Abstract
The present study aimed to assess the prevalence of psychological distress, associated lifestyle behaviors, and associated coping strategies among the students of healthcare profession. A total of 588 medical, dental, and nursing students studying in institutes of health sciences, KIIT University, Bhubaneswar, India participated in this cross-sectional online survey during September–October, 2020. A semi-structured questionnaire, DASS-21questionnaire, and Brief COPE were used to collect relevant information. The proportion of students experiencing symptoms of depression, anxiety, and stress was 26.2%, 27.7%, and 9.7%, respectively. Body mass index, presence of comorbidity, and soft drink consumption were significantly associated with psychological distress. Students experiencing psychological distress were applying emotion-focused coping behaviors (venting, acceptance, self-blame, substance use, religion) and avoidant coping behaviors (self-distraction, behavioral disengagement, denial). The prevalence of psychological distress among the students of health profession studying in KIIT University of Bhubaneswar during the period of Covid-19 pandemic is low and it can be further lowered by designing appropriate interventions incorporating healthy lifestyle behaviors and suitable coping strategies thereby ensuring sound mental health of these students.
Similar content being viewed by others
World Health Organization (WHO) declared Covid-19 as a public health emergency of international concern on 30th January 2020 and India reported its first confirmed case of coronavirus on the same day. The psychological issues accompanying the Covid-19 pandemic are emerging as serious public health concerns affecting not only individuals affected with Covid-19, but also healthy individuals (Duan & Zhu, 2020; Torales et al., 2020; Wang et al., 2020). Evidence shows that during outbreaks, university students and healthcare professionals have higher rates of psychological distress compared to the general population (Naser et al., 2020). Emotional disorders are common among the students of the health profession and need special attention (Filho et al., 2020; Lai et al., 2020; Moutinho et al., 2017). These students are vulnerable to develop depression, anxiety, and stress because of factors like structure of the medical curriculum, need to meet the academic requirement, frequent examinations, high-performance pressure, fear of failing, learning environment, lack of time for self-care, relationship with family and friends (Dyrbye & Shanafelt, 2016; Hakami et al., 2020; Weber et al., 2019).
In response to the Covid-19 pandemic, many countries including India introduced restriction measures such as social distancing, restriction of social gatherings, closure of educational institutions, limitation of population movement, self-isolation, etc. As a result, educational institutions across the world postponed or suspended all activities and shifted from classroom teaching to online learning format. The changes in the delivery of the medical curriculum might be expected to further worsen the academic stressors for students which may lead to reduced academic performance. In addition to teaching-related changes and loss of social connectedness, lifestyle behavior might negatively impact the students’ mental wellbeing and cause further psychological distress.
Therefore, there is a pressing need to assess and monitor the unprecedented mental health burden on the students of the health profession, alleviate the negative impacts, and provide the necessary support to them. There is a paucity of research that has addressed the mental health status of the students of the health profession especially in India during this pandemic. The present study aimed to assess the prevalence of psychological distress in terms of depression, anxiety, and stress among the students of the healthcare profession during the period of the Covid-19 pandemic, determine the associated lifestyle behaviors, and evaluate the coping strategies adopted by the students to tackle the situation.
Materials and Methods
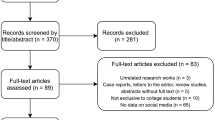
The present online cross-sectional survey was carried out during September–October, 2020 among the students of healthcare profession studying in the institutes of health sciences namely Kalinga Institute of Medical Sciences (KIMS), Kalinga Institute of Dental Sciences (KIDS), and Kalinga Institute of Nursing Sciences (KINS) of KIIT University, Bhubaneswar, India. Assuming the prevalence of psychological distress among the students of the health profession as 50%, 5% acceptable margin of error, and 95% confidence interval, the minimum sample size was estimated as 384. First, all the students were provided the protocol, information sheet, and consent form through e-mail. They were clarified about their doubts over phone/e-mail. Students suffering from acute severe illness, those suffering from Covid-19, or having family members infected/died with Covid-19 were excluded from the study. Privacy and confidentiality were maintained during data collection. A google form was created using a semi-structured questionnaire comprising 3 sections and sent to the eligible study participants through e-mail after obtaining their informed consent. Out of 728 students approached, 604 provided all relevant information by filling up the questionnaire. The study protocol was approved by the Institutional Ethics Committee of the author's institution (Ref. No: KIIT/KIMS/IEC/365/2020) and informed consent was sought from all the study participants before their inclusion in the study. The study has also been registered with Clinical Trial Registry-India (CTRI registration No: CTRI/2020/08/027492).
