Abstract
Background
In RELAY, a randomized, double-blind, phase III trial investigating the efficacy and safety of ramucirumab+erlotinib (RAM+ERL) or ERL+placebo (PBO) in patients with untreated, stage IV, epidermal growth factor receptor (EGFR)-mutated non-small cell lung cancer (NSCLC), RAM+ERL demonstrated superior progression-free survival (PFS) versus PBO+ERL, with no new safety signals.
Objective
The aim of this paper was to report efficacy and tolerability findings for the Taiwanese participants of RELAY.
Patients and Methods
Patients were randomized 1:1 to RAM+ERL or ERL+PBO. Primary endpoint was investigator-assessed PFS. Secondary endpoints included objective response rate (ORR), duration of response (DoR) and tolerability. Data for the current analysis are reported descriptively.
Results
In RELAY, 56 Taiwanese patients were enrolled; 26 received RAM+ERL, 30 received ERL+PBO. The demographic profile of the Taiwanese subgroup was consistent with that of the overall RELAY population. Median PFS for RAM+ERL/ERL+PBO, respectively, was 22.05 months/13.40 months (unstratified hazard ratio 0.4; 95% confidence interval 0.2–0.9); ORR was 92%/60%; median DoR was 18.2 months/12.7 months. All patients experienced one or more treatment-emergent adverse events (TEAEs); those most commonly reported were diarrhea and dermatitis acneiform (58% each) for RAM+ERL and diarrhea (70%) and paronychia (63%) for PBO+ERL. Grade ≥ 3 TEAEs were experienced by 62%/30% of RAM+ERL/PBO+ERL patients, respectively, and included dermatitis acneiform (19%/7%), hypertension (12%/7%), and pneumonia (12%/0%).
Conclusions
PFS for the Taiwanese participants of RELAY receiving RAM+ERL versus ERL+PBO was consistent with that in the overall RELAY population. These results, together with no new safety signals and a manageable safety profile, may support first-line use of RAM+ERL in Taiwanese patients with untreated EGFR-mutant stage IV NSCLC.
Trial Registration
www.clinicaltrials.gov, NCT02411448.
Similar content being viewed by others
A potential treatment strategy for patients with epidermal growth factor receptor (EGFR)-mutated non-small cell lung cancer (NSCLC) is dual inhibition of the EGFR and vascular endothelial growth factor (VEGF) signaling pathways. |
In the global, randomized, phase III RELAY study, the combination of ramucirumab, a human immunoglobulin G1 monoclonal antibody against VEGF receptor 2, and erlotinib, an EGFR tyrosine kinase inhibitor, demonstrated superior progression-free survival (PFS) versus erlotinib plus placebo in patients with untreated, EGFR-mutated, stage IV NSCLC. |
In this exploratory analysis of study data, PFS for the Taiwanese participants of RELAY receiving ramucirumab plus erlotinib versus erlotinib plus placebo was consistent with that in the overall RELAY population, with no new safety signals. |
1 Introduction
In 2020, lung cancer was the second most common cancer worldwide, with approximately 2.21 million new cases, and was associated with the highest number of cancer deaths at 1.80 million [1]. In Taiwan, lung cancer has the highest mortality rate of all cancers and accounts for nearly 19% of all cancer deaths [2]. Non-small cell lung cancer (NSCLC) is the most prevalent type of lung cancer globally, accounting for 85% of all lung cancer cases [3].
Epidermal growth factor receptor (EGFR) gene mutations are commonly associated with NSCLC in certain populations [4] and occur more commonly in East Asian populations (30–60%) than in Caucasian populations (7–20%) [4,5,6]. EGFR mutations have been reported in 34.0–55.7% of Taiwanese patients with lung cancer [5, 7]. Of note, EGFR mutations are also more commonly found in women and non-smokers [5, 8].
The presence of specific activating EGFR mutations—exon 19 deletion or exon 21 (L858R) substitution—is indicative of sensitivity to EGFR tyrosine kinase inhibitors (TKIs), the current first-line standard of care in EGFR-mutated NSCLC [9], and should be considered when deciding on the treatment strategy [6, 10]. Unfortunately, most patients with EGFR mutant lung cancers receiving EGFR TKIs will eventually experience disease progression due to acquired resistance, which limits the long-term efficacy of these agents [11,12,13]. This highlights the need for additional first-line treatment options that extend EGFR TKI efficacy and delay disease progression and the emergence of TKI resistance.
