Abstract
Background
There is growing evidence supporting multidisciplinary molecular tumor boards (MTB) in solid tumors whereas hematologic malignancies remain underrepresented in this regard.
Objective
The present study aimed to assess the clinical relevance of MTBs in primary refractory diffuse large B-cell lymphomas/high-grade B-cell lymphomas with MYC and BCL2 rearrangements (prDLBCL/HGBL-MYC/BCL2) (n = 13) and HGBL, not otherwise specified (NOS), with MYC and BCL6 rearrangements (prHGBL, NOS-MYC/BCL6) (n = 6) based on our previously published whole-exome sequencing (WES) cohort.
Patients and Methods
For genomic analysis, the institutional MTB WES pipeline (University Cancer Center Schleswig-Holstein: UCCSH), certified for routine clinical diagnostics, was employed and supplemented by a comprehensive immunohistochemical work-up. Consecutive database research and annotation according to established evidence levels for molecularly stratified therapies was performed (NCT-DKTK/ESCAT).
Results
Molecularly tailored treatment options with NCT-DKTK evidence level of at least m2A were identified in each case. We classified mutations in accordance with biomarker/treatment baskets and detected a heterogeneous spectrum of targetable alterations affecting immune evasion (IE; n = 30), B-cell targets (BCT; n = 26), DNA damage repair (DDR; n = 20), tyrosine kinases (TK; n = 13), cell cycle (CC; n = 7), PI3K-MTOR-AKT pathway (PAM; n = 2), RAF-MEK-ERK cascade (RME; n = 1), and others (OTH; n = 11).
Conclusion
Our virtual MTB approach identified potential molecularly targeted treatment options alongside targetable genomic signatures for both prDLBCL/HGBL-MYC/BCL2 and prHGBL, NOS-MYC/BCL6. These results underline the potential of MTB consultations in difficult-to-treat lymphomas early in the treatment sequence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The approach of a virtual molecular tumor board (MTB) reveals a vast potential for molecularly stratified treatment options with reasonable molecular evidence levels in primary refractory cases of diffuse large B-cell lymphomas/high-grade B-cell lymphomas (HGBL) with MYC and BCL2 and HGBL, not otherwise specified, with MYC and BCL6 rearrangements beyond the spectrum of standard treatment strategies. |
Addressing an urgent unmet medical need, the present study aims to draw attention to the potential benefits of a more frequent inclusion of rare hematologic malignancies in MTB settings. |
1 Introduction
The 5th edition of the World Health Organization Classification of Haematolymphoid Tumors (WHO-HAEM5) took recent findings concerning a distinctive mutational pathogenesis as well as gene expression signatures into account and renewed the former provisional entity of high-grade B-cell lymphomas with MYC and BCL2 and/or BCL6 rearrangements (HGBL-DH/TH) [1,2,3,4]. The novel term is diffuse large B-cell lymphoma/high-grade B-cell lymphoma with MYC and BCL2 rearrangements (DLBCL/HGBL-MYC/BCL2). Lymphomas with dual MYC and BCL6 rearrangements were excluded and are now classified either as DLBCL, not otherwise specified (NOS) or HGBL, NOS based on cytomorphologic characteristics [1]. However, there still exists a relevant subset of aggressive B-cell non-Hodgkin lymphoma (B-NHL) cases harboring both MYC and BCL6 rearrangements presenting with insufficient response rates to standard immunochemotherapy and poor prognosis [3]. Such cases as well as DLBCL/HGBL-MYC/BCL2 affiliate to a spectrum of difficult-to-treat aggressive B-NHL.
Recent advances in oncology include the comprehensive implementation of multidisciplinary molecular tumor boards (MTB) moving from omnidirectional and unspecific to personalized and targeted treatment strategies. In congruence, recent advances in genomic profiling and increasing availability of such complex diagnostics led to rapid development of novel molecularly targeted therapeutics in cancer patients [5, 6]. However, there is still room for improvement as recommended treatments can be realized only in a small fraction of cases due to prolonged turn-around periods for molecular diagnostic workups, rapid progression of the disease, or limited performance status after heavy pretreatments [6]. Moreover, the performance of molecular diagnostics and the procedure for communicating MTB recommendations is still not well standardized [7, 8]. As the majority of molecularly stratified treatment options are not covered by health insurances, meeting the costs of individual treatments represents a common challenge in the realization of MTB recommendations [9].
Major publications reporting on MTB approaches reveal a disproportionally low representation of hematologic malignancies, as MTB activities focus on solid tumors to a great extent [6, 10]. In concert with expanding publicly available datasets in repositories and growing experience regarding molecularly stratified therapies, clinical outcomes in personalized treatment strategies are continually improving [11].
Comprehensive genomic profiling decisively refined the taxonomy and uncovered potential therapeutic vulnerabilities in a relevant fraction of the aforementioned difficult-to-treat entities across the spectrum of hematologic malignancies such as primary refractory (pr) DLBCL/HGBL-MYC/BCL2 and DLBCL/HGBL, NOS. Dismal prognosis in such cases is explained by extraordinarily aggressive tumor biology, underlining the urgent yet unmet clinical need for the expansion of treatment strategies.
Applying the institutional MTB whole-exome sequencing (WES) pipeline (University Cancer Center Schleswig-Holstein; UCCSH), which is certified for routine clinical diagnostics, the present study aimed to evaluate 19 cases with prDLBCL/HGBL-MYC/BCL2 and prDLBCL/HGBL, NOS from a previous study by our group from the precision hematologist’s perspective in a virtual MTB setting [2, 12]. MTB recommendations for immunologically and/or molecularly stratified treatment options were generated based on WES data. Each potential target was individually annotated in the light of recurrence and therapeutic addressability.
2 Patients and Methods
2.1 Study Design and Patient Characteristics
Corresponding to the 4th edition of the WHO Classification of Tumors of the Haematopoietic and Lymphoid Tissue (WHO-HAEM4), our institutional database was screened for the provisional entity high-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangement (HGBL-DH/TH) within the scope of this retrospective proof-of-concept study [13]. From our previously published WES cohort, re-screening identified 19 cases with primary-refractory disease indicating potential benefits from the application of a virtual MTB approach. All cases were redefined in accordance with the latest version of the WHO-HAEM5 in December 2022.
2.2 Genomic Analysis
Sample preparation and WES from formalin-fixed, paraffin-embedded (FFPE) tissue sections in addition to bioinformatic data processing (raw data preparation, filtering, the detection of single-nucleotide variants [SNV], short insertions and deletions [indels] and somatic copy number aberrations [SCNA]) were performed as previously published by Künstner et al. [2]. The median coverage was 234× (standard deviation ± 195×; average depth of 304×). Quality-filtered sequencing data was mapped against the human reference genome (hg19) using the Medical Informatics for Research and Care in University Medicine (MIRACUM) pipeline. The certified institutional UCCSH MTB pipeline comprises several steps of bioinformatic analysis, which are described below.