Section 1 contained socio-demographic characteristics such as age, gender, body mass index; lifestyle behaviors like fast food (pizza, burger, muffin, noodle, rolls, chips, etc.) consumption, soft drink (nonalcoholic sweetened carbonated beverages like soda, Pepsico, coca-cola, sprite, etc.) consumption, screen time (time spent on electronic devices including smartphones, laptops, tablets, TV, videogames), and exercise/yoga. Also, anthropometric parameters such as height and weight were recorded.
Section 2 included the DASS-21 questionnaire which was used to assess the mental health status of the students (Lovibond & Lovibond, 1995). The questionnaire has been validated in India as reported by previous studies (Sharma et al., 2020; Singh et al., 2015). It consists of 21 items categorized into 3 sub-scales namely depression, anxiety, and stress each containing 7 items. The depression scale assesses dissatisfaction, hopelessness, devaluation of life, self-depreciation, lack of energy, lack of interest, and inability to feel pleasure. The anxiety scale assesses dryness of mouth, breathing difficulty, trembling experience, situational anxiety, and subjective experience of anxious affect. The stress scale assesses difficulty relaxing, nervous arousal, and being agitated, overreaction to the situation, and intolerance. The respondents were required to indicate the presence of a symptom during the past week. The responses for each item is based on a 4-point Likert scale ranging from 0 (did not apply to me at all), 1 (applied to me to some degree, or some of the time), 2 (applied to me to a considerable degree or a good part of time) to 3 (applied to me very much or most of the time). Scores for depression, anxiety, and stress were calculated by summing the scores for the relevant items and categorized into normal, mild, moderate, severe, and extremely severe categories. Higher scores indicated a higher level of severity in each dimension.
In Sect. 3, Brief COPE questionnaire (Carver, 1997), validated in Indian population (Rani et al., 2016) was used to assess the coping strategies adopted by the respondents. It consists of 28 items categorized into 14 subscales, each with 2 items. Different specific coping behaviors including self-distraction, active coping, denial, use of instrumental support, substance use, use of emotional support, positive reframing, behavioral disengagement, venting, planning, humor, acceptance, religion, and self-blame were assessed. These subscales were then classified into 3 higher-order subscales (broad coping categories): Emotion-focused coping (substance use, use of emotional support, venting, positive reframing, humor, acceptance, religion, and self-blame), problem-focused coping (active coping, use of instrumental support and planning), and avoidant coping (distraction, denial, and behavioral disengagement). The response for each item is measured on a Likert scale from 1 (I haven’t been doing this at all), 2 (I’ve been doing this a little bit), 3 (I’ve been doing this a medium amount), to 4 (I’ve been doing this a lot).
All the data were cleaned and analyzed using SPSS version 21. Descriptive analysis of sociodemographic characteristics, psychological distress in terms of depression, anxiety, stress, any mental health condition i.e., one or more of the disorders, and coping strategies was performed. Data were expressed as percentage, means, standard deviations, 95% confidence intervals, and regression coefficients. Multivariate logistic regression (backward elimination approach) was conducted to develop the models identifying the most useful socio-demographic correlated and coping behaviors associated with the mental health outcomes. The variable with the highest p-value was removed from each subsequent model and the process was repeated until variables with p value < 0.05 were retained in the final model. The level of statistical significance was set at p < 0.05 for all the analyses. We tested multicollinearity among the independent variables which were not found in our data.