A potential treatment strategy is dual inhibition of the EGFR and vascular endothelial growth factor (VEGF) signaling pathways [14]. EGFR and VEGF have interconnected signaling pathways [15]; VEGF is a key regulator of angiogenesis, and dysregulation of the EGFR pathway results in upregulation of the VEGF pathway [15]. Dual inhibition of these pathways has been shown to reduce angiogenesis and attenuate tumor resistance to EGFR TKIs [14, 16]. Targeting these pathways to improve outcomes in patients with EGFR-mutated NSCLC is supported by preclinical and clinical data [15, 17,18,19].
Ramucirumab (RAM) is a human immunoglobulin G1 monoclonal antibody against VEGF receptor 2 (VEGFR-2) that demonstrated efficacy in patients with untreated, EGFR-mutated, stage IV NSCLC in the RELAY study [20]. This global, randomized, phase III study compared the efficacy and safety of RAM combined with the EGFR TKI erlotinib (ERL) versus ERL plus placebo (PBO). East Asian patients comprised 75% (336/449) of the overall population and included 56 patients from Taiwan (12% of the overall population). In the intention-to-treat (ITT) population, the primary endpoint, progression-free survival (PFS), was significantly longer in the RAM+ERL group compared with the ERL+PBO group (median PFS: 19.4 vs 12.4 months; stratified hazard ratio [HR] 0.59; 95% confidence interval [CI] 0.46–0.76; p < 0.0001). In addition, there were no new safety signals and safety outcomes were consistent with similar studies investigating RAM and ERL [20].
Currently, RAM+ERL is an approved first-line regimen for patients with EGFR-mutated NSCLC in Taiwan. However, there is a lack of published evidence on the efficacy and safety of RAM in Taiwanese patients with NSCLC. This manuscript presents the efficacy and safety findings from an exploratory analysis of the subgroup of patients from Taiwan included in the RELAY study and examines them in the context of the overall study results.
2 Methods
2.1 Study Design, Population and Treatment
The RELAY study was a global, double-blind, placebo-controlled, phase III trial (www.clinicaltrials.gov identifier: NCT02411448) conducted across 13 countries (Canada, France, Germany, Hong Kong, Italy, Japan, Romania, South Korea, Spain, Taiwan, Turkey, the UK and the USA). Patients were enrolled between 28 January 2016 and 1 February 2018 across 100 investigator sites. Key inclusion criteria for patient enrolment included age at least 18 years (at least 20 years in Taiwan), stage IV NSCLC, EGFR mutation-positive (exon 19 deletion or exon 21 [L858R] substitution), and Eastern Cooperative Oncology Group (ECOG) performance status (PS) 0–1. Key exclusion criteria included known EGFR T790M mutation, prior treatment with EGFR TKI treatment or chemotherapy and central nervous system metastases. Patients who met the inclusion criteria were randomized 1:1 to receive either RAM+ERL or PBO+ERL and treated until progression or unacceptable toxicity was evident. The full RELAY study details have been published [20]. The study was conducted in accordance with the ethical principles of the Declaration of Helsinki. Informed consent was obtained from all patients prior to participating in the study. The protocol and amendments were approved by the ethics committees of all participating centers.
2.2 Endpoints
The primary endpoint was investigator-assessed PFS measured as time from randomization to disease progression or death from any cause, assessed by investigators using the Response Evaluation Criteria in Solid Tumors version 1.1 (RECIST v1.1). Secondary endpoints included overall survival (OS), objective response rate (ORR), disease control rate (DCR), and duration of response (DoR). Safety and tolerability assessments included treatment-emergent adverse events (TEAEs), treatment-emergent serious adverse events (TE-SAEs), treatment-emergent adverse events (AEs) of special interest (TE-AESIs), and deaths, including those due to AEs. Exploratory endpoints included PFS2 (time from randomization to second objective disease progression after start of additional systemic anticancer treatment or death from any other cause, whichever occurred first).
2.3 Statistical Analysis
The data cut-off date was 23 January 2019. Statistical analysis was descriptive only as RELAY was not powered to show statistical significance between treatment arms for the subgroup of patients in the Taiwanese population. Efficacy endpoints were assessed in the ITT population, which included all randomly assigned patients. Analyses were performed using Kaplan–Meier methodology to estimate medians with 95% CI based on normal approximation. Comparisons were made using the unstratified log-rank test. Safety and exposure analyses were performed on the safety population. The safety population included all randomized patients who received at least one dose of an investigational product (i.e., RAM or PBO) administered in combination with ERL. The extent of exposure was also analyzed by assessment of drug exposure and dose intensity. SAS Enterprise Guide, version 7.15 was used for all statistical analyses.
