP53 mutations were associated with better outcomes with ABCP (atezolizumab plus bevacizumab plus carboplatin plus paclitaxel), but not with ACP, in KRAS patients [43]. In our study, no difference in efficacy was observed according to the presence of TP53 mutations, but the PFS Kaplan-Meier curves tended to separate at 12 months and beyond in favor of TP53-mutated patients.
MET overexpression has been linked to poor prognosis in NSCLC patients, in line with the biological properties of MET, known to promote proliferation and invasiveness [21, 47]. Surprisingly, in our study, MET overexpression was associated with better efficacy and longer survival, although the amount of missing data limits the scope of the results. To our knowledge, this is the first description of the efficacy of anti-PD(L)1-based therapy according to the level of MET overexpression. MET expression has been found to be associated with high PDL1 expression and tumor-infiltrating lymphocytes in NSCLC [48]. The reason MET overexpression correlated with survival while patients harboring MET exon 14 mutations and MET amplification showed poor outcomes is unclear. Some points worth considering could be the lack of correlation between MET overexpression and MET inhibitor efficacy and differences in patient characteristics, especially in terms of age and smoking status [49,50,51].
The small number of patients in molecular subgroups is the main limitation of this work and may have led to a lack of power and sampling bias. Further limitations stem from its retrospective design, including reporting bias, a lack of centralized radiological assessment, and variable scanning intervals along with alpha inflation due to multiple testing.
Despite these limitations, this study suggests that the efficacy of combining pembrolizumab with pemetrexed and platinum-based chemotherapy differs according to certain histo-molecular biomarkers, which may help determine which patients are liable to benefit from CIT.
The histo-molecular response factors evaluated in our study, which are those currently available in clinical practice, reflect the biological diversity of NSCLC but do not seem sufficient for predicting the response to CIT. The identification of new biomarkers, especially immunological scores, could provide better understanding of the complexity of the tumor microenvironment and could help to optimize treatments through a personalized approach.
References
Clinical Practice Living Guidelines—Metastatic Non-Small-Cell Lung Cancer | ESMO, (n.d.). https://www.esmo.org/guidelines/guidelines-by-topic/lung-and-chest-tumours/clinical-practice-living-guidelines-metastatic-non-small-cell-lung-cancer. Accessed 6 Aug 2022.
de Castro G, Kudaba I, Wu Y-L, Lopes G, Kowalski DM, Turna HZ, et al. KEYNOTE-042 5-year survival update: pembrolizumab versus chemotherapy in patients with previously untreated, PD-L1–positive, locally advanced or metastatic non–small-cell lung cancer. J Immunother Cancer. 2021;9:363. https://doi.org/10.1136/jitc-2021-SITC2021.363.
Borghaei H, Gettinger S, Vokes EE, Chow LQM, Burgio MA, de Castro Carpeno J, et al. Five-year outcomes from the randomized, phase III Trials CheckMate 017 and 057: nivolumab versus docetaxel in previously treated non-small-cell lung cancer. J Clin Oncol. 2021;39:723–33. https://doi.org/10.1200/JCO.20.01605.
Li H, van der Merwe PA, Sivakumar S. Biomarkers of response to PD-1 pathway blockade. Br J Cancer. 2022;126:1663–75. https://doi.org/10.1038/s41416-022-01743-4.
Lee CK, Man J, Lord S, Links M, Gebski V, Mok T, et al. Checkpoint inhibitors in metastatic EGFR-mutated non-small cell lung cancer—a meta-analysis. J Thorac Oncol. 2017;12:403–7. https://doi.org/10.1016/j.jtho.2016.10.007.
Lisberg A, Cummings A, Goldman JW, Bornazyan K, Reese N, Wang T, et al. A phase II study of pembrolizumab in EGFR-mutant, PD-L1+, tyrosine kinase inhibitor naïve patients with advanced NSCLC. J Thorac Oncol. 2018;13:1138–45. https://doi.org/10.1016/j.jtho.2018.03.035.
Mazieres J, Drilon A, Lusque A, Mhanna L, Cortot AB, Mezquita L, et al. Immune checkpoint inhibitors for patients with advanced lung cancer and oncogenic driver alterations: results from the IMMUNOTARGET registry. Ann Oncol. 2019;30:1321–8. https://doi.org/10.1093/annonc/mdz167.
