Abstract
Mobile health (mHealth) messaging has been used to enhance quitting. Optimal sequencing of more personalized and intensive interventions may increase abstinence for mHealth non-responders (continuing smokers). We aim to test the effectiveness and cost of an adaptive design intervention based on chat-based personalized instant messaging (PIM) versus that based on regular instant messaging (RIM; non-personalized) on validated abstinence. Sequential, multiple assignment randomized trial proactively recruited adult daily cigarette smokers in Hong Kong. At baseline, participants received brief cessation advice plus referral assistance to cessation services and were randomized to receive PIM (PIM group, n = 422) or RIM (RIM group, n = 422). At 1 month, PIM non-responders were further randomized (ratio 3:1) to receive either combined cessation interventions (CCI, including multi-media messages, nicotine replacement therapy sampling, incentive for service referral, phone counselling, family/peer group chat) or maintained PIM for 2 months. RIM non-responders were further randomized (ratio 1:3) to receive PIM or maintained RIM. Responders (quitters) in either group continued to receive the respective initial intervention. Bio-validated abstinence at 6 months by intention-to-treat. The 844 participants were mostly male (82.3%). At 1 month, 370 (87.7%) and 373 (88.4%) non-responded to PIM and RIM, respectively. Of non-responders, 273 (73.8%) received CCI and 91 (24.4%) received PIM. At 6 months, PIM group had non-significantly higher validated abstinence than RIM group (10.2% vs. 8.3%, risk ratio [RR] 1.23, 95%CI 0.80 to 1.88) at doubled cost (US$33,228.8 vs. 15,985.5). In non-responders, receiving CCI (vs. maintained PIM: 4.8% vs. 6.2%, RR 0.77, 95%CI 0.30 to 1.97) or PIM (vs. maintained RIM: 3.3% vs 5.7%, RR 0.58, 95%CI 0.17 to 1.95) did not increase validated abstinence. The PIM-based adaptive intervention did not significantly increase validated abstinence than that of non-personalized IM. Non-responders to PIM or RIM did not benefit from more intensive interventions. ClinicalTrials.gov Identifier: NCT03992742
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Text messaging and app-based interventions were effective in increasing smoking abstinence (Whittaker et al., 2019), probably through improving perceived behavioural and psychosocial support for quitting (Hoeppner et al., 2017). In Hong Kong, we reported that instant messaging (IM) tools (e.g. WhatsApp) had quickly displaced SMS text messages because chat-based interventions through IM were more convenient, low-cost and interactive in providing individual behavioural counselling (Luk et al., 2019). Our cluster randomized controlled trials (RCT) showed the efficacy of IM-based interventions in increasing abstinence in community (Wang et al., 2019) and workplace-recruited smokers (Weng et al., 2022). However, only a small proportion of our participants (around 17.0%) interacted with the counsellors. Most non-interacting smokers were not motivated (Wang et al., 2019) or never attempted to quit (Weng et al., 2022), thus less likely to quit with the low-intensity smoking cessation (SC) support.
More personalized counselling that tailored to smoking and quitting-related characteristics (like that in face-to-face counselling) may enhance SC support. Identifying those who are more likely to fail in quitting at an early stage for providing more personalized and/or intensive support may increase abstinence. Adaptive clinical trials usually step-up or change the intervention to be more intensive for participants with suboptimal responses to initial minimal intervention with the assumption that greater support (i.e. more intensive intervention) should be provided to change non-responders’ behaviours to produce stronger effects (Bhatt & Mehta, 2016). Triaging smokers who were non-responding to usual care at 3 months for long-term counselling significantly increased abstinence at 12 months (odds ratio = 4.41, P < 0.001) (Burns et al., 2016). In our SC trial using IM-based intervention (Wang et al., 2019), 87.3% participants (461/528) who remained smoking at 1 month failed to quit at 6 months, and 70% participants (44/63) who reported quitting at 1 month-maintained abstinence at 6 months. Providing more intensive or personalized interventions for the early non-responding participants may enhance the support and improve cessation outcomes.
The sequential, multiple assignment, randomized trial (SMART) design has been used in mental health (e.g. depression) (Bothwell et al., 2018), substance abuse (Freeman et al., 2020; Morgenstern et al., 2021) and weight loss (Naar et al., 2019) trials to compare different sequences of medications and behavioural treatments or treatment tactics (e.g. treatment delivery methods). Our search in PubMed and ClinicalTrials.gov found 3 ongoing SMARTs for SC: one incorporating lung cancer screening on high risk smokers (Fu et al., 2017), one facilitating the use of Quitline for smokers in Community Health Centers (Fernandez et al., 2020), and one testing post-relapse treatment for relapse recovery (NCT02564315), but no result has been reported.
In the present trial, we used the SMART design to test the effectiveness of different sequenced adaptive-design interventions (ADIs) (Murphy, 2005) with a 2-stage randomization: (1) randomized participants for chat-based personalized instant messaging (PIM) or regular instant messaging (RIM) at first stage, and (2) subsequently randomized participants, who were not responsive to the initial intervention (non-responders, self-reported smoking in the past 7 days), to the higher intensity combined cessation interventions (CCI, for PIM non-responders) or PIM (for RIM non-responders). Self-determined CCI was designed to increase the non-responders’ motivation to quit via positive attitudes, social influence and improved self-efficacy (Sheeran et al., 2020). Prior trials and reviews have shown the effectiveness of these CCI components, including multi-media message (Brendryen & Kraft, 2008), nicotine replacement therapy sampling (Hartmann-Boyce et al., 2018; Cheung et al., 2020), financial incentive for active referral (Weng et al., 2020; Wang et al., 2017a), phone counselling (Matkin et al., 2019) and social support (Faro et al., 2023). Specifically, we tested 2 research questions: (1) by the first randomization, whether an mHealth-based ADI that initiated with personalized chatting is more effective than that initiated with regular messages; (2) by the second randomization of non-responders, whether to step-up the initial intervention with more intensive components will be more effective than maintaining (i.e. continuing with) the initial intervention.