3 Results
3.1 Baseline and Other Characteristics
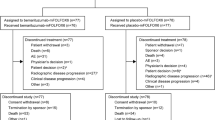
The Taiwanese subgroup population consisted of 56 patients (12% of the total RELAY study population) randomized to receive RAM+ERL (26 patients) or PBO+ERL (30 patients), enrolled from eight local sites. The majority of patients were female (63%) and had never smoked (73%). All (100%) patients enrolled in the subgroup received study treatment. Baseline characteristics were balanced across treatment arms (Table 1). At data cut-off, eight patients were on treatment (RAM+ERL: 6 patients [23%]; PBO+ERL: 2 patients [7%]). Disease progression was the most common reason for discontinuing treatment and was higher among the PBO+ERL group (PBO+ERL: 26 patients [87%]; RAM+ERL: 12 patients [46%]). Post-treatment discontinuation follow-up ended due to loss to follow-up in 1/26 patients (3.8%) in the RAM+ERL arm and 2/30 patients (6.7%) in the PBO+ERL arm.
3.2 Efficacy Data
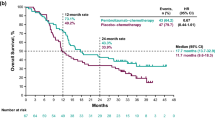
After a median duration of follow-up of 20.7 months (interquartile range [IQR] 15.8–27.2), investigator-assessed PFS was longer in patients receiving RAM+ERL than in those receiving PBO+ERL (median 22.05 months vs 13.40 months, unstratified HR: 0.4; 95% CI: 0.2–0.9) (Fig. 1A). Likewise, the ORR was numerically higher with RAM+ERL than with PBO+ERL (92% vs 60%, respectively). DCR was similar with RAM+ERL and PBO+ERL (100% vs 93%, respectively) (Table 2). The median DoR in patients who responded to treatment was longer in the RAM+ERL treatment arm (18.2 months) than in the PBO+ERL treatment arm (12.7 months) (Table 2). OS data were immature at cut-off with a censoring of 92% for RAM+ERL and 93% for PBO+ERL (OS HR 1.16; 95% CI: 0.16–8.25). Similarly, PFS2 data were immature, with a censoring rate of 92% for RAM+ERL and 93% for PBO+ERL (HR 1.16; 95% CI: 0.16–8.25) (Table 2).
Kaplan–Meier plot of PFS (investigator-assessed) for A Taiwanese subgroupa (n = 56) and B overall RELAY ITT population (n = 449)b. aMedian follow-up was 20.7 months (IQR 15·8–27.2). bFigure B reproduced [20] with permission from Elsevier. CI confidence interval, ERL erlotinib, HR hazard ratio, ITT intention to treat, PBO placebo, PFS progression-free survival, RAM ramucirumab
3.3 Treatment Exposure
The median duration of RAM or PBO therapy was numerically shorter in patients who received RAM+ERL than in those who received PBO+ERL (9.0 vs 11.2 months, respectively) (Table 3). In contrast, the restricted mean duration of therapy for RAM or PBO was numerically longer in patients who received RAM+ERL than those who received PBO+ERL (12.8 vs 11.7 months, respectively) (Table 3). The median duration of ERL was numerically longer in those receiving RAM than in those receiving PBO (13.7 months vs 12.4 months, respectively) (Table 3). Relative dose intensity was >90% across treatment arms (Table 3). In patients receiving RAM or PBO, a lower percentage of patients receiving PBO required dose modifications than patients receiving RAM (53% vs 81%, respectively).
3.4 Safety
All patients reported at least one TEAE, irrespective of the study treatment they received (Table 4). The most commonly reported any-grade TEAEs were diarrhea and dermatitis acneiform (58% each) for RAM+ERL, and diarrhea (70%) and paronychia (63%) for PBO+ERL (Table 5). Dermatitis acneiform was the most common grade ≥ 3 TEAE in either arm (RAM+ERL 19%; PBO+ERL 7%) and the only grade ≥ 3 TEAE in PBO+ERL patients (7%) (Table 5). Pneumonia and skin infection were the most common grade ≥ 3 SAEs, occurring in 12% and 8% of RAM+ERL-treated patients, respectively (no patient in the PBO+ERL arm experienced pneumonia or skin infection). One patient receiving PBO+ERL experienced grade ≥ 3 pneumothorax (vs none receiving RAM+ERL) (Table 5). Incidence of any-grade TE-AESIs was 73% for RAM+ERL patients (vs 20% for PBO patients), with bleeding/hemorrhage and liver injury/failure each seen in 50% of patients. Half of the patients receiving PBO+ERL experienced any-grade liver injury/failure (Table 5). Only one patient (receiving PBO+ERL) experienced grade ≥ 3 pneumonitis; no other interstitial lung disease (ILD) events were recorded (Table 5). Only one patient treated with RAM+ERL discontinued due to an AE and the event was non-serious. No patient receiving ERL+PBO discontinued due to an AE (Table 4). The main AEs of any grade leading to dose modifications were increased blood bilirubin (RAM+ERL 27% vs PBO+ERL 17%), proteinuria (RAM+ERL 23% vs PBO+ERL 0%), increased alanine aminotransferase (RAM+ERL 8% vs PBO+ERL 7%), and epistaxis (RAM+ERL 8% vs PBO+ERL 0%). No deaths due to an AE or within 30 days of discontinuation from study treatment were recorded in the Taiwanese subgroup.