2.3 Molecular Tumor Board (MTB) Data Preparation
MTB database research standardized genomic reports, provided by the Medical Systems Biology Group (University of Luebeck), were constituted individually for each case upon MIRACUM pipeline analysis. Individual genomic reports provided information on tumor mutational burden (TMB), the tumor heterogeneity based on tumor subclones, the percentual content of tumor cells, the variant allele frequency (VAF) for each genomic alteration, microsatellite instability (MSI) status, the result of BRCAness calculation (cut-off ≥ 20%) and combined annotation dependent depletion (CADD) phred-score calculation (cut-off > 20) as this score indicates the deleteriousness of an alteration. A detailed description of bioinformatics, especially filtering processes, is provided in the Electronic Supplementary Material (ESM).
2.4 MTB Annotation and Data Analysis
First, the databases COSMIC, OncoKB (prognostic and diagnostic levels), ClinVar (clinically relevant variation), and cBioPortal were applied in order to approve the recurrence of a genomic alteration. Second, ProteinPaint was exerted to check the functional relevance of an alteration. Third, the therapeutic vulnerability was annotated for each recurrent alteration of functional relevance by means of the databases CIVIC, OncoKB (therapeutic and FDA levels), the Cancer Genome Interpreter (CGI), and the Drug–Gene Interaction database (DGIdb). Additional potential therapeutic targets identified by MSI status, BRCAness scoring or immunotherapeutic rationales based on high TMB status (≥10 mut/Mb) were similarly checked. Molecularly stratified treatment options were allocated to evidence levels in accordance with the National Center for Tumor Diseases/German Cancer Consortium NCT/DKTK-MASTER program (Supplementary Fig. 1, see ESM) and with the European Society for Medical Oncology Scale for Actionability of Molecular Targets (ESCAT; Supplementary Fig. 2, see ESM) [14, 15]. For targets amenable to multiple agents, we favored agents with the highest level of evidence according to the NCT/DKTK classification. As proposed by Horak et al., annotated genomic alterations were classified by biomarker/treatment baskets [6].
Finally, ongoing trials were checked if no treatment recommendation was available for a recurrent and functionally relevant alteration (https://clinicaltrials.gov). Alternatively, literature was evaluated for preclinical evidence of targetable vulnerabilities corresponding to DKTK levels m3/4. Only resources open for academic research purposes were considered for MTB recommendations.
2.5 Prioritization of Therapeutic Vulnerabilities
The prioritization of potential molecularly stratified treatment options simultaneously considers several variables and therefore represents a multifactorial process. Genomic alterations were assessed in regard to their biological relevance and conclusiveness based on CADD score calculation, VAF and gene-set enrichment analysis. Variants of unknown significance were excluded from further analyses unless such variants were associated with high CADD scores or functional relevance. Each recommended drug was either approved by the US Food and Drug Administration (FDA) and/or European Medicines Agency (EMA) or at least designated for FDA fast-track development as a minimum requirement for consideration within the scope of this study (cutoff date 1 February 2023). More detailed information on the treatment prioritization process including the calculation of a modified Matching Score (mMS) is provided in Supplementary Table 1 (see ESM). Potential drug combinations were evaluated in accordance with the I-PREDICT study by Sicklick et al. [28] and screened for potential drug interactions by the attending pharmacist.
2.6 Virtual MTB Setting
In accordance with the institutional standards of UCCSH, four rounds of virtual multidisciplinary MTB were performed in which 19 prDLBCL/HGBL-MYC/BCL2 and prDLBCL/HGBL, NOS cases were retrospectively discussed (first to third round: 5 cases; fourth round: 4 cases). The four conferences were conducted on the virtual meeting platform ‘VidyoConnect’ (VidyoInc., Hackensack, New Jersey; United States). A conference was quorate if a molecular oncologist, a bioinformatician, a pathologist, and a pharmacist were present. This fundamental requirement was equivalent to the conventional MTB setting. Decision making for each case reflected a multifactorial process based on molecular diagnostics, performance status, prior therapies, and prioritization of therapeutic vulnerabilities in light of drug approval and data on the efficacy for each drug (see also Sect. 2.5). This process was also equivalent to the routine clinical MTB setting. As the required information for each case was collected prior to the conference, each case had to be comprehensively reconstituted in one session starting from case presentation right up to MTB treatment recommendations. Centralized documentation of MTB recommendations was conducted in each case analogue to the conventional MTB setting. Figure 1 illustrates the detailed workflow of our virtual MTB.
Virtual UCCSH MTB workflow for primary refractory diffuse large B-cell lymphomas/high-grade B-cell lymphomas with MYC and BCL2 aberrations (prDLBCL/HGBL-MYC/BCL2) and prDLBCL/HGBL, NOS with MYC and BCL6 rearrangements. After institutional case selection, academic WES was performed in 47 cases. Consecutively, 19 primary-refractory cases were identified and underwent UCCSH MTB pipeline evaluation. Afterward, manual database research annotation was conducted for each relevant variant. In a virtual MTB setting, each prDLBCL/HGBL-MYC/BCL2 and prDLBCL/HGBL, NOS case with MYC/BCL6 was discussed. Potential therapeutic vulnerabilities were allocated to molecular evidence levels and to treatment baskets. A multifactorial treatment prioritization process guided MTB treatment recommendations. MTB molecular tumor board, NOS not otherwise specified, UCCSH University Cancer Center Schleswig-Holstein, WES whole-exome sequencing
2.7 Data Availability
Data used in this study were downloaded from the European genome-phenome archive (EGA) accession number EGAS00001005420.
2.8 Ethics Statement
This retrospective study was approved by the ethics committee of the University of Lübeck (reference no. 18-356), conducted in accordance with the Declaration of Helsinki, and patients provided written informed consent regarding routine diagnostic and academic investigations, including genomic studies of their biopsy specimen as well as the transfer of their clinical data.
3 Results
3.1 Baseline Clinicopathological Characteristics
In total, we report on 19 patients with prDLBCL/HGBL-MYC/BCL2 and prDLBCL/HGBL, NOS (former HGBL-DH/TH), carving out the potential of a virtual MTB approach. The median age was 72.0 years (range 35–79) with a pronounced male predominance (74%). Additional DLBCL/HGBL-MYC/BCL2 and DLBCL/HGBL, NOS cases responding to initial cytoreductive treatment served as a comparison cohort (n = 28) [2]. The course of the disease, information on clinical characteristics, and treatment sequences for each case are shown in Fig. 2a. Survival analysis by means of the Kaplan–Meier method revealed significantly inferior progression-free survival (p < 0.0001) and overall survival (p = 0.0086) in primary refractory (pr) cases compared with those cases responding to first-line treatment (Fig. 2b/c).