Negrao MV, Skoulidis F, Montesion M, Schulze K, Bara I, Shen V, et al. Oncogene-specific differences in tumor mutational burden, PD-L1 expression, and outcomes from immunotherapy in non-small cell lung cancer. J Immunother Cancer. 2021;9: e002891. https://doi.org/10.1136/jitc-2021-002891.
Dong Z-Y, Zhang J-T, Liu S-Y, Su J, Zhang C, Xie Z, et al. EGFR mutation correlates with uninflamed phenotype and weak immunogenicity, causing impaired response to PD-1 blockade in non-small cell lung cancer. OncoImmunology. 2017;6: e1356145. https://doi.org/10.1080/2162402X.2017.1356145.
Gainor JF, Shaw AT, Sequist LV, Fu X, Azzoli CG, Piotrowska Z, et al. EGFR mutations and ALK rearrangements are associated with low response rates to PD-1 pathway blockade in non-small cell lung cancer: a retrospective analysis. Clin Cancer Res. 2016;22:4585–93. https://doi.org/10.1158/1078-0432.CCR-15-3101.
Liu C, Zheng S, Jin R, Wang X, Wang F, Zang R, et al. The superior efficacy of anti-PD-1/PD-L1 immunotherapy in KRAS-mutant non-small cell lung cancer that correlates with an inflammatory phenotype and increased immunogenicity. Cancer Lett. 2020;470:95–105. https://doi.org/10.1016/j.canlet.2019.10.027.
García-González J, Ruiz-Bañobre J, Afonso-Afonso FJ, Amenedo-Gancedo M, Areses-Manrique MC, Campos-Balea B, et al. PD-(L)1 inhibitors in combination with chemotherapy as first-line treatment for non-small-cell lung cancer: a pairwise meta-analysis. J Clin Med. 2020;9:2093. https://doi.org/10.3390/jcm9072093.
Skoulidis F, Goldberg ME, Greenawalt DM, Hellmann MD, Awad MM, Gainor JF, et al. STK11/LKB1 mutations and PD-1 inhibitor resistance in KRAS-mutant lung adenocarcinoma. Cancer Discov. 2018;8:822–35. https://doi.org/10.1158/2159-8290.CD-18-0099.
Bai R, Lv Z, Xu D, Cui J. Predictive biomarkers for cancer immunotherapy with immune checkpoint inhibitors. Biomark Res. 2020;8:34. https://doi.org/10.1186/s40364-020-00209-0.
Gandhi L, Rodríguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F, et al. Pembrolizumab plus chemotherapy in metastatic non–small-cell lung cancer. N Engl J Med. 2018;378:2078–92. https://doi.org/10.1056/NEJMoa1801005.
Bracci L, Schiavoni G, Sistigu A, Belardelli F. Immune-based mechanisms of cytotoxic chemotherapy: implications for the design of novel and rationale-based combined treatments against cancer. Cell Death Differ. 2014;21:15–25. https://doi.org/10.1038/cdd.2013.67.
Hendriks LE, Kerr KM, Menis J, Mok TS, Nestle U, Passaro A, Peters S, Planchard D, et al. Oncogene-addicted metastatic non-small-cell lung cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. 2023;34:339–57. https://doi.org/10.1016/j.annonc.2022.12.009.
D’Haene N, Le Mercier M, De Nève N, Blanchard O, Delaunoy M, El Housni H, et al. Clinical validation of targeted next generation sequencing for colon and lung cancers. PLoS ONE. 2015;10: e0138245. https://doi.org/10.1371/journal.pone.0138245.
Descarpentries C, Leprêtre F, Escande F, Kherrouche Z, Figeac M, Sebda S, et al. Optimization of routine testing for MET exon 14 splice site mutations in NSCLC patients. J Thorac Oncol. 2018;13:1873–83. https://doi.org/10.1016/j.jtho.2018.08.2023.
Spigel DR, Ervin TJ, Ramlau RA, Daniel DB, Goldschmidt JH, Blumenschein GR, et al. Randomized phase II trial of onartuzumab in combination with erlotinib in patients with advanced non–small-cell lung cancer. JCO. 2013;31:4105–14. https://doi.org/10.1200/JCO.2012.47.4189.