Methods
Study Design
This was a two-arm, parallel group, assessor-blinded SMART nested within a Quit to Win (QTW) contest organized by the Hong Kong Council on Smoking and Health (Wang et al., 2019; Weng et al., 2020; Wang et al., 2017a; Weng et al., 2021). The trial protocol has been approved by the Institutional Review Board of the University of Hong Kong/ Hospital Authority Hong Kong West Cluster, registered with ClinicalTrials.gov (NCT03992742), and published elsewhere (Zhao et al., 2022). Written informed consents were obtained.
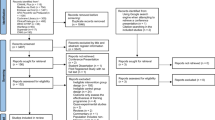
Figure 1 shows the Consolidated Standards of Reporting Trials (CONSORT) diagram for reporting an adaptive design (Dimairo et al., 2020). In stage 1, after baseline data collection, all participants received brief cessation advice plus referral to smoking cessation services and were randomized to receive personalized instant messaging (PIM group) or regular instant messaging (RIM group) at 1:1 allocation ratio. In stage 2, after 1-month follow-up, participants were classified as responders (self-reported quitters in the past 7 days) and non-responders (continuing smokers, even a single puff in the past 7 days). By intention-to-treat, participants lost to follow-up were treated as non-responders (assuming no change in smoking behaviour since baseline). Non-responders in the PIM group were further randomized to receive additional combined cessation interventions (P-CCI) or maintained PIM (P-rPIM). Non-responders in the RIM group were further randomized to receive PIM (R-PIM) or maintained RIM (R-rRIM). Responders in PIM (P-PIM) and RIM group (R-RIM) groups continued to receive the save intervention respectively. The total duration of intervention for all participants was 3 months from baseline with 4 follow-ups at 1, 2, 3 and 6 months from treatment initiation.
CONSORT flowchart for reporting a response-adaptive randomization adaptive design. CE, carbon monoxide; pp, parts per million; QTW, Quit to Win; PIM, Personalized Instant Messaging; RIM, Regular Instant Messaging; IIT, Intent-to-treat, participants with missing outcomes were treated as smoking (non-responders); P-CCI, re-randomized for Combined Cessation Intervention; P-rPIM, re-randomized for maintained PIM; P-PIM, Continued PIM; R-PIM, re-randomized for PIM; R-rRIM, re-randomized for maintained RIM; R-RIM, continued RIM; VA, validated abstinence
Settings and Participants
Participants were individually recruited from 70 community sites, including shopping malls, housing estates, transportation hubs, throughout all 18 districts in Hong Kong. At each recruitment activity, SC advisors proactively approached smokers who were smoking, screened their eligibility and invited them for participation using a “foot-in-the-door” technique (Freedman & Fraser, 1966). All advisors (n = 69, mainly university students) were trained in a half-day workshop and completed a pre- and post-workshop test of their knowledge, attitude and practice in recruitment activity. At least one research team members monitored the recruitment process and provided support as needed. Advisors were instructed to follow the standardized recruitment script and intervention checklist.
Hong Kong residents aged 18 years or older who smoked daily in the preceding 3 months (verified by an exhaled carbon monoxide (CO) level ≥ 4 part per million (ppm)), could communicate in Cantonese and were able to use an instant messaging app were eligible. Smokers who had physical or cognitive difficulties in communication or were currently participating in other smoking cessation programs were excluded.
Randomization and Masking
Participants were computer-randomized within 3 days after enrolment. The first randomization assigned participants into the PIM or RIM group with random permuted block sizes of 2, 4 and 6 in an allocation ratio of 1:1. At 1 month, a second randomization was conducted on non-responders. In the PIM group, non-responders were further randomized to P-CCI or P-rPIM subgroup with an allocation ratio of 3:1 and block sizes of 4, 8 or 12. Similarly, non-responders in the RIM group were further randomized to R-PIM or R-rRIM subgroup, with an allocation ratio of 1:3 and block sizes of 4, 8 or 12. The different allocation ratio in the second randomization was designed to maximize the statistical power to compare P-CCI with R-rRIM subgroup, which was the co-primary comparison of the trial (refer to Outcomes below). Randomization was conducted by a co-investigator (WX) who was not involved in recruitment and intervention delivery. SC advisors, outcome assessors and statistical analysts were blinded to the group allocation.
Interventions
At baseline, all participants received brief face-to-face SC advice plus active referral to SC service using the AWARD model (Ask, Warn, Advise, Refer, Do-it-again, Appendix 1), which had been tested in our prior trials (Wang et al., 2019; Weng et al., 2020; Wang et al., 2017a; Weng et al., 2021; Cheung et al., 2017; Wang et al., 2017b; Cheung et al., 2021).
Personalized instant messaging (PIM)
Participants randomized to receive the PIM intervention were provided personalized behaviour support delivered through an instant messaging app (WhatsApp or WeChat) for 3 months (2 months for R-PIM subgroup participants, see Regular instant messaging below). Based on the Transtheoretical Behaviour Change Model (TTM) (Prochaska & DiClemente, 1982), we developed 3 sets of fix-scheduled messages tailored to participants’ intention to quit (within next 7 days, 30 days and 60 days/undecided, Appendix 1). Research team members customized the messages to the sex, age, daily cigarette consumption and motivation (e.g. quit for better health, for improved family relationship) of the participants and initiated real-time, interactive conversation once participants replied.