Results
In our study, 604 students responded by sending filled up questionnaires, out of which 16 were excluded because of the incompleteness of the data and thus 588 respondents were included in the final analysis. Table 1 outlines the distribution of sociodemographic characteristics of the respondents. The participants included 51.4% medical, 33.7% nursing, and 15% dental students. The mean age of the respondents was 20.9 ± 1.55 years and the majority (71.9%) of the respondents were females. More than half (54.5%) of the students were overweight or obese and more than one-fourth (27.9%) were not engaged in any kind of exercise/yoga. More than one-quarter of the students were spending screen time for ≥ 12 h per day. Out of 588 students, 24.5% and 16.7% were consuming fast food ≥ 3 times/week and soft drink > once a week respectively. Comorbidities like hypertension, diabetes, allergy, asthma, arthritis, dysmenorrhea, etc. were reported in 14.3% of the students.
The proportion of students with symptoms of depression, anxiety, and stress was 26.2%, 27.7%, and 9.7% respectively. Students were having mild (79, 13.4%), moderate (64, 10.9%), severe (11, 1.9%) levels of depression; mild (60, 10.2%), moderate (76, 12.9%), severe (27, 4.6%) levels of anxiety; mild (36, 6.1%) and moderate (21, 3.6%) levels of stress. More than one third (216, 36.7%) of the students reported symptoms suggestive of any mental health problem. Among the three types of psychological distress, the mean score of stress was the highest (6.9 ± 5.26), followed by depression (6.3 ± 5.52) and anxiety (5.2 ± 4.56). The three DASS-21 scales have shown good internal consistency (Cronbach’s α for depression, anxiety, and stress are 0.896, 0.823, and 0.879 respectively).
Table 2 shows the distribution of coping strategies based on Brief-COPE. Based on the mean scores, the most commonly reported coping strategies were acceptance, self-distraction, planning, active coping, positive reframing, emotional support, and instrumental support. The lowest mean scores were recorded for substance use, denial, and humor. Most of the students applied problem focussed strategies as the main coping mechanism compared to emotion focussed and avoidant coping strategies. The internal consistencies of the 14 two-item subscales in this sample ranged from 0.54 (venting) to 0.82 (substance use) with 11 of them with Chronbach’s α > 0.7. The 3 broad coping categories also showed good internal consistency (Chronbach’s α > 0.70).
Table 3 reveals the results of the regression models identifying the most useful sociodemographic factors associated with psychological distress. Factors like body mass index, and soft drink consumption were the important variables significantly associated with each of the outcome variable i.e., depression, anxiety, and stress. Presence of comorbidity was the other significant predictor of depression whereas age, presence of comorbidity, and screen time per day were also significantly associated with anxiety among the students.
Table 4 presents the results of regression models showing an association between the scores of coping strategies and psychological distress in male and female students. In male students, emotion-focused coping behaviors such as venting, acceptance, and self-blame were significantly associated with depression whereas avoidant coping behaviors like self-distraction, behavioral disengagement, and denial were associated with any of the psychological distress. Similarly, female respondents experiencing psychological distress applied emotion-focused coping behaviors (substance use, religion, self-blame) and avoidant coping behaviors (self-distraction, behavioral disengagement).
Discussion
The study findings showed that more than one-third of students of the health profession had experienced symptoms suggestive of any mental health problem i.e., one or more of the disorders. In our study, symptoms of depression, anxiety, and stress were observed in 30.8%, 27.2%, and 27.2% medical students respectively which are lower as compared to the results reported in a study which showed 64.4% and 46.2% of medical students experiencing moderate to severe symptoms of depression and anxiety respectively (Filho et al., 2020). In another study among Australian medical students, deterioration of mental wellbeing was reported in 68% of students since Covid-19 onset (Lyons et al., 2020). Hakami et al. in their study among dental students during the Covid-19 pandemic observed higher levels of depression (60.6%), anxiety (37.0%), and stress (34.9%) among dental students compared to our results (Hakami et al., 2020). The variation in the prevalence might be due to methodological and socio-cultural differences in different studies. The lower prevalence of psychological distress in our study might be attributed to the mentor–mentee program adopted by the faculties in KIIT University. It was reported in a study among nursing students conducted during the Covid-19 outbreak that 22.3%, 28.3%, and 6.5% of students had experienced depression, anxiety, and stress respectively which is similar to the findings of our study (Deo et al., 2020).