Yin W, Cheng J, Tang Z, Toruner G, Hu S, Guo M, et al. MET amplification (MET/CEP7 ratio ≥ 1.8) is an independent poor prognostic marker in patients with treatment-naive non–small-cell lung cancer. Clin Lung Cancer. 2021;22:e512–8. https://doi.org/10.1016/j.cllc.2020.11.002.
Montrone M, Rosati G, Longo V, Catino A, Massafra R, Nardone A, et al. Immunotherapy in elderly patients affected by non-small cell lung cancer: a narrative review. J Clin Med. 2023;12:1833. https://doi.org/10.3390/jcm12051833.
Fujimoto D, Miura S, Yoshimura K, Wakuda K, Oya Y, Haratani K, et al. A real-world study on the effectiveness and safety of pembrolizumab plus chemotherapy for nonsquamous NSCLC. JTO Clin Res Rep. 2022;3: 100265. https://doi.org/10.1016/j.jtocrr.2021.100265.
Hayashi H, Sugawara S, Fukuda Y, Fujimoto D, Miura S, Ota K, et al. A randomized phase II study comparing nivolumab with carboplatin-pemetrexed for EGFR-mutated NSCLC with resistance to EGFR tyrosine kinase inhibitors (WJOG8515L). Clin Cancer Res. 2022;28:893–902. https://doi.org/10.1158/1078-0432.CCR-21-3194.
Lee HY, Ahn HK, Jeong JY, Kwon MJ, Han J-H, Sun J-M, et al. Favorable clinical outcomes of pemetrexed treatment in anaplastic lymphoma kinase positive non-small-cell lung cancer. Lung Cancer. 2013;79:40–5. https://doi.org/10.1016/j.lungcan.2012.10.002.
Shen C-I, Chao H-S, Shiao T-H, Chiang C-L, Huang H-C, Luo Y-H, et al. Comparison of the outcome between immunotherapy alone or in combination with chemotherapy in EGFR-mutant non-small cell lung cancer. Sci Rep. 2021;11:16122. https://doi.org/10.1038/s41598-021-95628-w.
Benjamin DJ, Chen S, Eldredge JB, Schokrpur S, Li D, Quan Z, et al. The role of chemotherapy plus immune checkpoint inhibitors in oncogenic-driven NSCLC: a university of California lung cancer consortium retrospective study. JTO Clin Res Rep. 2022;3: 100427. https://doi.org/10.1016/j.jtocrr.2022.100427.
Yang JC-H, Lee DH, Lee J-S, Fan Y, De Marinis F, et al. Pemetrexed and platinum with or without pembrolizumab for tyrosine kinase inhibitor (TKI)-resistant, EGFR -mutant, metastatic nonsquamous NSCLC: phase 3 KEYNOTE-789 study. JCO. 2023;41:LBA9000–LBA9000. https://doi.org/10.1200/JCO.2023.41.17_suppl.LBA9000.
Lu S, Wu L, Jian H, Cheng Y, Wang Q, Fang J, et al. Sintilimab plus chemotherapy for patients with EGFR-mutated non-squamous non-small-cell lung cancer with disease progression after EGFR tyrosine-kinase inhibitor therapy (ORIENT-31): second interim analysis from a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Respir Med. 2023;11(7):624-636. https://doi.org/10.1016/S2213-2600(23)00135-2.
Bylicki O, Tomasini P, Radj G, Guisier F, Monnet I, Ricordel C, Decroisette C, Greillier L. Atezolizumab with or without bevacizumab and platinum-pemetrexed in patients with stage IIIB/IV non-squamous non-small cell lung cancer with EGFR mutation, ALK rearrangement or ROS1 fusion progressing after targeted therapies: a multicentre phase II open-label non-randomised study GFPC 06-2018. Eur J Cancer. 2023;183:38–48. https://doi.org/10.1016/j.ejca.2023.01.014.
Reck M, Mok TSK, Nishio M, Jotte RM, Cappuzzo F, Orlandi F, et al. Atezolizumab plus bevacizumab and chemotherapy in non-small-cell lung cancer (IMpower150): key subgroup analyses of patients with EGFR mutations or baseline liver metastases in a randomised, open-label phase 3 trial. Lancet Respir Med. 2019;7:387–401. https://doi.org/10.1016/S2213-2600(19)30084-0.