Clinical features in primary refractory diffuse large B-cell lymphomas/high-grade B-cell lymphomas with MYC and BCL2 aberrations (prDLBCL/HGBL-MYC/BCL2) and prDLBCL/HGBL, NOS with MYC/BCL6. a The swimmer plot illustrates the clinical course of the disease for each primary-refractory case. b, c Kaplan Meier survival analysis (PFS and OS) comparing primary-refractory cases and the comparison cohort which were not associated with primary refractory disease. NOS not otherwise specified, OS overall survival, PFS progression-free survival
Baseline clinicopathological characteristics including treatment modalities and toxicity profiles according to common toxicity criteria adverse events (CTCAE 6.0) are summarized in Table 1, differentiating between prDLBCL/HGBL-MYC/BCL2 and prDLBCL/HGBL, NOS (including dual MYC/BCL6 rearrangements) in accordance with WHO-HAEM5.
3.2 Whole Exome Profiling
WES analysis identified 2433 missense mutations, 1025 in-frame mutations, 179 nonsense mutations as well as 179 frame-shift mutations (indels) and 82 splice-site mutations after variant filtering. In total, 1126 mutations (28.9%) were found to be functionally relevant based on exhaustive database research, whereas 2098 mutations (53.8%) were inconclusive and functional neutrality was annotated for 675 mutations (17.3%) (Fig. 3a). The median TMB was comparable (low to intermediate levels) between patients with primary refractory disease and patients from the comparison cohort (Table 1; Fig. 3b). A high TMB status (18.2 mut/Mb) was detected in a single case from the comparison cohort. To evaluate significantly (p < 0.05) distinct features between both subgroups, an enrichment analysis (groupwise Fisher exact testing) was performed resulting in three genomic events (GLE1, ODF2, SPTAN1) that were predominantly altered in primary responders, and seven alterations (C2orf77, FASTKD1, KLHL23, METTL5, PHOSPHO2, PHOSPHO2-KLHL23, SSB) that were almost exclusively detected in primary refractory cases (Supplementary Figure 3, see ESM). As expected, and previously reported by our group, the application of the LymphGen algorithm proposed by Wright et al. allocated 13 prDLBCL/HGBL-MYC/BCL2 cases to the C3/EZB cluster, three prDLBCL/HGBL, NOS cases to the C1/BN2 cluster and the remaining three cases were unclassifiable [2, 16]. The predominant mutational signatures were associated with spontaneous deamination (AC1) and DNA MMR (AC26) (Fig. 3c, Supplementary Table 2, see ESM) [17]. In line with previous results considering other hematologic malignancies, we did not detect any evidence of MSI-related hypermutations regardless of the availability of germline-paired tissues (available in two cases).
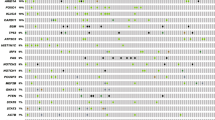
Genomic features and results from manual database research and annotation of relevant genomic alterations in primary refractory diffuse large B-cell lymphomas/high-grade B-cell lymphomas with MYC and BCL2 aberrations (prDLBCL/HGBL-MYC/BCL2) and prDLBCL/HGBL, NOS with MYC/BCL6. a Pie charts outlining functionality, the mutational subtype and the mechanism of detected mutations. b Comparative median TMB calculation between primary-refractory cases and the comparison group. c Bar plot visualizes predominant mutational signatures in primary-refractory cases. d Oncoprint summarizes targetable driver mutations detected upon MIRACUM pipeline analysis and potential therapeutic options. e Case-related summary of MTB recommendations and associated molecular evidence levels according to National Center for Tumor Diseases/German Cancer Consortium (NCT/DKTK) and European Society for Medical Oncology Scale for Actionability of Molecular Targets (ESCAT) tiers. f Bar plot visualizing the status of approval for annotated therapeutic options. g Sankey plot assigning molecular evidence levels to treatment baskets. h Sankey plot allocating patients dependent on the assigned genomic cluster (BN2 vs EZB vs other). The plot shows the best response of primary-refractory patients after standard (immune) chemotherapy. Moreover, the Sankey plot illustrates therapeutic vulnerabilities beyond standard chemotherapy based on genomic alterations. TMB tumor mutational burden
3.3 Rationale 1: Annotation of Genomic Alterations
Applying the MIRACUM pipeline revealed 111 relevant driver mutations carried by 44 genes in the 19 pr-cases. Comprehensive database research led to the assignment of 91 potential treatment recommendations involving 73 variants across 23 genes. An additional 16 treatment options were recommended based on genomic clusters (3 = BN2 cluster; 13 = EZB cluster). For the C1/BN2 cluster, the recommendation of ibrutinib in combination with R-CHOP is only relevant in cases that were not treated with an R-CHOP-based regimen in the first-line setting or when a molecular characterization is performed early on and a molecularly tailored add-on therapy can be recommended. This recommendation is based on results reported from the subsequent PHOENIX trial subgroup analysis and preliminary results presented by Zhang et al. [18,19,20]. Unfortunately, other regimens containing ibrutinib such as the combination with lenalidomide and rituximab (iR2) did not stratify according to genomic subtypes [21]. Upon personalized annotation of therapeutic vulnerabilities, the spectrum of targeted therapeutics was heterogeneous, involving novel agents such as futibatinib, tazemetostat or defactinib and well established drugs such as venetoclax, afatinib as well as ivosidenib. Results from MIRACUM pipeline analysis and individual database research are shown in Fig. 3d, e. FDA approval was available for 15 agents, EMA approval for 14 agents, and 7 agents were designated for FDA fast-track development (Fig. 3f). The spectrum of MTB treatment recommendations is summarized in Table 2. The median mMS was 60%, ranging from 27 to 100%. In the majority of cases, an mMS ≥ 50% was calculated (84%) (Supplementary Table 3, see ESM).
3.4 Rationale 2: Immunotherapy and PARP Inhibition
Immunotherapeutic strategies were recommended for mutations that were previously associated with an objective response towards such agents (KMT2A, KMT2C, KMT2D, ROS1, PARP1) in vivo or in vitro [22,23,24,25]. There was no case with a high TMB status (≥ 10 mut/Mb) among prDLBCL/HGBL-MYC/BCL2 and prDLBCL/HGBL, NOS cases.
A rationale for the recommendation of PARP inhibitors was made based on a pathological BRCAness score which was found in one case (39.9% of mutations affecting homologous recombination deficiency [HRD], AC3 signature). In 15/19 cases we found a fraction of mutations associated with the AC3 signature. However, in the majority of cases, the 20% cut-off leading to a PARP inhibitor rationale was not reached. Similar to immunotherapeutic recommendations, PARP inhibition seemed feasible in cases presenting with mutations for which an objective response was previously demonstrated (KMT2C, RB1) in vivo or in vitro [26, 27]. All recommendations for immunotherapy and PARP inhibitors are outlined in Table 2.
3.5 Rationale 3: Drug Combinations
Recent studies aimed to advance MTB recommendations originating concepts for drug combinations [28]. Here, drug combinations would be preferred if available datasets existed, demonstrating their feasibility and effectiveness in a specific tumor type or in basket trials (18/19 cases; 95%; Supplementary Table 4, see ESM). For novel drug combinations, several considerations were taken into account including the availability of involved agents, their molecular evidence levels (mEL), and overlapping toxicities. In total, our database research revealed 40 potential drug combinations expanding the spectrum of MTB recommendations. In particular, immunotherapeutic agents represent promising combination partners (involved in 11/40 potential combinations; 27.5%) as several standard treatment strategies include such agents among a broad spectrum of malignancies [29, 30].