4 Discussion
In this exploratory subgroup analysis of the Taiwanese patient population within the RELAY study, RAM+ERL demonstrated numerically longer PFS versus PBO+ERL in patients with untreated metastatic NSCLC and sensitizing EGFR mutations. This finding is consistent with that of the overall RELAY study (Fig. 1B, in which PFS was significantly longer with RAM+ERL vs PBO+ERL (p < 0.0001) [20]. The median duration of follow-up for the Taiwanese subgroup was consistent with that for the overall RELAY population (~ 21 months) and, hence, was considered sufficient for the detection of PFS events. Tolerability likewise was consistent between the RAM+ERL treatment arms in the Taiwanese subgroup and the overall RELAY safety population, with no unexpected safety concerns in the Taiwanese subgroup. Considering secondary outcomes, DoR was higher with RAM+ERL than with PBO+ERL in both the Taiwanese subgroup and the overall RELAY population, and DCR was consistent across treatment arms in both populations.
The finding that ORR was higher with RAM+ERL than with PBO+ERL in the Taiwanese subgroup but similar across both groups in the overall RELAY population should be interpreted with caution due to the small sample size of the Taiwanese subgroup. Overall survival and PFS2 results for the Taiwanese subgroup and the overall RELAY population were premature at cut-off, precluding comparison of the two groups. Patients enrolled in RELAY were representative of a real-world NSCLC population with a higher percentage of women and non-smokers [22]—a profile reflected in the Taiwanese subgroup.
In patients receiving RAM or PBO in the Taiwanese subgroup, the median duration of therapy was numerically shorter in the RAM+ERL treatment arm than in the PBO+ERL treatment arm, whereas the duration of therapy for ERL was longer in the RAM+ERL arm than in the PBO+ERL arm. In contrast, patients in the overall RELAY population had longer duration of therapy for both drugs in the RAM+ERL arm compared with the PBO+ERL arm. The numerically shorter duration of therapy for RAM or PBO in patients receiving RAM+ERL versus PBO+ERL in the Taiwanese subgroup is probably a consequence of small sample sizes on the point estimation of the median using Kaplan–Meier methodology. This was further explored using restricted mean survival time (RMST), an alternative measure that may overcome some of the limitations of proportional hazards modeling. RMST is the average time free from an event up until a milestone time point—a numeric expression of the area under the Kaplan–Meier survival curve [23]. In restricted mean analyses, duration of therapy for RAM or PBO in patients receiving RAM+ERL versus PBO+ERL in the Taiwanese subgroup was in line with findings in the overall RELAY population.
Median duration of treatment was calculated in the RELAY study using the last known treatment stop date at data cut-off, and so did not take into account patients who were still on treatment or those without progression who had discontinued study treatment for other reasons. Hence, median duration of therapy is an underestimate of the true, expected therapy duration. In the overall RELAY population, at the time of data cut-off, 107/449 patients were still on study treatment, 64/224 patients randomized to RAM+ERL and 43/225 randomized to PBO+ERL [20]. For the Taiwanese subgroup, 8/56 patients were on treatment at data cut-off, 6/26 receiving RAM+ERL and 2/30 PBO+ERL. The limited number of patients included in the Taiwanese subgroup could have increased the magnitude of variability in this finding.
Treatment resistance with first- and second-generation EGFR TKIs is primarily mediated through the emergence of gatekeeper T790M resistance mutations and remains a therapeutic challenge in patients with mutated NSCLC [11,12,13]. The third-generation EGFR TKI, osimertinib, inhibits T790M resistance mutations [24, 25] and thus may be an effective strategy after first- (or second-) generation EGFR TKI treatment failure. Consequently, osimertinib is the preferred first-line treatment option for patients with EGFR-mutant stage IV NSCLC recommended by the European Society for Medical Oncology (ESMO), the American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) [26,27,28]. However, the ESMO guidelines note that the osimertinib PFS and OS benefits were less pronounced in Asian patients. These results were evident from the subgroup analysis of the FLAURA study. Patients receiving osimertinib in the non-Asian subgroup achieved longer OS than those in the Asian subgroup (HR 0.54; 95% CI 0.38–0.77 vs HR 1.00; 95% CI 0.75–1.32) [29]. Furthermore, like first- and second-generation EGFR TKIs, osimertinib-treated patients may also develop treatment resistance. The mechanisms of treatment resistance in osimertinib are heterogenous and yet to be fully elucidated, highlighting the need for further treatment options.