Overall, the PIM intervention aimed to engage and motivate participants to develop a personalized quit plan, monitor their quitting progress, provide individualized behavioural and psychological support, and enhance the intervention effect by offering combined behavioural and pharmacological support. For responders (P-PIM subgroup), messages and interactive chatting in stage 2 mainly focused on relapse prevention. The behavioural change techniques (BCTs) were used to maximize self-regulation and promote adjuvant activities for quitting (Michie et al., 2011). Motivational Interviewing (MI) skills (Lindson et al., 2019) were adopted throughout the conversation to improve the motivation to change with a supportive environment.
Combined Cessation Interventions (CCI)
For non-responders in PIM group allocated to receive CCI (P-CCI subgroup), research team members explained and assisted them to choose one or more preferred cessation supports including (1) multi-media messages, provided once weekly in pictures, web links and short videos to encourage engagement; (2) 1-week dosage of nicotine replacement therapy sampling (NRT-S, gum or patch; Nicotinell. GlaxoSmithKline, Brentford, London, UK) to motivate quit attempt and alleviate withdrawal symptoms; (3) small financial incentive (HK$100, ≈ US$ 12.8) for using smoking cessation service, (4) an in-depth phone counselling session guided by MI and (5) family or close friend (as a source of social support) group chat moderated by a research team member. P-CCI participants who were lost to follow-up or could not make the choice during follow-up received multi-media messages (default option) in addition to the PIM. Those who declined to receive any CCI continued to receive PIM.
The NRT-S and financial incentive were sent by post to participants who were willing to use medication assistance and verbally committed to use any smoking cessation services within the next 2 months. The dose of the NRT-S provided depended on participants’ daily cigarette consumption: 2 mg nicotine gum or 14 mg nicotine patch for those who smoked < 20 cigarettes per day and 21 mg nicotine patch for those who smoked ≥ 20 cigarettes per day. Contraindications were checked and side effects were monitored through PIM and follow-ups. Phone counselling was scheduled as required by participants. The detailed procedures are shown in Appendix 1.
Regular Instant Messaging (RIM)
Regular smoking cessation-related text messages were sent in a tapering schedule from twice weekly in the first month to once a week in the following 2 months. Additional 4 messages were delivered at 1, 2, 3 and 6 months as follow-up reminders (20 in total). RIM was unidirectional without real-time reply. For RIM participants who were allocated to receive PIM in stage 2 (R-PIM subgroup), we notified them of a transfer of intervention that allowed interactive support in the coming 2 months. Further messages were scheduled based on their baseline intention to quit (intended to quit within next 30 days or 60 days/undecided).
Intervention Fidelity
The PIM intervention was delivered by two master-level smoking cessation research team members trained in TTM and MI counselling skills. The logistics of providing the CCI were supervised by experienced research team members. The message dialogues and phone counselling were recorded and randomly checked with case discussion at least weekly.
Outcomes
Responders vs. Non-responders
At the end of stage 1 intervention, all participants were assessed for intervention response (incorporated with 1-month follow-up). A responder was defined as no smoking in the past 7 days (7-day point-prevalence abstinence, PPA), whereas a non-responder was defined as smoking for even a puff in the past 7 days. Participants who were lost to follow-up were treated as non-responders (by intention-to-treat) for the subsequent interventions (West et al., 2005).
Primary and Secondary Outcomes
The primary outcome was smoking abstinence validated biochemically at 6 months after treatment initiation using exhaled carbon monoxide (< 4 ppm, by piCO Smokerlyzer) and salivary cotinine (< 10 ng/ml, by NicAlert test strip) (Javors et al., 2005; Cooke et al., 2008). Biochemically validated abstinence at 3 months (end of treatment) was the main secondary outcome. Other secondary outcomes included self-reported 7-day PPA, smoking reduction by at least 50% of baseline consumption, quit attempt (abstinence for ≥24 h) and smoking cessation service use, defined by any use of the treatments delivered by existing smoking cessation service providers (e.g. counselling, medication, acupuncture).
Group Comparisons
Assuming a more intensive and personalized mHealth-based ADI would be more effective regardless of subsequent changes after the second randomization, we primarily compared quitting outcomes between the PIM group with the RIM group (Primary comparison). We also assumed that participants non-responding to the stage 1 mHealth interventions would be benefitted from subsequent more intensive cessation supports. First, those who received PIM augmented by CCI (P-CCI subgroup) were compared with those who received RIM alone (R-rRIM) (Co-primary comparison) to investigate the effect of the most intensive adaptive intervention versus the least intensive mHealth support in non-responders. Second, we examined the quitting outcomes of CCI vs. PIM (P-CCI subgroup vs. P-rPIM subgroup) and PIM vs. RIM (R-PIM subgroup vs. R-rRIM subgroup) in non-responders. Last, in responders, we examined the quitting outcomes of continuous PIM vs. RIM (P-PIM subgroup vs. R-RIM subgroup).