3.6 Molecular Evidence Levels (NCT/DKTK and ESCAT)
The procedure of individual annotations for each genetic alteration detected by WES in this difficult-to-treat entity included the allocation to mEL according to NCT/DKTK recommendations of at least m3 and ESCAT tier IV. Among the 107 potential MTB recommendations, 16 therapeutic options were assigned to m1A (n = 10; 10.9%) or m1B (n = 6; 6.6%) rationales, respectively. The majority of MTB recommendations were allocated to NCT/DKTK mEL m2A (n = 26; 28.6%), m2B (n = 32; 35.2%), and m2C (n = 5; 5.5%). Moreover, 31 recommendations were based on preclinical data (NCT/DKTK m3 and ESCAT-tier IVA/B; 34.1%). According to ESCAT, our proof-of-concept approach assigned 27 recommendations to tier I (IA: n = 7, 7.7%; IB: n = 3, 3.3%; IC: n = 17, 18.7%), six recommendations to tier IIA (6.6%) and 46 recommendations to tier IIIA (50.5%). The low frequency of high mEL (NCT/DKTK m1A-C and ESCAT IA-C) reflects the lack of molecularly stratified clinical trials in patients with hematologic malignancies. Biologic rationales (NCT/DKTK m4) or current developments (ESCAT tier V) were not considered in the present cohort.
3.7 Assignment to Therapeutic Baskets
The drug’s mechanism of action rather than its functionality was the decisive factor for the assignment to a treatment basket. According to baskets, MTB recommendations were allocated to DNA damage repair (DDR; n = 20), immune evasion (IE; n = 30), cell cycle (CC; n = 7), tyrosine kinases (TK; n = 13), PI3K-MTOR-AKT pathway (PAM; n = 2), RAF-MEK-ERK cascade (RME; n = 1), and others (OTH; n = 11). Due to their specific genomic features, we added another treatment basket called B-cell targets (BCT; n = 26), which was one of the predominant baskets upon allocation (Fig. 3g; Supplementary Fig. 4, see ESM).
3.8 Virtual MTB Recommendations
The turnaround time from genomic diagnostics (WES) to virtual MTB recommendations was at least 3 weeks. The virtual MTB focused on the recommendation of treatment options but not additional diagnostics. Across the 19 prDLBCL/HGBL-MYC/BCL2 and prDLBCL/HGBL, NOS cases, the application of the standardized institutional UCCSH-MTB pipeline revealed 91 potential MTB recommendations upon a multifactorial treatment prioritization process. Molecularly stratified treatment recommendations were identified in each case. According to NCT/DKTK mEL and ESCAT tiers, the spectrum of MTB recommendations ranged from m3 to m1A rationales and from IVB to IA rationales, respectively. Among the entire cohort, our virtual approach identified a median of six MTB recommendations (range 3–9). Interestingly, the allocation to treatment baskets was extraordinarily heterogeneous and highlights the broad range of additional treatment options in a virtual second-line setting and the relevance of molecular diagnostics in rare and/or difficult-to-treat hematologic malignancies (Fig. 3h). Additionally, we provide an overview of alternative agents in Supplementary Table 5 (see ESM).
3.9 Review of Literature: Efficacy of Targeted Therapeutics in Non-Hodgkin B-Cell Lymphomas
Irrespective of a molecularly stratified intention, each recommended drug from our virtual MTB approach was screened for its effectiveness or its therapeutic potential based on preclinical data in non-Hodgkin B-cell lymphomas in a review of literature. In total, MTB recommendations included 20 different agents. For the review of literature, the databases Google Scholar (https://scholar.google.com), PubMed (https://pubmed.ncbi.nlm.nih.gov) and ClinicalTrials.gov (https://clinicaltrials.gov) were examined using the keywords ‘lymphoma’, ‘DLBCL’, ‘HGBL’, ‘aggressive lymphoma’, ‘B-cell non-Hodgkin lymphoma’, ‘phase I’, ‘phase II’, ‘phase III’ in combination with the name of each of the 20 drugs. For nine agents (45%), the review of literature revealed datasets indicating the efficacy against non-Hodgkin B-cell lymphomas. However, for 11 agents, efficacy data from solid tumors was extrapolated to the spectrum of hematologic malignancies. Three datasets report on the preclinical activity of napabucasin, eprenetapopt, and the combination of tazemetostat and venetoclax. Currently, an ongoing phase I trial is investigating the efficacy of tazemetostat and venetoclax in DLCBL/HGBL (ClinicalTrials.gov identifier: NCT05618366). Results from the review of literature are summarized in Supplementary Tables 6 and 7 (see ESM).
4 Discussion
Recent insights into the genomic landscape of DLBCL/HGBL-MYC/BCL2 and DLBCL/HGBL, NOS revealed several potential therapeutic vulnerabilities beyond standard R-CHO(E)P-based immunochemotherapy and resulted in the allocation to genomic clusters defined via the LymphGen algorithm by Wright et al. based on distinct molecular signatures [2, 3, 16]. In the primary-refractory setting, therapeutic options beyond standard immunochemotherapy are limited and oftentimes not applicable as a relevant subset of patients is not eligible for intensive treatments. This constitutes an urgent unmet medical need across the spectrum of rare and difficult-to-treat hematologic malignancies that potentially can be addressed by means of a more frequent integration into precision medicine efforts. Our findings provide evidence that the application of a certified MTB pipeline for patients presenting with prDLBCL/HGBL-MYC/BCL2 and prDLBCL/HGBL, NOS appeared to be feasible as molecularly stratified treatment recommendations were identified for each case.
The spectrum of molecularly stratified treatment options is steadily increasing and novel agents progressively enter the market, elevating the number of FDA (US) and/or EMA (Europe) drug approvals. However, the vast majority of MTB recommendations are related to solid tumors [6, 31]. As evidence for novel and innovative targeted treatment options in the era of precision oncology is rapidly growing, improvements such as the standardized integration of RNA-seq data into MTB decision making or comprehensive regulation regarding the performance of next-generation sequencing (NGS) approaches aiming to reduce heterogeneous MTB recommendations and to harmonize proceedings in University Cancer Centers are urgently required. The infrequent appearance of MTB introductions of patients with hematologic malignancies is accompanied by a lack of suitable basket trials for such tumors. Consecutively, findings from solid tumors gathered from MTBs are mostly extrapolated into the spectrum of hematologic malignancies, which leads to limited molecular evidence not exceeding m2A levels according to NCT/DKTK or ESCAT tier IIIA according to ESCAT recommendations. Additionally, the majority of MTB recommendations and ongoing basket trials consider the applicability of single agents targeting a single molecular vulnerability. Aggressive hematologic diseases such as DLBCL/HGBL-MYC/BCL2 and DLBCL/HGBL, NOS are hardly manageable through the administration of single-agent targeted therapeutics. Therefore, future treatment strategies in such settings respecting the molecular background of the disease must incorporate combination therapies or a predefined immunochemotherapeutic backbone to control the disease [20]. Accordingly, we favored combination therapies in our approach, if applicable.