An additional approach to improve outcomes could be the addition of antiangiogenic treatment (e.g., the anti-VEGFR2 antibody ramucirumab) to an EGFR TKI. Preclinical trials have highlighted the role of VEGF/VEGFR expression in EGFR TKI resistance and further reported on the efficacy of combining VEGFR inhibitors and EGFR TKIs [15, 17]. Combination treatment with ERL and an antiangiogenic treatment is an alternative first-line therapy recommended by the ESMO, ASCO and NCCN when osimertinib is unavailable [26,27,28]. Ramucirumab and bevacizumab are both antiangiogenic treatments which have been investigated in separate clinical trials. The RELAY study has demonstrated the superiority of dual inhibition of VEGF and EGFR signaling pathways over EGFR TKI+PBO in global and, specifically, Asian populations [20, 30, 31]. The ARTEMIS trial, a phase III, randomized, double-blinded study that compared a VEGF inhibitor (bevacizumab) with or without ERL in Chinese patients with untreated EGFR-mutant NSCLC, also reported a PFS benefit for bevacizumab+ERL over ERL alone [32]. The combination of bevacizumab+ERL over ERL alone was also investigated in the phase II JO25567 study; Japanese patients with stage IIIB–IV EGFR-mutant NSCLC, receiving combination therapy of bevacizumab + ERL, achieved significant improvement in PFS than patients receiving ERL alone although this did not translate into a significant improvement in OS between the treatment groups [33]. These results were validated by the NEJ026 phase III trial that confirmed significantly longer PFS in patients receiving combination therapy of bevacizumab+ERL than patients receiving ERL alone [19].
The AE profile was consistent in type and severity between the RAM+ERL treatment arms in the Taiwanese subgroup and the overall RELAY safety population. The most commonly observed TEAEs in patients receiving RAM+ERL or PBO+ERL in either study group, diarrhea and dermatitis acneiform, are known AEs associated with ERL therapy [34, 35]. Since EGFR is expressed in numerous cell tissues including the skin and gastrointestinal tract (GIT), the inhibition of EGFR TK activity has direct effects on these organ systems although exact mechanisms are poorly understood. In the skin, EGFR inhibition ultimately results in inflammation-induced dermatitis acneiform [35]. In the GIT, multiple factors are considered to be the cause of diarrhea; one theory is excess chloride which leads to secretory diarrhea [36]. Diarrhea and dermatitis acneiform of any grade was numerically higher in both treatments arms of the Japanese and overall RELAY safety population than in the Taiwanese subgroup; however, this could be explained by the small sample size [20, 31].
Hypertension is a known AE of VEGF inhibitor therapy [36], and was the most common grade ≥ 3 TE-AESI among both the Taiwanese subgroup and the overall RELAY safety population. ILD is one of the most serious AEs associated with TKIs. Despite the use of steroids to treat ILD, patients receiving TKIs for NSCLC often discontinue TKI therapy [37]. Globally, the incidence of TKI-induced ILD in patients with NSCLC is approximately 1%; a higher incidence (3.5%) has been reported in Japanese populations [37, 38]. Only one ILD/pneumonitis event was reported (in a patient receiving PBO+ERL) in the Taiwanese subgroup, and this is consistent with the few such events reported in the overall RELAY population [20].
5 Limitations/Strengths
The small size of the Taiwanese subgroup and retrospective nature of the study are major limitations of this analysis, preventing powered statistical analysis. Interpretation of the findings and their extrapolation to a broader Taiwanese population should therefore be made in this context. Of note, however, is that the descriptive results observed in the Taiwanese subgroup were generally consistent with those reported in the overall RELAY population.
6 Conclusion
PFS for the Taiwanese subgroup of patients with untreated EGFR mutation-positive stage IV NSCLC receiving first-line treatment with RAM+ERL versus ERL+PBO in the RELAY study appeared to be consistent with that in the overall RELAY population. These results, together with no new safety signals and a manageable safety profile, may support the first-line use of RAM+ERL in untreated EGFR-mutant stage IV NSCLC in a Taiwanese population.
References
World Health Organization. Cancer. 2022. https://www.who.int/news-room/fact-sheets/detail/cancer. Accessed 11 May 2022.
Taiwan Ministry of Health and Welfare. Cause of death statistics. 2019. https://www.mohw.gov.tw/cp-4650-50697-2.html. Accessed 11 May 2022.
Oser MG, Niederst MJ, Sequist LV, Engelman JA. Transformation from non-small-cell lung cancer to small-cell lung cancer: molecular drivers and cells of origin. Lancet Oncol. 2015;16(4):e165–72. https://doi.org/10.1016/S1470-2045(14)71180-5.