Yu X, Ji X, Su C. HER2-altered non-small cell lung cancer: biology, clinicopathologic features, and emerging therapies. Front Oncol. 2022;12:860313. https://doi.org/10.3389/fonc.2022.860313.
Yang G, Yang Y, Liu R, Li W, Xu H, Hao X, et al. First-line immunotherapy or angiogenesis inhibitor plus chemotherapy for HER2-altered NSCLC: a retrospective real-world POLISH study. Ther Adv Med Oncol. 2022;14:17588359221082340. https://doi.org/10.1177/17588359221082339.
Saalfeld FC, Wenzel C, Christopoulos P, Merkelbach-Bruse S, Reissig TM, Laßmann S, et al. National network genomic medicine lung cancer (nNGM), efficacy of immune checkpoint inhibitors alone or in combination with chemotherapy in NSCLC harboring ERBB2 mutations. J Thorac Oncol. 2021;16:1952–8. https://doi.org/10.1016/j.jtho.2021.06.025.
Niu X, Sun Y, Planchard D, Chiu L, Bai J, Ai X, et al. Durable response to the combination of atezolizumab with platinum-based chemotherapy in an untreated non-smoking lung adenocarcinoma patient with BRAF V600E mutation: a case report. Front Oncol. 2021;11: 634920. https://doi.org/10.3389/fonc.2021.634920.
Seegobin K, Majeed U, Wiest N, Manochakian R, Lou Y, Zhao Y. Immunotherapy in non-small cell lung cancer with actionable mutations other than EGFR. Front Oncol. 2021;11: 750657. https://doi.org/10.3389/fonc.2021.750657.
Saigi M, Alburquerque-Bejar JJ, Mc Leer-Florin A, Pereira C, Pros E, Romero OA, et al. MET-oncogenic and JAK2-inactivating alterations are independent factors that affect regulation of PD-L1 expression in lung cancer. Clin Cancer Res. 2018;24:4579–87. https://doi.org/10.1158/1078-0432.ccr-18-0267.
Titmarsh HF, O’Connor R, Dhaliwal K, Akram AR. The emerging role of the c-MET-HGF axis in non-small cell lung cancer tumor immunology and immunotherapy. Front Oncol. 2020;10:54. https://doi.org/10.3389/fonc.2020.00054.
Morimoto K, Yamada T, Yokoi T, Kijima T, Goto Y, Nakao A, et al. Clinical impact of pembrolizumab combined with chemotherapy in elderly patients with advanced non-small-cell lung cancer. Lung Cancer. 2021;161:26–33. https://doi.org/10.1016/j.lungcan.2021.08.015.
Kim JH, Kim HS, Kim BJ. Prognostic value of KRAS mutation in advanced non-small-cell lung cancer treated with immune checkpoint inhibitors: a meta-analysis and review. Oncotarget. 2017;8:48248–52. https://doi.org/10.18632/oncotarget.17594.
Landre T, Justeau G, Assié J-B, Chouahnia K, Davoine C, Taleb C, et al. Anti-PD-(L)1 for KRAS-mutant advanced non-small-cell lung cancers: a meta-analysis of randomized-controlled trials. Cancer Immunol Immunother. 2022;71:719–26. https://doi.org/10.1007/s00262-021-03031-1.
Gadgeel S, Rodriguez-Abreu D, Felip E, Esteban E, Speranza G, Reck M, et al. LBA5-KRAS mutational status and efficacy in KEYNOTE-189: pembrolizumab (pembro) plus chemotherapy (chemo) vs placebo plus chemo as first-line therapy for metastatic non-squamous NSCLC. Ann Oncol. 2019;30:xi64–xi65. https://doi.org/10.1093/annonc/mdz453.002.
West HJ, McCleland M, Cappuzzo F, Reck M, Mok TS, Jotte RM, et al. Clinical efficacy of atezolizumab plus bevacizumab and chemotherapy in KRAS-mutated non-small cell lung cancer with STK11, KEAP1, or TP53 comutations: subgroup results from the phase III IMpower150 trial. J Immunother Cancer. 2022;10: e003027. https://doi.org/10.1136/jitc-2021-003027.
Federico AD, Giglio AD, Parisi C, Gelsomino F. STK11/LKB1 and KEAP1 mutations in non-small cell lung cancer: prognostic rather than predictive? Eur J Cancer. 2021;157:108–13. https://doi.org/10.1016/j.ejca.2021.08.011.