In our study, the overweight/obese students were more likely to have depression compared to students with a normal body mass index. This finding is in consistency with the results of previous literature which showed a significant positive association of overweight/obesity with increased risk of depression (Bjorngaard et al., 2015; Zhao et al., 2019). However, we observed that underweight students had higher odds of developing depression, anxiety, and stress as compared to students with a normal body mass index.
The odds of experiencing depression and anxiety increased in students having other comorbidities like hypertension, diabetes, asthma, arthritis, dysmenorrhea, etc. compared to healthy students. It is evident from previous research that anxiety and depression are significantly associated with these morbidities (Alkhathami et al., 2017; Bajalan et al., 2019; Fair et al., 2019; Gagua et al., 2013; Goodwin et al., 2012; Hamrah et al., 2018). Torun et al. in their study during the Covid-19 pandemic showed that the presence of chronic disease was more likely associated with increased anxiety in medical students (Torun & Torun, 2020). In the present study, students consuming soft drink frequently (> once/week) had higher odds of having psychological distress than those consuming soft drink ≤ once/week. Zhang et al. studied the association between soft drink and symptoms of anxiety and depression and observed that those frequently consuming soft drinks had significantly higher levels of anxiety and depression compared with those barely consuming soft drinks (Zhang et al., 2019). In another study conducted in Korean adolescents, it was reported that frequent energy drink (highly caffeinated soft drink) intake was significantly associated with stress and depressive mood (Park et al., 2016).
Our study revealed that students aged ≤ 20 years were 1.5 times more likely to have shown anxiety than their counterparts. Older students owing to their seniority and maturity might be able to handle the situation more effectively whereas newcomers and young students might face difficulty adjusting between the MBBS curriculum and the current situation. It was also observed that students with screen time ≥ 12 h per day had more anxiety than those with screen time < 6 h a day. This is supported by the results reported in previous literature (Boers et al., 2020; Twenge & Campbell, 2018).
The present study identified the coping strategies associated with psychological distress among male and female students separately. In consistency with our results, earlier studies have shown that young adults with mood disorders used significantly more maladaptive coping strategies (emotion-focused and avoidant coping) and less adaptive coping style like problem-focused coping strategy (Horwitz et al., 2011).
The coping behavior self-blame was significantly associated with depressive symptoms in both male and female students. Our result corroborates with the findings of previous research (Fear et al., 2009; Horwitz et al., 2011; Tilghman-Osborne et al., 2008). Substance use as a coping behavior was not significantly associated with any of the psychological distress except anxiety in female students. However, earlier studies have shown an association between adolescent alcohol use and depression (Galaif et al., 2007; Horwitz et al., 2011; Mason et al., 2008; Saxon et al., 2017). Similar to the results of an earlier study (Saxon et al., 2017), we also found religion as a coping behavior associated with a lower probability of having depression or any mental health condition in female students. Engaging in religious activities and receiving advice from religious groups are protective against poor mental health (Saxon et al., 2017; Seguin & Roberts, 2017; Sousa, 2013).
Active coping (taking active steps to remove the stressor or lessen its effects) was the only problem-focused coping strategy found to be protective against depression in male students. Other studies have also suggested that the use of active coping was supportive of mental health (Saxon et al., 2017; Seguin & Roberts, 2017). Other problem-focused coping behaviors such as planning and use of instrumental support were not inversely associated with any of the psychological distress in our study population. This might be explained by the fact that maladaptive behaviors had a stronger influence than adaptive strategies.
Avoidant coping strategies like self-distraction, behavioral disengagement, and denial showed significant associations with depression/anxiety/stress symptoms both in male and female students. Although these behaviors are somewhat controversial coping strategies but they can be considered useful in minimizing distress. Our results are supported by the findings of an earlier study (Saxon et al., 2017).
The study has a few limitations. Due to cross-sectional study design, only associations and no causal inferences can be made about the outcome. The online self-administered questionnaires may lead to reporting bias and social desirability bias resulting in under or over-reporting of the actual outcomes. The differences in mental health variables at different times could not be derived as we had no baseline data of the students before the Covid-19 pandemic. Also, the study included students studying in institutes belonged to a single university and thus the findings may not be generalized to students of health profession studying in other universities.