Prabhakar CN. Epidermal growth factor receptor in non-small cell lung cancer. Transl Lung Canc Res. 2015;4(2):110. https://doi.org/10.3978/j.issn.2218-6751.2015.01.01.
Shigematsu H, Lin L, Takahashi T, Nomura M, Suzuki M, Wistuba II, et al. Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J Natl Cancer Inst. 2005;97(5):339–46. https://doi.org/10.1093/jnci/dji055.
Hsu WH, Yang JH, Mok TS, Loong HH. Overview of current systemic management of EGFR-mutant NSCLC. Ann Oncol. 2018;29(Suppl. 1):i3-9. https://doi.org/10.1093/annonc/mdx702.
Hsu KH, Ho CC, Hsia TC, Tseng JS, Su KY, Wu MF, et al. Identification of five driver gene mutations in patients with treatment-naive lung adenocarcinoma in Taiwan. PLoS One. 2015;10(3):e0120852. https://doi.org/10.1371/journal.pone.0120852.
Gazdar A. Activating and resistance mutations of EGFR in non-small-cell lung cancer: role in clinical response to EGFR tyrosine kinase inhibitors. Oncogene. 2009;28(Suppl. 1):S24-31. https://doi.org/10.1038/onc.2009.198.
Planchard D, Popat ST, Kerr K, Novello S, Smit EF, Faivre-Finn C, et al. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29(Supp. 4):iv192-237. https://doi.org/10.1093/annonc/mdy275.
Sheng M, Wang F, Zhao Y, Li S, Wang X, Shou T, et al. Comparison of clinical outcomes of patients with non-small-cell lung cancer harbouring epidermal growth factor receptor exon 19 or exon 21 mutations after tyrosine kinase inhibitors treatment: a meta-analysis. Eur J Clin Pharmacol. 2016;72(1):1–11. https://doi.org/10.1007/s00228-015-1966-0.
Yu AH, Arcila ME, Rekhtman N, Sima CS, Zakowski MF, Pao W, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Canc Res. 2013;19(8):2240–7. https://doi.org/10.1158/1078-0432.CCR-12-2246.
Wu SG, Shih JY. Management of acquired resistance to EGFR TKI–targeted therapy in advanced non-small cell lung cancer. Mol Cancer. 2018;17(1):1–14. https://doi.org/10.1186/s12943-018-0777-1.
Rodak O, Peris-Díaz MD, Olbromski M, Podhorska-Okołów M, Dzięgiel P. Current landscape of non-small cell lung cancer: epidemiology, histological classification, targeted therapies, and immunotherapy. Cancers. 2021;13(18):4705. https://doi.org/10.3390/cancers13184705.
Cui Q, Hu Y, Cui Q, Wu D, Mao Y, Ma D, et al. Osimertinib rechallenge with bevacizumab vs chemotherapy plus bevacizumab in EGFR-mutant NSCLC patients with osimertinib resistance. Front Pharmacol. 2022;12:3724. https://doi.org/10.3389/fphar.2021.746707.
Osude C, Lin L, Patel M, Eckburg A, Berei J, Kuckovic A, et al. Mediating EGFR-TKI resistance by VEGF/VEGFR autocrine pathway in non-small cell lung cancer. Cells. 2022;11(10):1694. https://doi.org/10.3390/cells11101694.
Le X, Nilsson M, Goldman J, Reck M, Nakagawa K, Kato T, et al. Dual EGFR-VEGF pathway inhibition: a promising strategy for patients with EGFR-mutant NSCLC. J Thorac Oncol. 2021;16(2):205–15. https://doi.org/10.1016/j.jtho.2020.10.006.
Naumov GN, Nilsson MB, Cascone T, Briggs A, Straume O, Akslen LA, et al. Combined vascular endothelial growth factor receptor and epidermal growth factor receptor (EGFR) blockade inhibits tumor growth in xenograft models of EGFR inhibitor resistance. Clinl Canc Res. 2009;15(10):3484–94. https://doi.org/10.1158/1078-0432.CCR-08-2904.
Seto T, Kato T, Nishio M, Goto K, Atagi S, Hosomi Y, et al. Erlotinib alone or with bevacizumab as first-line therapy in patients with advanced non-squamous non-small-cell lung cancer harbouring EGFR mutations (JO25567): an open-label, randomised, multicentre, phase 2 study. Lancet Oncol. 2014;15(11):1236–44. https://doi.org/10.1016/S1470-2045(14)70381-X.