Sample Size
The required sample size was calculated based on an risk ratio (RR) of 1.83 on validated abstinence at 6 months reported by an earlier meta-analysis of mHealth interventions (Whittaker et al., 2016). Assuming a biochemically validated quit rate of 5.0% in participants receiving RIM at 6 months based on our previous trial (Wang et al., 2019), 1200 participants will be needed (600 each group) to achieve 80% power with a 5% false-positive error rate using an allocation ratio of 1:1. Given the 7-day PPA reported in our previous mHealth trial at 1 month (intervention: 10.7% vs. control:7.7%) (Wang et al., 2019), we assumed 64 (600*10.7%) and 46 (600*7.7%) participants would be defined as responders in the PIM and RIM group. Our pilot trial reported an effect of 1.12 when comparing 2 months of PIM plus 1-week nicotine replacement therapy vs. RIM on self-reported abstinence at 3 months (Zhao et al., 2021). Using an allocation ratio of 3:1 and an RR of 2.05 (1.83*1.12) with a 5% false-positive error rate, a sample size of 402 [(600-64)*3/4] in P-CCI and 416 [(600-46)*3/4] in R-rRIM would have a power of 0.81 to test the validated quit rate at 6 months by co-primary comparison. A total of 844 smokers were recruited by the end of the recruitment (70.3%) due to frequent disruptions of the social movement during the same period in Hong Kong.
Statistical Analysis
Intention-to-treat analyses were used with missing outcomes considered to have no change from baseline (West et al., 2005). The primary and secondary outcomes between the study groups were compared using Poisson regression models to yield RRs. Sensitivity analyses were conducted including (1) regression models of the quitting outcomes were repeated with adjustment for baseline imbalanced factors, (2) multiple imputation by chained equation models to impute missing outcomes, using study group, sex, age, education attainment, daily cigarette consumption, time to first cigarette since awake, previous quit attempts and intention to quit (baseline data) and (3) complete case analysis by excluding participants with missing quitting outcomes.
Post hoc analyses were done to compare the baseline smoking profile by intervention responses at 1 month and the intervention effect in subgroups of sex, age, educational attainment, daily cigarette consumption and intention to quit within 30 days. The use of CCI and the effectiveness of using the CCI on the primary outcome was analysed, adjusting for sex, age, nicotine dependency, previous quit attempt and intention to quit. We used Stata/MP v15.1 (Stata Corp, Texas, USA) for all statistical analyses. The operating cost of interventions, including the personnel for participant recruitment and intervention delivery and materials (e.g. print-based materials, NRTS), were calculated in both study groups.
Results
Participants Flow and Characteristics
Figure 1 shows that of 1089 smokers screened for eligibility, 844 (82.3% male, Table 1) were eligible and participated (77.5%). Participants were individually randomized into the PIM group (N = 422) or the RIM group (N = 422). At 1 month, 52 (12.3%) and 49 participants (11.6%) in the PIM and RIM group were classified as responders, respectively. By intention-to-treat, 273 (73.8%) and 97 (26.2%) of the 370 non-responders (including those who were lost to follow-up) in the PIM group were further randomized respectively to P-CCI and P-rPIM subgroup (ratio 3:1). In the RIM group, 91 (24.4%) and 282 (75.6%) of the 373 non-responders were further randomized to R-PIM and R-rRIM subgroup (ratio 1:3). Retention rates were 77.1% (n = 651) at 1 month, 70.3% (n = 593) at 2 months, 68.6% (n = 579) at 3 months and 79.5% (n = 671) at 6 months.
Of all 844 participants, 49.3% had a low nicotine dependence level, 23.6% had quit attempts within the past year and 30.6% intended to quit within the next 7 days. Table 1 shows that demographic and smoking characteristics were similar between the PIM and RIM group except that RIM group had more participants with a monthly household income between 25,000 to 60,000 (P = 0.02). Compared with daily cigarette smokers in the general population in 2019 (Census & Statistics Department (Hong Kong SAR government), 2019), the trial participants were younger (47.5% vs. 26.0% aged 18–39), had higher daily cigarette consumption (mean 14.1 vs. 12.7) and had more with past quit attempt (70.6% vs. 32.6%) (Table S1). Participants classified as non-responders at 1 month had a higher daily cigarette consumption (mean ± SD: 14.3 ± 8.3 vs. 12.3 ± 7.7, P = 0.02), perceived quitting as less important (6.9 ± 2.6 vs. 8.0 ± 2.2, P < 0.001) and had a lower confidence in quitting (5.3 ± 2.5 vs. 6.8 ± 2.6, P < 0.001) at baseline than those who classified as responders (Table S2). Table S2 also shows that more non-responders (vs. responders) had no intention to quit within next 30 days (47.1% vs. 20%, P < 0.001) and Table S3 shows that they had lower retention rates at 2-, 3- and 6-month follow-ups.
Smoking Cessation Outcomes by Primary Group Comparison
Of 177 participants who reported smoking abstinence at 6 months, 78 (44.1%) passed the biochemical validation test. The validation participation rate of the PIM group was higher than the RIM group but the difference was not statistically significant (50.0% vs. 38.5%, P = 0.09).
Table 2 shows that the PIM group had a non-significantly higher biochemically validated abstinence than the RIM group at 6 months (10.2% vs. 8.3%, RR 1.23, 95%CI 0.80 to 1.88, P = 0.34). The corresponding validated abstinence rates at 3 months were 8.8% and 6.9% (RR 1.28, 95%CI 0.80 to 2.04, P = 0.31), respectively. Self-reported 7-day PPA, smoking reduction, quit attempt and use of smoking cessation service at 3 and 6 months were similar between the two groups. Table S4 shows similar results from analyses using multivariable regressions (adjusting for imbalanced baseline covariates), multiple imputation and complete case models. Table S5 shows that the effect of PIM vs. RIM was significant only in females (RR (female vs. male): 14.3 vs. 0.88, P for interaction = 0.03) and significantly stronger in middle-aged smokers (RR (45–59 years vs. 60 or above): 1.52 vs. 0.71, P for interaction = 0.049).