Another open question that needs to be addressed in future trials is the transferability into the lymphoma setting of established biomarkers associated with designated MTB rationales from solid tumors such as immunotherapy in tumors harboring DNA MMR mutational signatures or PARP inhibition in neoplasms with HRD deficiency [15, 32].
The comparative enrichment analysis revealed ten genomic events that were differentially altered between primary refractory cases and those that responded to initial cytoreductive treatment. Ajorloo et al. reported SPTAN1, which was found to be altered most exclusively in responders corresponding to our dataset, to reflect a potential treatment target in non-Hodgkin lymphomas based on autoantibody profiling [33]. According to literature, none of the other nine alterations were previously associated with the occurrence of lymphomas. However, such alterations seem to play a role that is exceptionally restricted to lymphoma biology without any relevance for MTB treatment recommendations.
Keeping the timeframe between initial diagnosis/relapse/refractory setting and MTB recommendation as short as possible poses a relevant challenge concerning the realization of MTBs, as genomic profiling requires a few weeks depending on the availability, the workload, and the NGS method. In light of the MIRACUM consortium, the implementation of the UCCSH MTB pipeline which is certified for routine clinical diagnostics allows an efficient bioinformation workload. However, essentially, all processes included in the molecular work-up had to be streamlined starting from sample preparation alongside the performance of whole exome sequencing right up to the annotation of genomic findings and the translation into standardized treatment recommendations in order for the program to succeed. Nevertheless, there is still room for further improvement and this raises the question regarding the optimal moment of MTB introduction for potential candidates. Preferentially, we recommend the introduction of a potential candidate after the first evaluation of response in terms of interim positron emission tomography (PET2) [34]. This strategy tries to anticipate early relapses or refractory diseases in high-risk settings and helps to overcome time pressures in molecular diagnostics. To further optimize this strategy, it is necessary to improve tools for optimal risk stratification in aggressive B-cell lymphomas. However, the spectrum of approved and effective second-line treatment options in the setting of aggressive B-cell lymphoma relapse has steadily increased in recent years. In this setting, the option of chimeric antigen receptor (CAR) T-cell therapy poses a novel effective strategy even in a relevant fraction of patients who are ineligible for autologous hematopoietic stem cell transplantation (AutoHSCT) [35, 36]. The present study aimed to uncover further treatment options beyond approved strategies. Therefore, we recommend molecularly stratified therapies after treatment failures of approved options or in patients who are ineligible for CAR T-cell therapies or other approved options.
Predictably, early MTB introductions for extended diagnostics such as genomic profiling promise to be cost effective as MTB-related diagnostics are responsible for a fractional amount of costs [37]. Tools such as machine-learning approaches based on artificial intelligence (AI) models or the calculation of common matching scores will help to standardize the process of MTB inclusion and MTB treatment recommendations [38].
Liquid biopsies represent a simple, readily available and cost-effective alternative diagnostic tool for the detection and monitoring of targetable genomic alterations over the course of the disease. Overcoming sensitivity issues, this technique harbors the potential to simplify molecular diagnostics in MTB settings [39]. Apart from diagnostics, the use of 3D organoid cell culture approaches (in vitro) or patient-derived xenograft (PDX) models (in vivo) for the evaluation and anticipation of the effectiveness of recommended treatments can be useful, particularly in hematologic malignancies in which most targeted therapeutics remain insufficiently evaluated [40, 41].
Limitations of our current study include its limited sample size and the retrospective design alongside the potential for fragmentary data. Potential bias during the inclusion procedure (selection bias) and during the analysis procedure (detection bias) cannot be ruled out. Moreover, a more comprehensive genomic profiling including RNA transcriptome sequencing and a higher proportion of matched germline DNA would have been desirable for the verification of the biological relevance and conclusiveness of individual genetic alterations. The expansion of diagnostics considering markers that are directly associated with immunotherapeutic rationales such as programmed cell death (ligand)-1 [PD-(L)1] or other treatment targets such as CD19 (CAR T-cell therapy, tafasitamab or loncastuximab tesirine) probably extend the spectrum of treatment options. Another limiting aspect of the current approach is that a large proportion of MTB treatment recommendations was gathered from solid tumors and subsequently extrapolated to the setting of primary refractory aggressive B-cell lymphomas. An example for the limited transferability is the disappointing efficacy of immune checkpoint inhibitors in the light of monotherapy in aggressive B-cell non-Hodgkin lymphomas (apart from primary mediastinal B-cell lymphoma; PMBCL) compared with the revolutionary role among a large spectrum of solid tumors or Hodgkin lymphomas [42,43,44,45]. Novel data suggest the application of pembrolizumab after CAR T-cell failure in relapsed or refractory aggressive B-cell lymphomas [46].
The present study draws attention to the potential benefits of a more frequent inclusion of prDLBCL/HGBL-MYC/BCL2 and prDLBCL/HGBL, NOS serving as a role model in the spectrum of rare and/or difficult-to-treat hematologic malignancies. However, our virtual MTB approach revealed promising therapeutic vulnerabilities associated with reasonable mEL. The present results aim to initiate a learning process expanding the spectrum of individualized treatments into the field of hematology. As our approach is solely virtual in nature, the efficacy and tolerability of molecularly stratified treatments in prDLBCL/HGBL-MYC/BCL2 and prDLBCL/HGBL, NOS and other difficult-to-treat hematologic neoplasms need to be demonstrated in further studies.
References
Alaggio R, Amador C, Anagnostopoulos I, Attygalle AD, Araujo IBO, Berti E, et al. The 5th ediition of the World Health Organization classification of haematolymphoid tumours: lymphoid neoplasms. Leukemia. 2022;36(7):1720–48. https://doi.org/10.1038/s41375-022-01620-2.
Künstner A, Witte HM, Riedl J, Bernard V, Stolting S, Merz H, et al. Mutational landscape of high-grade B-cell lymphoma with MYC-, BCL2 and/or BCL6 rearrangements characterized by whole-exome sequencing. Haematologica. 2021;107(8):1850–63. https://doi.org/10.3324/haematol.2021.279631.
Cucco F, Barrans S, Sha C, Clipson A, Crouch S, Dobson R, et al. Distinct genetic changes reveal evolutionary history and heterogeneous molecular grade of DLBCL with MYC/BCL2 double-hit. Leukemia. 2020;34(5):1329–41. https://doi.org/10.1038/s41375-019-0691-6.
Ennishi D, Jiang A, Boyle M, Collinge B, Grande BM, Ben-Neriah S, et al. Double-Hit gene expression signature defines a distinct subgroup of germinal center B-cell-like diffuse large B-cell lymphoma. J Clin Oncol. 2019;37(3):190–201. https://doi.org/10.1200/JCO.18.01583.
Tempero M. One size fits all? really? J Natl Compr Canc Netw. 2018;16(10):1161. https://doi.org/10.6004/jnccn.2018.0080.