The prevalence of psychological distress among the students of health profession studying in KIIT University of Bhubaneswar during the period of Covid-19 pandemic is low. However, it is important to address students’ mental health concerns and provide appropriate support by delivering psychological interventions. Based on the results, the concerned institutional authorities need to design appropriate interventions incorporating healthy lifestyle behaviors and suitable coping strategies to ensure sound mental health for the students of the healthcare profession.
References
Alkhathami, A. D., Alamin, M. A., Alqahtani, A. M., Alsaeed, W. Y., Alkhathami, M. A., & Al-Dhafeeri, A. H. (2017). Depression and anxiety among hypertensive and diabetic primary health care patients: Could patients’ perception of their diseases control be used as a screening tool? Saudi Medical Journal, 38(6), 621–628.
Bajalan, Z., Moafi, F., MoradiBaglooei, M., & Alimoradi, Z. (2019). Mental health and primary dysmenorrhea: A systematic review. Journal of Psychosomatic Obstetrics and Gynecology, 40(3), 185–194. https://doi.org/10.1080/0167482X.2018.1470619
Bjorngaard, J. H., Carslake, D., Nilsen, T. I. L., Linthorst, A. C. E., Smith, G. D., Gunnell, D., & Romundstad, P. R. (2015). Association of body mass index with depression, anxiety and suicide—An instrumental variable analysis of the HUNT study. PLoS ONE, 10(7), e0131708. https://doi.org/10.1371/journal.pone.0131708
Boers, E., Afzali, M. H., & Conrod, P. (2020). Temporal associations of screen time and anxiety symptoms among adolescents. Canadian Journal of Psychiatry, 65(3), 206–208. https://doi.org/10.1177/0706743719885486
Carver, C. S. (1997). You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine, 4(1), 92–100. https://doi.org/10.1207/s15327558ijbm0401_6
Deo, P. K., Budhathoki, S., Raut, J., Adhikari, B., & Shrestha, J. (2020). Factors associated with perceived stress, anxiety, depression, insomnia during covid-19 outbreak among nursing students. International Journal of Science and Research, 9(9), 23–29.
Duan, L., & Zhu, G. (2020). Psychological interventions for people affected by the COVID-19 epidemic. The Lancet Psychiatry, 7(4), 300–302. https://doi.org/10.1016/S2215-0366(20)30073-0
Dyrbye, L., & Shanafelt, T. (2016). A narrative review on burnout experienced by medical students and residents. Medical Education, 50(1), 132–149. https://doi.org/10.1111/medu.12927
Fair, D. C., Rodriguez, M., Knight, A. M., & Rubinstein, T. B. (2019). Depression and anxiety in patients with juvenile idiopathic arthritis: Current insights and impact on quality of life, a systematic review. Open Access Rheumatology: Research and Reviews, 11, 237–252. https://doi.org/10.2147/OARRR.S174408
Fear, J. M., Champion, J. E., Reeslund, K. L., Forehand, R., Colletti, C., Roberts, L., & Compas, B. E. (2009). Parental depression and interparental conflict: Children and adolescents’ self-blame and coping responses. Journal of Family Psychology, 23(5), 762–766. https://doi.org/10.1037/a0016381
Filho, C. I. S., Rodrigues, W. C. de L. V., Castro, R. B. de, Marcal, A. A., Pavelqueires, S., Takano, L., Oliveira, W. L. de, Neto, C. I. S., Filho, C. I. S., Rodrigues, W. C. de L. V., Castro, R. B. de, Marcal, A. A., Pavelqueires, S., Takano, L., Oliveira, W. L. de, & Neto, C. I. S. (2020). Impact of Covid-19 pandemic on mental health of medical students: A cross-sectional study using GAD-7 and PHQ-9 Questionnaires Carlos. https://doi.org/10.1101/2020.06.24.20138925
Gagua, T., Tkeshelashvili, B., Gagua, D., & Mchedlishvili, N. (2013). Assessment of anxiety and depression in adolescents with primary dysmenorrhea: A case-control study. Journal of Pediatric and Adolescent Gynecology, 26(6), 350–354. https://doi.org/10.1016/j.jpag.2013.06.018