Smoking Cessation Outcomes by Secondary Group Comparisons
In both group non-responders, offering CCI (P-CCI subgroup, n = 273) did not show higher validated abstinence than maintained RIM (R-rRIM subgroup) at both 3 (3.7% vs. 3.9%, RR 0.94, 95%CI 0.41 to 2.18) and 6 months (4.8% vs. 5.7%, RR 0.84, 95%CI 0.41 to 1.71) (Table 2). In the P-CCI subgroup, 167 (61.2%) participants received at least 1 of the CCIs at 1 month, 95 (34.8%) were lost to follow-up or did not choose any of the CCI, and 11 (4.0%) declined to receive any CCI. Table S6 shows that among the 167 participants who received any of the CCIs, 136 (81.4%) received multi-media messages, 83 (49.7%) received NRT-S, 29 (17.4%) received financial incentive for active referral to SC service, 149 (89.2%) received phone counselling and only 1 (0.6%) received social support group chat. Receipt of either the multi-media messages, NRT-S, financial incentive or phone counselling increased validated abstinence than receipt of none of the CCI (adjusted RR 1.33 to 2.30), though the increases were not statistically significant (P = 0.15 to 0.71). Table S7 shows that receipt of any of the CCI showed a non-significantly higher validated abstinence (6.0% vs. 2.8%, P = 0.25), self-reported abstinence (14.4% vs. 11.3%, P = 0.47), smoking reduction (26.4% vs. 22.6%, P = 0.49), and were significantly more likely to made quit attempt (44.3% vs. 30.2%, P = 0.025) and use smoking cessation services (27.5% vs. 7.6%, P < 0.001) at 6 months. Table S6 also shows that receipt of more CCIs also showed higher validated abstinence at 6 months (received 4 of the CCIs vs. none: 18.2% vs. 2.8%, P = 0.03).
In the PIM group non-responders, Table 3 shows that CCI (P-CCI subgroup) had non-significantly lower validated or self-reported abstinence than maintained PIM (P-rPIM subgroup) at 3 and 6 months (P range 0.29–0.85). Similar results were found in the RIM group non-responders, with a significantly lower self-reported abstinence (6.6% vs. 18.1%, RR = 0.36, 95%CI 0.16–0.82) in PIM (R-PIM subgroup) than maintained RIM (R-rRIM subgroup) at 6 months.
More PIM responders (P-PIM subgroup) had validated abstinence than RIM responders (R-RIM subgroup) at 3 (44.2% vs. 32.7%, RR 1.35, 95%CI 0.82 to 2.50, P = 0.24) and 6 month (46.2% vs. 32.7%, RR 1.41, 95%CI 0.86 to 2.33, P = 0.18), but the differences were not statistically significant.
Cost-Effectiveness Analyses
Table 4 shows that the total intervention cost was US$33228.8 in the PIM group and $15985.5 in the RIM group. The average cost per validated abstinent participant at 6 months was 70% higher in the PIM group ($772.8, 95%CI 584.1 to 1054.1) than in the RIM group ($456.7, 95%CI 333.7 to 647.5).
Discussion
This is the first SMART adaptively allocated more personalized and intensive interventions for community-recruited smokers who were non-responding to the mHealth messaging support to increase smoking abstinence. The PIM-based ADI led to a non-significantly higher validated abstinence rates than the RIM-based ADI at 3- and 6-month follow-ups. Integrating with additional CCI for smokers who non-responded to PIM did not significantly affect smoking abstinence as compared to maintained PIM. In RIM non-responders, receiving further personalized chatting subjected to a lower abstinence rate compared with maintained RIM. Considering the small intervention effect and the nearly doubled cost per validated abstinence in the PIM group, this study does not support replacing the less intensive IM with personalized IM cessation intervention.
The SMART is designed to test the sequencing of evidence-based interventions, efficacy testing of individual intervention does not need to be duplicated and thus a control group (usual care) was not included. Both the PIM and RIM group received brief cessation advice and were actively referred to existing smoking cessation services. Such a method was found effective in increasing smoking abstinence among proactively recruited community smokers (Wang et al., 2017a). Albeit delivered in a lower intensity, messages provided in the RIM group were also guided by the BCTs, tested in prior mHealth smoking cessation trials (Wang et al., 2019; Weng et al., 2022; Zhao et al., 2021) and covered most cessation-related information as those provided in the PIM group. The similarity in the content of the PIM and RIM may be the main reason for the lack of detectable intervention effect. The result was consistent with other studies found that the intensity of the mHealth-based intervention, either with (Abroms et al., 2014) or without (Liao et al., 2018) personalization to the baseline smoking profile, did not significantly increase abstinence rate at 6 months.
However, in responders receiving continuous interventions, PIM showed higher validated abstinence than RIM at both 3 and 6 months (RR ranged 1.35 to 1.41). Non-significant results were probably due to the small sub-sample size (n = 101). With the ability to provide real-time responses to participants for individualized barriers or questions, PIM was potentially more effective in promoting long-term abstinence and preventing relapse for the early quitters. Integrating personalized mHealth support for treatment seekers or smoking cessation service users may increase successful long-term cessation. We also found female and middle-aged participants to be more susceptible to personalized chatting (see Table S5), presumably via the improved psychological and psychosocial support and higher perceived convenience and acceptance of the intervention model (Hoeppner et al., 2017; Luk et al., 2019). The intervention could be further tailored and tested for specific populations who were more receptive to individualized psychological support (e.g. female smokers).