Horak P, Heining C, Kreutzfeldt S, Hutter B, Mock A, Hullein J, et al. Comprehensive genomic and transcriptomic analysis for guiding therapeutic decisions in patients with rare cancers. Cancer Discov. 2021;11(11):2780–95. https://doi.org/10.1158/2159-8290.CD-21-0126.
Heinrich K, Miller-Phillips L, Ziemann F, Hasselmann K, Ruhlmann K, Flach M, et al. Lessons learned: the first consecutive 1000 patients of the CCCMunich (LMU) Molecular Tumor Board. J Cancer Res Clin Oncol. 2023;149(5):1905–15. https://doi.org/10.1007/s00432-022-04165-0.
Tessier-Cloutier B, Grewal JK, Jones MR, Pleasance E, Shen Y, Cai E, et al. The impact of whole genome and transcriptome analysis (WGTA) on predictive biomarker discovery and diagnostic accuracy of advanced malignancies. J Pathol Clin Res. 2022;8(4):395–407. https://doi.org/10.1002/cjp2.265.
Walters MK, Ackerman AT, Weese JL, Ruggeri A, Mullane MP, Hunt A, et al. Quantifying the value of the molecular tumor board: discordance recommendation rate and drug cost avoidance. JCO Precis Oncol. 2022;6: e2200132. https://doi.org/10.1200/PO.22.00132.
Hoefflin R, Geissler AL, Fritsch R, Claus R, Wehrle J, Metzger P, et al. Personalized clinical decision making through implementation of a molecular tumor board: a German single-center experience. JCO Precis Oncol. 2018;2:PO.18.00105. https://doi.org/10.1200/PO.18.00105.
Boehm KM, Khosravi P, Vanguri R, Gao J, Shah SP. Harnessing multimodal data integration to advance precision oncology. Nat Rev Cancer. 2022;22(2):114–26. https://doi.org/10.1038/s41568-021-00408-3.
Witte HM, Fähnrich A, Künstner A, Riedl J, Fliedner SMJ, Reimer N, et al. Primary refractory plasmablastic lymphoma: a precision oncology approach. Front Oncol. 2023;13:1129405. https://doi.org/10.3389/fonc.2023.1129405.
Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375–90. https://doi.org/10.1182/blood-2016-01-643569.
Leichsenring J, Horak P, Kreutzfeldt S, Heining C, Christopoulos P, Volckmar AL, et al. Variant classification in precision oncology. Int J Cancer. 2019;145(11):2996–3010. https://doi.org/10.1002/ijc.32358.
Mateo J, Chakravarty D, Dienstmann R, Jezdic S, Gonzalez-Perez A, Lopez-Bigas N, et al. A framework to rank genomic alterations as targets for cancer precision medicine: the ESMO Scale for Clinical Actionability of molecular Targets (ESCAT). Ann Oncol. 2018;29(9):1895–902. https://doi.org/10.1093/annonc/mdy263.
Wright GW, Huang DW, Phelan JD, Coulibaly ZA, Roulland S, Young RM, et al. A probabilistic classification tool for genetic subtypes of diffuse large B cell lymphoma with therapeutic implications. Cancer Cell. 2020;37(4):551-568 e14. https://doi.org/10.1016/j.ccell.2020.03.015.
Hubschmann D, Jopp-Saile L, Andresen C, Kramer S, Gu Z, Heilig CE, et al. Analysis of mutational signatures with yet another package for signature analysis. Genes Chromosomes Cancer. 2021;60(5):314–31. https://doi.org/10.1002/gcc.22918.
Wilson WH, Wright GW, Huang DW, Hodkinson B, Balasubramanian S, Fan Y, et al. Effect of ibrutinib with R-CHOP chemotherapy in genetic subtypes of DLBCL. Cancer Cell. 2021;39(12):1643-1653 e3. https://doi.org/10.1016/j.ccell.2021.10.006.
Johnson PWM, Balasubramanian S, Hodkinson B, Shreeve SM, Sun S, Srinivasan S, et al. Clinical impact of ibrutinib plus R-CHOP in untreated DLBCL coexpressing BCL2 and MYC in the phase 3 PHOENIX trial. Blood Adv. 2023;7(10):2008–17. https://doi.org/10.1182/bloodadvances.2022009389.
Zhang M, Xu P, Wang L, Cheng S, Zhao W. Genetic subtype guided rituximab-based immunochemotherapy improves outcome in newly diagnosed diffuse large B-cell lymphoma: first report of a randomized phase 2 study. Hematol Oncol. 2021;39(S2). https://doi.org/10.1002/hon.26_2879.
Ramchandren R, Johnson P, Ghosh N, Ruan J, Ardeshna KM, Johnson R, et al. The iR(2) regimen (ibrutinib plus lenalidomide and rituximab) for relapsed/refractory DLBCL: a multicentre, non-randomised, open-label phase 2 study. EClinicalMedicine. 2023;56: 101779. https://doi.org/10.1016/j.eclinm.2022.101779.
Zhang R, Wu HX, Xu M, Xie X. KMT2A/C mutations function as a potential predictive biomarker for immunotherapy in solid tumors. Biomark Res. 2020;8(1):71. https://doi.org/10.1186/s40364-020-00241-0.
Zhang P, Huang Y. Genomic alterations in KMT2 family predict outcome of immune checkpoint therapy in multiple cancers. J Hematol Oncol. 2021;14(1):39. https://doi.org/10.1186/s13045-021-01050-0.
Zhou Y, Jiang W, Zeng L, Mi J, Song L, Lizaso A, et al. A novel ROS1 G2032 K missense mutation mediates lorlatinib resistance in a patient with ROS1-rearranged lung adenocarcinoma but responds to nab-paclitaxel plus pembrolizumab. Lung Cancer. 2020;143:55–9. https://doi.org/10.1016/j.lungcan.2020.03.019.
Zhang X, Wang Y, Qu GAC, Chen J. Pan-cancer analysis of PARP1 alterations as biomarkers in the prediction of immunotherapeutic effects and the association of its expression levels and immunotherapy signatures. Front Immunol. 2021;12: 721030. https://doi.org/10.3389/fimmu.2021.721030.
Rampias T, Karagiannis D, Avgeris M, Polyzos A, Kokkalis A, Kanaki Z, et al. The lysine-specific methyltransferase KMT2C/MLL3 regulates DNA repair components in cancer. EMBO Rep. 2019;20(3):e46821. https://doi.org/10.15252/embr.201846821.
Zoumpoulidou G, Alvarez-Mendoza C, Mancusi C, Ahmed RM, Denman M, Steele CD, et al. Therapeutic vulnerability to PARP1,2 inhibition in RB1-mutant osteosarcoma. Nat Commun. 2021;12(1):7064. https://doi.org/10.1038/s41467-021-27291-8.
Sicklick JK, Kato S, Okamura R, Schwaederle M, Hahn ME, Williams CB, et al. Molecular profiling of cancer patients enables personalized combination therapy: the I-PREDICT study. Nat Med. 2019;25(5):744–50. https://doi.org/10.1038/s41591-019-0407-5.