Galaif, E. R., Sussman, S., Newcomb, M. D., & Locke, T. F. (2007). Suicidality, depression, and alcohol use among adolescents: A review of empirical findings. International Journal of Adolescent Medicine and Health, 19(1), 27–35. https://doi.org/10.1515/IJAMH.2007.19.1.27
Goodwin, R. D., Bandiera, F. C., Steinberg, D., Ortega, A. N., & Feldman, J. M. (2012). Asthma and mental health among youth: Etiology, current knowledge and future directions. Expert Review of Respiratory Medicine, 6(4), 397–406. https://doi.org/10.1586/ers.12.34
Hakami, Z., Khanagar, S. B., Vishwanathaiah, S., Hakami, A., Bokhari, A. M., Jabali, A. H., Alasmari, D., & Aldrees, A. M. (2020). Psychological impact of the coronavirus disease 2019 (COVID-19) pandemic on dental students: A nationwide study. Journal of Dental Education. https://doi.org/10.1002/jdd.12470
Hamrah, M. S., Hamrah, M. H., Ishii, H., Suzuki, S., Hamrah, M. H., Hamrah, A. E., Dahi, A. E., Takeshita, K., Yisireyili, M., Hamrah, M. H., Fotouhi, A., Sakamoto, J., & Murohara, T. (2018). Anxiety and depression among hypertensive outpatients in Afghanistan: A cross-sectional study in Andkhoy City. International Journal of Hypertension. https://doi.org/10.1155/2018/8560835
Horwitz, A. G., Hill, R. M., & King, C. A. (2011). Specific coping behaviors in relation to adolescent depression and suicidal ideation. Journal of Adolescence, 34(5), 1077–1085. https://doi.org/10.1016/j.adolescence.2010.10.004
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., Wu, J., Du, H., Chen, T., Li, R., Tan, H., Kang, L., Yao, L., Huang, M., Wang, H., Wang, G., Liu, Z., & Hu, S. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976
Lovibond, S. H., & Lovibond, P. F. (1995). DASS-21. In Manual for the Depression Anxiety & Stress Scales (2nd ed.). Psychology Foundation.
Lyons, Z., Wilcox, H., Leung, L., & Dearsley, O. (2020). COVID-19 and the mental well-being of Australian medical students: Impact, concerns and coping strategies used. Australasian Psychiatry. https://doi.org/10.1177/1039856220947945
Mason, W. A., Kosterman, R., Haggerty, K. P., Hawkins, J. D., Redmond, C., Spoth, R. L., & Shin, C. (2008). Dimensions of adolescent alcohol involvement as predictors of young-adult major depression. Journal of Studies on Alcohol and Drugs, 69(2), 275–285.
Moutinho, I. L. D., Maddalena, D. C. P., & N., Roland, R. K., Lucchetti, A. L. G., TibiriçÁ, S. H. C., Da Silva Ezequiel, O., & Lucchetti, G. . (2017). Depression, stress and anxiety in medical students: A cross-sectional comparison between students from different semesters. Revista Da Associacao Medica Brasileira, 63(1), 21–28. https://doi.org/10.1590/1806-9282.63.01.21
Naser, A. Y., Dahmash, E. Z., Al-Rousan, R., Alwafi, H., Alrawashdeh, H. M., Ghoul, I., Abidine, A., Bokhary, M. A., & AL-Hadithi, H. T., Ali, D., Abuthawabeh, R., Abdelwahab, G. M., Alhartani, Y. J., Al Muhaisen, H., Dagash, A., & Alyami, H. S. . (2020). Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: A cross-sectional study. Brain and Behavior, 10(8), e01730. https://doi.org/10.1002/brb3.1730
Park, S., Lee, Y., & Lee, J. H. (2016). Association between energy drink intake, sleep, stress, and suicidality in Korean adolescents: Energy drink use in isolation or in combination with junk food consumption. Nutrition Journal. https://doi.org/10.1186/s12937-016-0204-7
Rani, M., Visalakshi, J., Shuba, K., Thenmozhi, M., Deepa, R., Katherine, R., & Lisa, E. (2016). Cultural adaptation of the brief COPE for persons living with. AIDS Behaviour, 19(2), 341–351. https://doi.org/10.1007/s10461-014-0872-2