Saito H, Fukuhara T, Furuya N, Watanabe K, Sugawara S, Iwasawa S, et al. Erlotinib plus bevacizumab versus erlotinib alone in patients with EGFR-positive advanced non-squamous non-small-cell lung cancer (NEJ026): interim analysis of an open-label, randomised, multicentre, phase 3 trial. Lancet Oncol. 2019;20(5):625–35. https://doi.org/10.1016/S1470-2045(19)30035-X.
Nakagawa K, Garon EB, Seto T, Nishio M, Aix SP, Paz-Ares L, et al. Ramucirumab plus erlotinib in patients with untreated, EGFR-mutated, advanced non-small-cell lung cancer (RELAY): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(12):1655–69. https://doi.org/10.1016/S1470-2045(19)30634-5.
Chiu C, Lin M, Wei Y, Chang G, Su W, Hsia T, et al. Efficacy and safety of ramucirumab (RAM) plus erlotinib (ERL) in Taiwanese patients with untreated, EGFR-mutated metastatic non-small-cell lung cancer (mnsclc) participating in the global phase 3 RELAY study. In Presented at the Taiwan Society of Pulmonary and Critical Care Medicine—2020 Annual Meeting; Taipei, Taiwan. Poster PA40.
Dogan S, Shen R, Ang DC, Johnson ML, D’Angelo SP, Paik PK, et al. Molecular epidemiology of EGFR and KRAS mutations in 3,026 lung adenocarcinomas: higher susceptibility of women to smoking-related KRAS-mutant cancers. Clin Canc Res. 2012;18(22):6169–77. https://doi.org/10.1158/1078-0432.CCR-11-3265.
Royston P, Parmar MK. Restricted mean survival time: an alternative to the hazard ratio for the design and analysis of randomized trials with a time-to-event outcome. BMC Med Res Methods. 2013;13(1):1–15. https://doi.org/10.1186/1471-2288-13-152.
Cross DA, Ashton SE, Ghiorghiu S, Eberlein C, Nebhan CA, Spitzler PJ, et al. AZD9291, an irreversible EGFR TKI, overcomes T790M-mediated resistance to EGFR inhibitors in lung cancer novel mutant-selective EGFR inhibitor overcomes drug resistance. Canc Discov. 2014;4(9):1046–61. https://doi.org/10.1158/2159-8290.CD-14-0337.
Soria JC, Ohe Y, Vansteenkiste J, Reungwetwattana T, Chewaskulyong B, Lee KH, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. New Eng J Med. 2018;378(2):113–25. https://doi.org/10.1056/NEJMoa1713137.
Hendriks LE, Kerr KM, Menis J, Mok TS, Nestle U, Passaro A, et al. Oncogene-addicted metastatic non-small-cell lung cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. 2023;34(4):339–57. https://doi.org/10.1016/j.annonc.2022.12.009.
Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman JR, Bharat A, et al. Non-small cell lung cancer, Version 3.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2022;20(5):497–530. https://doi.org/10.6004/jnccn.2022.0025.
Jaiyesimi IA, Owen DH, Ismaila N, Blanchard E, Celano P, Florez N, et al. Therapy for stage IV non–small-cell lung cancer with driver alterations: ASCO living guideline, version 20223. J Clin Oncol. 2023;41(11):e31–41. https://doi.org/10.1200/JCO.22.02782.
Ramalingam SS, Gray JE, Ohe Y, Cho BC, Vansteenkiste J, Zhou C, et al. Osimertinib vs comparator EGFR-TKI as first-line treatment for EGFRm advanced NSCLC (FLAURA): final overall survival analysis. Ann Oncol. 2019;30:v914–5. https://doi.org/10.1056/NEJMoa1913662.
Nishio M, Seto T, Reck M, Garon EB, Chiu CH, Yoh K, et al. Ramucirumab or placebo plus erlotinib in EGFR-mutated, metastatic non-small-cell lung cancer: East Asian subset of RELAY. Cancer Sci. 2020;111(12):4510–25. https://doi.org/10.1111/cas.14655.
Nishio K, Seto T, Nishio M, Reck M, Garon EB, Sakai K, et al. Ramucirumab plus erlotinib versus placebo plus erlotinib in patients with untreated metastatic EGFR-mutated NSCLC: RELAY Japanese Subset. JTO Clin Res Rep. 2021;2(6):100171. https://doi.org/10.1016/j.jtocrr.2021.100171.
Zhou Q, Xu CR, Cheng Y, Liu YP, Chen GY, Cui JW, et al. Bevacizumab plus erlotinib in Chinese patients with untreated, EGFR-mutated, advanced NSCLC (ARTEMIS-CTONG1509): a multicenter phase 3 study. Canc Cell. 2021;39(9):1279–91. https://doi.org/10.1016/j.ccell.2021.07.005.