Comparing with the early responders, non-responders were smokers with higher nicotine dependency and lower motivation to quit, which were commonly reported factors associated with lower intervention adherence and effect (Wang et al., 2019). Contrary to the assumption that non-responders would benefit from more intensive intervention in stepped care, we found that offering high-intensity CCI for PIM non-responders or providing interactive personalized chatting for the RIM non-responders even showed harmful effects when compared with maintained PIM or RIM. A systematic review and meta-regression (42 studies, 26,168 participants) of individual-level smoking cessation interventions (e.g. text messages, telephone interview, financial incentive, brief advice) tailored to the socioeconomic characteristics also found inconclusive evidence of more personalized intervention in promoting cessation (adjusted risk ratio 1.01, 95%CI 0.81 to 1.27) (Kock et al., 2019). Until confirmation from future definitive trials, more intensive and personalized intervention for non-responders may not be necessary considering the higher cost and potential counterproductive effect. Experiences and perceptions towards receiving the sequenced interventions in non-responders warrant exploration.
An acceptance rate of 61.2% for the CCI components was considered satisfactory, though we failed to find a similar trial for comparison. Multi-media messages and phone counselling were received by more than half of the participants, with a similar increase in validated abstinence as concluded in prior trials (Xia et al., 2020) and Cochrane review (Matkin et al., 2019). The effect of offering NRT-S (adjusted RR 1.98, 95%CI 0.44 to 8.98, P = 0.38) could be undermined due to low acceptance rate (only 30.4% received) and the poor compliance in the recipients. Within the 83 P-CCI participants receiving the NRT-S, only 37.4% (31/83) reported any use, and among whom 19.4% (6/31) had complied the course of 1 week. Compared with the non-users, any use of the NRT-S tripled the validated abstinence at 6 months (RR 3.47, 95%CI 1.13, 10.63, P = 0.029). Most participants who intended to try to use smoking cessation services were offered active referral at baseline (62.9% referred); thus, the acceptance rate of 10.6% for the stage-2 incentivized referral in P-CCI subgroup was considered reasonable (compared with total referral rate of 65.2% in previous trial providing incentivized referral at baseline (Weng et al., 2021)). The family/peer support group chat showed an unexpected low acceptance rate (0.37%, 1/273), possibly due to a perceived threat to their autonomy which could arouse self-defense (Westmaas et al., 2010). Non-responders also perceived higher level of difficulty and lower level of confidence in successful quitting, which might be the reason to not involve other people in quitting. Nevertheless, received more CCIs significantly predicted quitting outcomes in non-responders. Acceptance and adherence to more intensive interventions (or more components of proven effective interventions) are the major challenge for developing effective adaptive interventions. Future studies are warranted to assess the need and experiences of the non-responders to improve the adherence and effectiveness of the intervention.
The study had several limitations. First, the trial was under-powered. All participants received proven effective brief counselling, active referral and IM interventions. Further research with full sample size and improved personalized interventions is needed. Second, although a satisfactory follow-up retention rate was achieved (79.5% at 6 months), non-response bias (selection bias) could not be excluded. Our sensitivity analyses using multiple imputations and by complete case yielded similar results to the main analyses by intention to treat. Third, participants were recruited from the community settings in Hong Kong with a low smoking prevalence (10.2% in 2019), with low average daily cigarette consumption (12.7), and predominantly male smokers, the generalizability of the findings for smokers at clinical settings or actively seeking SC treatments, and in populations with different smoking patterns in not certain.
Conclusions
The PIM-based adaptive intervention did not significantly increase validated abstinence than that of non-personalized IM. Non-responders to PIM or RIM did not benefit from more intensive interventions.
Data Availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publically available due to privacy or ethical restrictions.
Abbreviations
- ACE:
-
Adaptive designs CONSORT Extension
- ADI:
-
Adaptive-design intervention
- AWARD:
-
Ask, Warn, Advice, Refer and Do-it-again
- BCTs:
-
Behavioural Change Techniques
- CCI:
-
Combined cessation interventions
- CONSORT:
-
Consolidated Standards of Reporting Trials
- COSH:
-
Hong Kong Council on Smoking and Health
- HSI:
-
Heaviness of Smoking Index
- IRB:
-
Institutional Review Board
- ITT:
-
Intention-to-treat
- mHealth:
-
Mobile health
- MI:
-
Motivational interviewing
- NRT-S:
-
Nicotine replacement therapy sampling
- PPA:
-
Point prevalence abstinence
- ppm:
-
part per million
- PIM:
-
Personalized instant messaging
- QTW:
-
Quit to Win
- RIM:
-
Regular instant messaging
- SMART:
-
Sequential multiple-assignment randomized trial
- TTM:
-
Transtheoretical behaviour change model
References
Abroms, L. C., Boal, A. L., Simmens, S. J., Mendel, J. A., & Windsor, R. A. (2014). A randomized trial of Text2Quit. American Journal of Preventive Medicine, 47(3), 242–250.
Bhatt, D. L., & Mehta, C. (2016). Adaptive Designs for Clinical Trials. Drazen JM, Harrington DP, McMurray JJV, Ware JH, Woodcock J, eds. New England Journal of Medicine (NEJM), 375(1), 65–74.