Gandhi L, Rodriguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018;378(22):2078–92. https://doi.org/10.1056/NEJMoa1801005.
Rini BI, Plimack ER, Stus V, Gafanov R, Hawkins R, Nosov D, et al. Pembrolizumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2019;380(12):1116–27. https://doi.org/10.1056/NEJMoa1816714.
Luchini C, Lawlor RT, Milella M, Scarpa A. Molecular tumor boards in clinical practice. Trends Cancer. 2020;6(9):738–44. https://doi.org/10.1016/j.trecan.2020.05.008.
Janysek DC, Kim J, Duijf PHG, Dray E. Clinical use and mechanisms of resistance for PARP inhibitors in homologous recombination-deficient cancers. Transl Oncol. 2021;14(3): 101012. https://doi.org/10.1016/j.tranon.2021.101012.
Ajorloo F, Vaezi M, Saadat A, Safaee SR, Gharib B, Ghanei M, et al. A systems medicine approach for finding target proteins affecting treatment outcomes in patients with non-Hodgkin lymphoma. PLoS ONE. 2017;12(9): e0183969. https://doi.org/10.1371/journal.pone.0183969.
Duhrsen U, Muller S, Hertenstein B, Thomssen H, Kotzerke J, Mesters R, et al. Positron emission tomography-guided therapy of aggressive non-hodgkin lymphomas (PETAL): a multicenter randomized phase III trial. J Clin Oncol. 2018;36(20):2024–34. https://doi.org/10.1200/JCO.2017.76.8093.
Locke FL, Miklos DB, Jacobson CA, Perales MA, Kersten MJ, Oluwole OO, et al. Axicabtagene ciloleucel as second-line therapy for large B-cell lymphoma. N Engl J Med. 2022;386(7):640–54. https://doi.org/10.1056/NEJMoa2116133.
Kamdar M, Solomon SR, Arnason J, Johnston PB, Glass B, Bachanova V, et al. Lisocabtagene maraleucel versus standard of care with salvage chemotherapy followed by autologous stem cell transplantation as second-line treatment in patients with relapsed or refractory large B-cell lymphoma (TRANSFORM): results from an interim analysis of an open-label, randomised, phase 3 trial. Lancet. 2022;399(10343):2294–308. https://doi.org/10.1016/S0140-6736(22)00662-6.
Pages A, Foulon S, Zou Z, Lacroix L, Lemare F, de Baere T, et al. The cost of molecular-guided therapy in oncology: a prospective cost study alongside the MOSCATO trial. Genet Med. 2017;19(6):683–90. https://doi.org/10.1038/gim.2016.174.
Petak I, Kamal M, Dirner A, Bieche I, Doczi R, Mariani O, et al. A computational method for prioritizing targeted therapies in precision oncology: performance analysis in the SHIVA01 trial. NPJ Precis Oncol. 2021;5(1):59. https://doi.org/10.1038/s41698-021-00191-2.
Russo A, Incorvaia L, Del Re M, Malapelle U, Capoluongo E, Gristina V, et al. The molecular profiling of solid tumors by liquid biopsy: a position paper of the AIOM-SIAPEC-IAP-SIBioC-SIC-SIF Italian Scientific Societies. ESMO Open. 2021;6(3): 100164. https://doi.org/10.1016/j.esmoop.2021.100164.
Artegiani B, Clevers H. Use and application of 3D-organoid technology. Hum Mol Genet. 2018;27(R2):R99–107. https://doi.org/10.1093/hmg/ddy187.
Liu Y, Wu W, Cai C, Zhang H, Shen H, Han Y. Patient-derived xenograft models in cancer therapy: technologies and applications. Signal Transduct Target Ther. 2023;8(1):160. https://doi.org/10.1038/s41392-023-01419-2.
Reck M, Rodriguez-Abreu D, Robinson AG, Hui R, Csoszi T, Fulop A, et al. Updated analysis of KEYNOTE-024: pembrolizumab versus platinum-based chemotherapy for advanced non-small-cell lung cancer with PD-L1 tumor proportion score of 50% or greater. J Clin Oncol. 2019;37(7):537–46. https://doi.org/10.1200/JCO.18.00149.
Kuruvilla J, Ramchandren R, Santoro A, Paszkiewicz-Kozik E, Gasiorowski R, Johnson NA, et al. Pembrolizumab versus brentuximab vedotin in relapsed or refractory classical Hodgkin lymphoma (KEYNOTE-204): an interim analysis of a multicentre, randomised, open-label, phase 3 study. Lancet Oncol. 2021;22(4):512–24. https://doi.org/10.1016/S1470-2045(21)00005-X.
Ansell SM, Minnema MC, Johnson P, Timmerman JM, Armand P, Shipp MA, et al. Nivolumab for relapsed/refractory diffuse large B-cell lymphoma in patients ineligible for or having failed autologous transplantation: a single-arm, phase II study. J Clin Oncol. 2019;37(6):481–9. https://doi.org/10.1200/JCO.18.00766.
Zinzani PLL, Thieblemont C, Melnichenko V, Bouabdallah K, Walewski J, Majlis A, et al. Pembrolizumab in relapsed or refractory primary mediastinal large B-cell lymphoma: final analysis of KEYNOTE-170. Blood. 2023;142(2):141–5. https://doi.org/10.1182/blood.2022019340.
Chong EA, Alanio C, Svoboda J, Nasta SD, Landsburg DJ, Lacey SF, et al. Pembrolizumab for B-cell lymphomas relapsing after or refractory to CD19-directed CAR T-cell therapy. Blood. 2022;139(7):1026–38. https://doi.org/10.1182/blood.2021012634.
Meric-Bernstam F, Bahleda R, Hierro C, Sanson M, Bridgewater J, Arkenau HT, et al. Futibatinib, an irreversible FGFR1-4 inhibitor patients with advanced solid tumors harboring FGF/FGFR aberrations: a phase I dose-expansion study. Cancer Discov. 2022;12(2):402–15. https://doi.org/10.1158/2159-8290.CD-21-0697.
Wainberg ZA, Enzinger PC, Kang YK, Qin S, Yamaguchi K, Kim IH, et al. Bemarituzumab in patients with FGFR2b-selected gastric or gastro-oesophageal junction adenocarcinoma (FIGHT): a randomised, double-blind, placebo-controlled, phase 2 study. Lancet Oncol. 2022;23(11):1430–40. https://doi.org/10.1016/S1470-2045(22)00603-9.
Ferrarotto R, Eckhardt G, Patnaik A, LoRusso P, Faoro L, Heymach JV, et al. A phase I dose-escalation and dose-expansion study of brontictuzumab in subjects with selected solid tumors. Ann Oncol. 2018;29(7):1561–8. https://doi.org/10.1093/annonc/mdy171.