Yamamoto N, Seto T, Nishio M, Goto K, Okamoto I, Yamanaka T, et al. Erlotinib plus bevacizumab vs erlotinib monotherapy as first-line treatment for advanced EGFR mutation-positive non-squamous non-small-cell lung cancer: survival follow-up results of the randomized JO25567 study. Lung Cancer. 2021;151:20–4. https://doi.org/10.1016/j.lungcan.2020.11.020.
Li J, Gu J. Diarrhea with epidermal growth factor receptor tyrosine kinase inhibitors in cancer patients: a meta-analysis of randomized controlled trials. Crit Rev Oncol Hematol. 2019;134:31–8. https://doi.org/10.1016/j.critrevonc.2018.12.001.
Fabbrocini G, Panariello L, Caro G, Cacciapuoti S. Acneiform rash induced by EGFR inhibitors: review of the literature and new insights. Skin Appendage Disord. 2015;1(1):31–7. https://doi.org/10.1159/000371821.
Pandey AK, Singhi EK, Arroyo JP, Ikizler TA, Gould ER, Brown J, et al. Mechanisms of VEGF (vascular endothelial growth factor) inhibitor-associated hypertension and vascular disease. Hypertension. 2018;71(2):e1-8. https://doi.org/10.1161/HYPERTENSIONAHA.117.10271.
He Y, Zhou C. Tyrosine kinase inhibitors interstitial pneumonitis: diagnosis and management. Transl Lung Canc Res. 2019;8(Suppl 3):S318. https://doi.org/10.21037/tlcr.2019.05.02.
Ando M, Okamoto I, Yamamoto N, Takeda K, Tamura K, Seto T, et al. Predictive factors for interstitial lung disease, antitumor response, and survival in non-small-cell lung cancer patients treated with gefitinib. J Clin Oncol. 2006;24(16):2549–56. https://doi.org/10.1200/JCO.2005.04.9866.
Acknowledgments
The authors would like to acknowledge Jane Snowball and Gill Gummer (Rx Communications, Mold, UK) for medical writing assistance with the preparation of this manuscript, funded by Eli Lilly and Company.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Eli Lilly and Company.
Conflict of interest
Chao-Hua Chiu has received consulting fees or honorarium from Amgen, AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Chugai Pharmaceutical, Eli Lilly and Company, Janssen, Merck KGaA, Merck Sharp & Dohme, Novartis, Ono Pharmaceutical, Pfizer, Roche, Shionogi and Takeda. Gee-Chen Chang, Meng-Chih Lin, Jian Su, Wu-Chou Su and Yu-Feng Wei have no conflicts to declare. Te-Chun Hsia has received payment for lectures including service on speakers bureaus from AstraZeneca, Boehringer Ingelheim, Eli Lilly and Company, Roche, Takeda, Merck Sharp & Dohme, Merck KGaA, Bristol Myers Squibb and Amgen. Jin-Yuan Shih has received grants from Roche and Genconn Biotech; consulting fees or honorarium from ACT Genomics, Amgen, Genconn Biotech, AstraZeneca, Roche, Bayer, Boehringer Ingelheim, Eli Lilly and Company, Pfizer, Novartis, Merck Sharp & Dohme, Chugai Pharmaceutical, Takeda, CStone Pharmaceuticals, Janssen, TTY Biopharm, Orient EuroPharma, Mundipharma, Ono Pharmaceutical and Bristol Myers Squibb; and travel support from AstraZeneca, Roche, Boehringer Ingelheim and Chugai Pharmaceutical. Anne Kuei-Fang Wang, Min-Hua Jen and Tarun Puri are employees of Eli Lilly and Company with stock options.
Authors contributions
All authors contributed to the study conception/design or acquisition, analysis and interpretation of the data. All authors critically revised the manuscript for important intellectual content and have read and approved the final manuscript.
Ethics approval
The study was conducted in accordance with the ethical principles of the Declaration of Helsinki. The protocol and amendments were approved by the ethics committees of all participating centers.
Informed consent
Informed consent was obtained from all patients prior to participating in the study.
Data availability
Eli Lilly provides access to all individual participant data collected during the trial, after anonymisation, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the USA and EU and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once they are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, and blank or annotated case report forms will be provided in a secure data sharing environment for up to 2 years per proposal. For details on submitting a request, see the Vivli website.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chiu, CH., Lin, MC., Wei, YF. et al. Efficacy and Tolerability of Ramucirumab Plus Erlotinib in Taiwanese Patients with Untreated, Epidermal Growth Factor Receptor-Mutated, Stage IV Non-small Cell Lung Cancer in the RELAY Study. Targ Oncol 18, 505–515 (2023). https://doi.org/10.1007/s11523-023-00975-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-023-00975-5