Bothwell, L. E., Avorn, J., Khan, N. F., & Kesselheim, A. S. (2018). Adaptive design clinical trials: a review of the literature and ClinicalTrials.gov. BMJ Open, 8(2), e018320.
Brendryen, H., & Kraft, P. (2008). Happy Ending: A randomized controlled trial of a digital multi-media smoking cessation intervention. Addiction, 103(3), 478–484.
Burns, R. J., Rothman, A. J., Fu, S. S., Lindgren, B., Vock, D. M., & Joseph, A. M. (2016). Longitudinal care improves cessation in smokers who do not initially respond to treatment by increasing cessation self-efficacy, satisfaction, and readiness to quit: A mediated moderation analysis. Annals of Behavioral Medicine, 50(1), 58–69.
Cheung, Y. T. D., Cheung Li, W. H., Wang, M. P., & Lam, T. H. (2020). Delivery of a nicotine replacement therapy sample at outdoor smoking hotspots for promoting quit attempts: A Pilot Randomized Controlled Trial. Nicotine and Tobacco Research, 22(9), 1468–1475.
Cheung, Y. T. D., Jiang, N., Jiang, C. Q., et al. (2021). Physicians’ very brief (30-sec) intervention for smoking cessation on 13 671 smokers in China: A pragmatic randomized controlled trial. Addiction (Abingdon, England), 116(5), 1172–1185.
Cheung, Y. T. D., Wang, M. P., Li, H. C. W., et al. (2017). Effectiveness of a small cash incentive on abstinence and use of cessation aids for adult smokers: A randomized controlled trial. Addictive Behaviors, 66, 17–25.
Cooke, F., Bullen, C., Whittaker, R., McRobbie, H., Chen, M. H., & Walker, N. (2008). Diagnostic accuracy of NicAlert cotinine test strips in saliva for verifying smoking status. Nicotine & Tobacco Research, 10(4), 607–612.
Dimairo, M., Pallmann, P., Wason, J., et al. (2020 Jun 17). The Adaptive designs CONSORT Extension (ACE) statement: A checklist with explanation and elaboration guideline for reporting randomised trials that use an adaptive design. BMJ, 369, m115.
Faro, J. M., Chen, J., Flahive, J., et al. (2023). Effect of a machine learning recommender system and viral peer marketing intervention on smoking cessation. JAMA Network Open, 6(1), e2250665.
Fernandez, M. E., Schlechter, C. R., Del Fiol, G., et al. (2020). QuitSMART Utah: an implementation study protocol for a cluster-randomized, multi-level Sequential Multiple Assignment Randomized Trial to increase Reach and Impact of tobacco cessation treatment in Community Health Centers. Implementation Science, 15(1), 9.
Freedman, J. L., & Fraser, S. C. (1966). Compliance without pressure: The foot-in-the-door technique. Journal of Personality and Social Psychology, 4(2), 195–202.
Freeman, T. P., Hindocha, C., Baio, G., et al. (2020). Cannabidiol for the treatment of cannabis use disorder: A phase 2a, double-blind, placebo-controlled, randomised, adaptive Bayesian trial. Lancet Psychiatry, 7(10), 865–874.
Fu, S. S., Rothman, A. J., Vock, D. M., et al. (2017). Program for lung cancer screening and tobacco cessation: Study protocol of a sequential, multiple assignment, randomized trial. Contemporary Clinical Trials, 60, 86–95.
Hartmann-Boyce, J., Chepkin, S. C., Ye, W., Bullen, C., & Lancaster, T. (2018). Nicotine replacement therapy versus control for smoking cessation. Cochrane Database of Systematic Reviews, 5(5), CD000146.
Hoeppner, B. B., Hoeppner, S. S., & Abroms, L. C. (2017). How do text-messaging smoking cessation interventions confer benefit? A multiple mediation analysis of Text2Quit: Mechanisms of text-messaging effect. Addiction, 112(4), 673–682.
Javors, M. A., Hatch, J. P., & Lamb, R. J. (2005). Cut-off levels for breath carbon monoxide as a marker for cigarette smoking. Addiction, 100(2), 159–167.
Kock, L., Brown, J., Hiscock, R., Tattan-Birch, H., Smith, C., & Shahab, L. (2019). Individual-level behavioural smoking cessation interventions tailored for disadvantaged socioeconomic position: A systematic review and meta-regression. Lancet Public Health, 4(12), e628–e644.
Liao, Y., Wu, Q., Kelly, B. C., et al. (2018). Effectiveness of a text-messaging-based smoking cessation intervention (“Happy Quit”) for smoking cessation in China: A randomized controlled trial. PLOS Medicine, 15(12), e1002713.
Lindson, N., Thompson, T. P., Ferrey, A., Lambert, J. D., & Aveyard, P. (2019). Motivational interviewing for smoking cessation. Cochrane Database of Systematic Reviews, 7(7), CD006936.
Luk, T. T., Wong, S. W., Lee, J. J., Chan, S. S. C., Lam, T. H., & Wang, M. P. (2019). Exploring community smokers’ perspectives for developing a chat-based smoking cessation intervention delivered through mobile instant messaging: Qualitative study. JMIR mHealth and uHealth, 7(1), e11954.
Matkin, W., Ordóñez-Mena, J. M., & Hartmann-Boyce, J. (2019). Telephone counselling for smoking cessation. Cochrane Database of Systematic Reviews, 5(5), CD002850.
Michie, S., Hyder, N., Walia, A., & West, R. (2011). Development of a taxonomy of behaviour change techniques used in individual behavioural support for smoking cessation. Addict Behav, 36(4), 315–319.