Ahn ER, Mangat PK, Garrett-Mayer E, Halabi S, Dib EG, Haggstrom DE, et al. Palbociclib in patients with non-small-cell lung cancer with CDKN2A alterations: results from the targeted agent and profiling utilization registry study. JCO Precis Oncol. 2020;4:757–66. https://doi.org/10.1200/PO.20.00037.
Kawazoe A, Kuboki Y, Bando H, Fukuoka S, Kojima T, Naito Y, et al. Phase 1 study of napabucasin, a cancer stemness inhibitor, in patients with advanced solid tumors. Cancer Chemother Pharmacol. 2020;85(5):855–62. https://doi.org/10.1007/s00280-020-04059-3.
Izutsu K, Ando K, Nishikori M, Shibayama H, Teshima T, Kuroda J, et al. Phase II study of tazemetostat for relapsed or refractory B-cell non-Hodgkin lymphoma with EZH2 mutation in Japan. Cancer Sci. 2021;112(9):3627–35. https://doi.org/10.1111/cas.15040.
Park H, Shapiro GI, Gao X, Mahipal A, Starr J, Furqan M, et al. Phase Ib study of eprenetapopt (APR-246) in combination with pembrolizumab in patients with advanced or metastatic solid tumors. ESMO Open. 2022;7(5): 100573. https://doi.org/10.1016/j.esmoop.2022.100573.
Xie T, Feng Q, Li Z, Lu M, Li J, Lizaso A, et al. Heterogeneous constitutional mismatch repair deficiency with MSH6 missense mutation clinically benefits from pembrolizumab and regorafenib combination therapy: a case report and literature review. Hered Cancer Clin Pract. 2021;19(1):7. https://doi.org/10.1186/s13053-021-00165-2.
Golan T, Varadhachary GR, Sela T, Fogelman DR, Halperin N, Shroff RT, et al. Phase II study of olaparib for BRCAness phenotype in pancreatic cancer. J Clin Oncol. 2018;36(4_suppl):297. https://doi.org/10.1200/JCO.2018.36.4_suppl.297.
Scholze H, Stephenson RE, Reynolds R, Shah S, Puri R, Butler SD, et al. Combined EZH2 and Bcl-2 inhibitors as precision therapy for genetically defined DLBCL subtypes. Blood Adv. 2020;4(20):5226–31. https://doi.org/10.1182/bloodadvances.2020002580.
Qualls D, Noy A, Straus D, Matasar M, Moskowitz C, Seshan V, et al. Molecularly targeted epigenetic therapy with mocetinostat in relapsed and refractory non-Hodgkin lymphoma with CREBBP or EP300 mutations: an open label phase II study. Leuk Lymphoma. 2023;64(3):738–41. https://doi.org/10.1080/10428194.2022.2164194.
Kim E, Jiang Y, Xu T, Bazeos A, Knapp A, Bolen CR, et al. Prognostic mutational subtyping in de novo diffuse large B-cell lymphoma. BMC Cancer. 2022;22(1):231. https://doi.org/10.1186/s12885-022-09237-5.
Blay JY, Serrano C, Heinrich MC, Zalcberg J, Bauer S, Gelderblom H, et al. Ripretinib in patients with advanced gastrointestinal stromal tumours (INVICTUS): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2020;21(7):923–34. https://doi.org/10.1016/S1470-2045(20)30168-6.
Montesinos P, Recher C, Vives S, Zarzycka E, Wang J, Bertani G, et al. Ivosidenib and azacitidine in IDH1-mutated acute myeloid leukemia. N Engl J Med. 2022;386(16):1519–31. https://doi.org/10.1056/NEJMoa2117344.
Jackman DM, Jegede O, Zauderer MG, Mitchell EP, Zwiebel J, Gray RJ, et al. A phase 2 study of defactinib (VS-6063) in patients with NF2 altered tumors: Results from NCI-match (EAY131) subprotocol U. J Clin Oncol. 2021;39(15_suppl):3087–3087. https://doi.org/10.1200/JCO.2021.39.15_suppl.3087.
Itzykson R, Kosmider O, Cluzeau T, Mansat-De Mas V, Dreyfus F, Beyne-Rauzy O, et al. Impact of TET2 mutations on response rate to azacitidine in myelodysplastic syndromes and low blast count acute myeloid leukemias. Leukemia. 2011;25(7):1147–52. https://doi.org/10.1038/leu.2011.71.
Janning M, Suptitz J, Albers-Leischner C, Delpy P, Tufman A, Velthaus-Rusik JL, et al. Treatment outcome of atypical EGFR mutations in the German National Network Genomic Medicine Lung Cancer (nNGM). Ann Oncol. 2022;33(6):602–15. https://doi.org/10.1016/j.annonc.2022.02.225.
Cavalieri S, Perrone F, Miceli R, Ascierto PA, Locati LD, Bergamini C, et al. Efficacy and safety of single-agent pan-human epidermal growth factor receptor (HER) inhibitor dacomitinib in locally advanced unresectable or metastatic skin squamous cell cancer. Eur J Cancer. 2018;97:7–15. https://doi.org/10.1016/j.ejca.2018.04.004.
Ang C, Stollman A, Zhu H, Sarpel U, Scarborough B, Sahni G, et al. Clinical benefit from trametinib in a patient with appendiceal adenocarcinoma with a GNAS R201H mutation. Case Rep Oncol. 2017;10(2):548–52. https://doi.org/10.1159/000477562.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by Projekt DEAL.
Conflict of interest
NR, AK, and HB acknowledge computational support from the OMICS compute cluster at the University of Lübeck. HB acknowledges funding by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) under Germany’s Excellence Strategy – EXC 22167-390884018. AK and NK acknowledge computational support from the OMICS compute cluster at the University of Lübeck. HW, NG, JR, AF, JK, VB, HM, AF, SF and NvB declare that they have no conflicts of interest that might be relevant to the contents of this manuscript.
Ethics approval
This retrospective study was approved by the ethics committee of the University of Lübeck (reference no. 18-356), conducted in accordance with the Declaration of Helsinki.
Consent to participate
Patients have provided written informed consent regarding routine diagnostic and academic investigations, including genomic studies of their biopsy specimen as well as the transfer of their clinical data.
Consent for publication
Not applicable.
Data availability
The datasets generated during and/or analyzed during the current study are available from the European genome-phenome archive (EGA), accession number EGAS00001005420.
Code availability
The analysis was performed using R and Prism9 (GraphPad). The code is available upon request.
Author contributions
Study concept: HW, NG. Data collection: HW, JR, AF, AK, JK, NR, VB, HM, AF, NG. Data analysis and creation of figures and tables: HW, AF, AK, SF, NvB, HM, HB, AF, NG. Initial draft of manuscript: HW. Critical revision and approval of final version: all authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Witte, H.M., Riedl, J., Künstner, A. et al. Molecularly Stratified Treatment Options in Primary Refractory DLBCL/HGBL with MYC and BCL2 or BCL6 Rearrangements (HGBL, NOS with MYC/BCL6). Targ Oncol 18, 749–765 (2023). https://doi.org/10.1007/s11523-023-00983-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-023-00983-5