Assoun S, Theou-Anton N, Nguenang M, Cazes A, Danel C, Abbar B, et al. Association of TP53 mutations with response and longer survival under immune checkpoint inhibitors in advanced non-small-cell lung cancer. Lung Cancer. 2019;132:65–71. https://doi.org/10.1016/j.lungcan.2019.04.005.
Dong Z-Y, Zhong W-Z, Zhang X-C, Su J, Xie Z, Liu S-Y, et al. Potential predictive value of TP53 and KRAS mutation status for response to PD-1 blockade immunotherapy in lung adenocarcinoma. Clin Cancer Res. 2017;23:3012–24. https://doi.org/10.1158/1078-0432.CCR-16-2554.
Pyo J-S, Kang G, Cho WJ, Choi SB. Clinicopathological significance and concordance analysis of c-MET immunohistochemistry in non-small cell lung cancers: a meta-analysis. Pathol Res Pract. 2016;212:710–6. https://doi.org/10.1016/j.prp.2016.05.006.
Yoshimura K, Inoue Y, Tsuchiya K, Karayama M, Yamada H, Iwashita Y, et al. Elucidation of the relationships of MET protein expression and gene copy number status with PD-L1 expression and the immune microenvironment in non-small cell lung cancer. Lung Cancer. 2020;141:21–31. https://doi.org/10.1016/j.lungcan.2020.01.005.
Watermann I, Schmitt B, Stellmacher F, Müller J, Gaber R, Kugler C, et al. Improved diagnostics targeting c-MET in non-small cell lung cancer: expression, amplification and activation? Diagn Pathol. 2015;10:130. https://doi.org/10.1186/s13000-015-0362-5.
Spigel DR, Edelman MJ, O’Byrne K, Paz-Ares L, Mocci S, Phan S, et al. Results from the phase III randomized trial of onartuzumab plus erlotinib versus erlotinib in previously treated stage IIIB or IV non-small-cell lung cancer: METLung. J Clin Oncol. 2017;35:412–20. https://doi.org/10.1200/JCO.2016.69.2160.
Drilon A, Cappuzzo F, Ou S-HI, Camidge DR. Targeting MET in lung cancer: will expectations finally be MET? J Thorac Oncol. 2017;12:15–26. https://doi.org/10.1016/j.jtho.2016.10.014.
Acknowledgements
The authors thank E. Wasielewski for his help in setting up this study and K. Broman for providing language help.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflict of interest
A.B.C. has received research grants (paid to institution) from Merck; consulting fees from Novartis and Roche; a speaker honorarium from Astra-Zeneca, BMS, MSD, Pfizer, Novartis, Takeda, Janssen, Roche, Abbvie, Amgen, and Exeliom; support from Pfizer, Novartis, and MSD to attend meetings; and has served on advisory boards for Novartis and InhaTarget. V.L. has received a speaker honorarium from Novartis, Astra-Zeneca and MSD. E.D. has received a speaker honorarium from Novartis. M.M., H.B., N.P., S.B., S.H., F.E., and G.C. declare that they have no conflicts of interest that might be relevant to the contents of this manuscript.
Ethics approval
This retrospective, non-interventional study was conducted in compliance with GDPR (EU General Data Protection Regulation) and MR004 (Reference Methodology 004 for data protection) and was approved by the Data Protection Officer of GHT (Territorial Hospital Group) Lille Métropole Flandre Intérieure, registered under ID 865.
Consent to participate
Not applicable due to the retrospective nature of the study. The patients were informed, by a mention in medical letters, of treatment of their data for research purposes. The local databases and medical files were searched for any potential refusal of additional data treatment.
Consent for publication
All authors gave their consent for publication.
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
M.M. and A.B.C. contributed to the study conception and design, data collection, and analyses. Statistical analyses were carried out by H.B. Early versions of the manuscript were drafted by M.M. and A.B.C. All authors provided feedback on the manuscript and have read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Marchal, M., Leroy, V., Behal, H. et al. Histo-Molecular Factors of Response to Combined Chemotherapy and Immunotherapy in Non-Small Cell Lung Cancers. Targ Oncol 18, 927–939 (2023). https://doi.org/10.1007/s11523-023-01009-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-023-01009-w