Morgenstern, J., Kuerbis, A., Shao, S., et al. (2021). An efficacy trial of adaptive interventions for alcohol use disorder. Substance Abuse Treatment, 123, 108264.
Murphy, S. A. (2005). An experimental design for the development of adaptive treatment strategies. Statistics in Medicine, 24(10), 1455–1481.
Naar, S., Ellis, D., Idalski Carcone, A., et al. (2019). Outcomes from a sequential multiple assignment randomized trial of weight loss strategies for African American adolescents with obesity. Annals of Behavioral Medicine, 53(10), 928–938.
Prochaska, J. O., & DiClemente, C. C. (1982). Transtheoretical therapy: Toward a more integrative model of change. Psychotherapy: Theory, Research & Practice, 19(3), 276–288.
Sheeran, P., Wright, C. E., Avishai, A., et al. (2020). Self-determination theory interventions for health behavior change: Meta-analysis and meta-analytic structural equation modeling of randomized controlled trials. Journal of Consulting and Clinical Psychology, 88(8), 726–737.
Wang, M. P., Li, W. H., Cheung, Y. T., et al. (2017b). Brief advice on smoking reduction versus abrupt quitting for smoking cessation in Chinese smokers: A cluster randomized controlled trial. Nicotine and Tobacco Research, 20(1), 67–72.
Wang, M. P., Luk, T. T., Wu, Y., et al. (2019). Chat-based instant messaging support integrated with brief interventions for smoking cessation: A community-based, pragmatic, cluster-randomised controlled trial. Lancet Digit Health, 1(4), e183–e192.
Wang, M. P., Suen, Y. N., & Li, W. H. (2017a). cheung, et al. Intervention with brief cessation advice plus active referral for proactively recruited community smokers: A pragmatic cluster randomized clinical trial. JAMA Internal Medicine, 177(12), 1790–1797.
Weng, X., Lau, O. S., Ng, C. H., Li, W. H. C., Lam, T. H., & Wang, M. P. (2022). Effect of a workplace mobile phone-based instant messaging intervention on smoking cessation: A cluster-randomized controlled trial. Addiction, 117(6), 1758–1767.
Weng, X., Luk, T. T., Suen, Y. N., et al. (2020). Effects of simple active referrals of different intensities on smoking abstinence and smoking cessation services attendance: A cluster randomised clinical trial. Addiction, 115(10), 1902–1912.
Weng, X., Wu, Y., Luk, T. T., et al. (2021). Active referral plus a small financial incentive upon cessation services use on smoking abstinence: A community-based, cluster-randomised controlled trial. The Lancet Regional Health–Western Pacific, 13, 100189.
West, R., Hajek, P., Stead, L., & Stapleton, J. (2005). Outcome criteria in smoking cessation trials: Proposal for a common standard. Addiction, 100(3), 299–303.
Westmaas, J. L., Bontemps-Jones, J., & Bauer, J. E. (2010). Social support in smoking cessation: Reconciling theory and evidence. Nicotine & Tobacco Research, 12(7), 695–707.
Whittaker, R., McRobbie, H., Bullen, C., Rodgers, A., & Gu, Y. (2016). Mobile phone-based interventions for smoking cessation. Cochrane Database of Systematic Reviews, 4(4), CD006611.
Whittaker, R., McRobbie, H., Bullen, C., Rodgers, A., Gu, Y., & Dobson, R. (2019). Mobile phone text messaging and app-based interventions for smoking cessation. Cochrane Database of Systematic Reviews, 10(10), CD006611.
Xia, W., Li, H. C. W., Cai, W., et al. (2020). Effectiveness of a video-based smoking cessation intervention focusing on maternal and child health in promoting quitting among expectant fathers in China: A randomized controlled trial. PLOS Medicine, 17(9), e1003355.
Zhao, S. Z., Weng, X., Luk, T. T., et al. (2022). Adaptive interventions to optimise the mobile phone-based smoking cessation support: Study protocol for a sequential, multiple assignment, randomised trial (SMART). Trials, 23(1), 681.
Zhao, S. Z., Wu, Y. S., Chiu, S. L., Fong, D. Y. T., Lam, T. H., & Wang, M. P. (2021). Mobile chat-based support plus nicotine replacement therapy sampling to promote smoking cessation for community smokers: A pilot randomized controlled trial. Tobacco Induced Diseases, 19, 32.
Census & Statistics Department (Hong Kong SAR government). Thematic Household Survey, Report_No. 72: Pattern of Smoking. Hong Kong Census Stat Dep. 2019;(13):136.
Acknowledgements
The authors would like to thank the participants, helpers from the universities and non-governmental organizations and research assistants who involved in this study.
Funding
This study is funded by the Hong Kong Council on Smoking and Health. The funding body has no role in the design of the study and collection, analysis and interpretation, writing of the report or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
MPW, XW, SZZ and THL participated in study concept and design. MPW, XW and SZZ participated in conducting the study. SZZ drafted the manuscript. All authors provided critical comments, have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Ethical approval has been granted by the Institutional Review Board of the University of Hong Kong/ Hospital Authority Hong Kong West Cluster (IRB reference number: UW 19-403).
Consent for Publication
Not applicable
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhi, Z.S., Xue, W., Yongda, W. et al. Optimizing mHealth Instant Messaging-Based Smoking Cessation Support: A Sequential, Multiple Assignment, Randomized Trial (SMART). Int J Ment Health Addiction (2024). https://doi.org/10.1007/s11469-024-01328-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s11469-024-01328-7