Saxon, L., Makhashvili, N., Chikovani, I., Seguin, M., McKee, M., Patel, V., Bisson, J., & Roberts, B. (2017). Coping strategies and mental health outcomes of conflict-affected persons in the Republic of Georgia. Epidemiology and Psychiatric Sciences, 26(3), 276–286. https://doi.org/10.1017/S2045796016000019
Seguin, M., & Roberts, B. (2017). Coping strategies among conflict-affected adults in low- and middle-income countries: A systematic literature review. Global Public Health, 12(7), 811–829. https://doi.org/10.1080/17441692.2015.1107117
Sharma, M. K., Hallford, D. J., & Anand, N. (2020). Confirmatory factor analysis of the Depression, Anxiety, and Stress Scale among Indian adults. Indian Journal of Psychiatry, 62, 379–383. https://doi.org/10.4103/psychiatry.IndianJPsychiatry
Singh, K., Junnarkar, M., & Sharma, S. (2015). Anxiety, stress, depression, and psychosocial functioning of Indian adolescents. Indian J Psychiatry, 57(4), 367–374. https://doi.org/10.4103/0019-5545.171841
Sousa, C. A. (2013). Political violence, health, and coping among Palestinian women in the West Bank. American Journal of Orthopsychiatry, 83(4), 505–519. https://doi.org/10.1111/ajop.12048
Tilghman-Osborne, C., Cole, D. A., Felton, J. W., & Ciesla, J. A. (2008). Characterological self-blame to depressive symptoms in adolescents over time. Journal of Social and Clinical Psychology, 27(8), 809–842. https://doi.org/10.1521/jscp.2008.27.8.809
Torales, J., O’Higgins, M., Castaldelli-Maia, J. M., & Ventriglio, A. (2020). The outbreak of COVID-19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry, 66(4), 317–320. https://doi.org/10.1177/0020764020915212
Torun, F., & Torun, S. D. (2020). The psychological impact of the COVID-19 pandemic on medical students in Turkey. Pakistan Journal of Medical Sciences, 36(6), 1355–1359.
Twenge, J. M., & Campbell, W. K. (2018). Associations between screen time and lower psychological well-being among children and adolescents: Evidence from a population-based study. Preventive Medicine Reports, 12, 271–283. https://doi.org/10.1016/j.pmedr.2018.10.003
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (covid-19) epidemic among the general population in china. International Journal of Environmental Research and Public Health. https://doi.org/10.3390/ijerph17051729
Weber, J., Skodda, S., Muth, T., Angerer, P., & Loerbroks, A. (2019). Stressors and resources related to academic studies and improvements suggested by medical students: A qualitative study. BMC Medical Education. https://doi.org/10.1186/s12909-019-1747-z
Zhang, X., Huang, X., Xiao, Y., Jing, D., Huang, Y., Chen, L., Luo, D., Chen, X., & Shen, M. (2019). Daily intake of soft drinks is associated with symptoms of anxiety and depression in Chinese adolescents. Public Health Nutrition, 22(14), 2553–2560. https://doi.org/10.1017/S1368980019001009
Zhao, Z., Ding, N., Song, S., Liu, Y., & Wen, D. (2019). Association between depression and overweight in Chinese adolescents: A cross-sectional study. British Medical Journal Open, 9, e024177. https://doi.org/10.1136/bmjopen-2018-024177
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional Ethics Committee of Kalinga Institute of Medical Sciences (Ref. No: KIIT/KIMS/IEC/365/2020).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mishra, J., Samanta, P., Panigrahi, A. et al. Mental Health Status, Coping Strategies During Covid-19 Pandemic Among Undergraduate Students of Healthcare Profession. Int J Ment Health Addiction 21, 562–574 (2023). https://doi.org/10.1007/s11469-021-00611-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11469-021-00611-1