Abstract
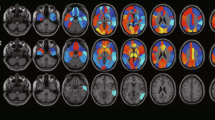
Exploring individual hallmarks of brain ageing is important. Here, we propose the age-related glucose metabolism pattern (ARGMP) as a potential index to characterize brain ageing in cognitively normal (CN) elderly people. We collected 18F-fluorodeoxyglucose (18F-FDG) PET brain images from two independent cohorts: the Alzheimer’s Disease Neuroimaging Initiative (ADNI, N = 127) and the Xuanwu Hospital of Capital Medical University, Beijing, China (N = 84). During follow-up (mean 80.60 months), 23 participants in the ADNI cohort converted to cognitive impairment. ARGMPs were identified using the scaled subprofile model/principal component analysis method, and cross-validations were conducted in both independent cohorts. A survival analysis was further conducted to calculate the predictive effect of conversion risk by using ARGMPs. The results showed that ARGMPs were characterized by hypometabolism with increasing age primarily in the bilateral medial superior frontal gyrus, anterior cingulate and paracingulate gyri, caudate nucleus, and left supplementary motor area and hypermetabolism in part of the left inferior cerebellum. The expression network scores of ARGMPs were significantly associated with chronological age (R = 0.808, p < 0.001), which was validated in both the ADNI and Xuanwu cohorts. Individuals with higher network scores exhibited a better predictive effect (HR: 0.30, 95% CI: 0.1340 ~ 0.6904, p = 0.0068). These findings indicate that ARGMPs derived from CN participants may represent a novel index for characterizing brain ageing and predicting high conversion risk into cognitive impairment.





Similar content being viewed by others
Availability of data and materials
All data are available upon request from the authors.
References
Fjell AM, McEvoy L, Holland D, Dale AM, Walhovd KB. What is normal in normal aging? Effects of aging, amyloid and Alzheimer’s disease on the cerebral cortex and the hippocampus. Prog Neurobiol. 2014;117:20–40.
Toepper M. Dissociating Normal Aging from Alzheimer’s Disease: A View from Cognitive Neuroscience. J Alzheimer’s Dis. 2017;57:331–52.
Mattson MP, Arumugam TV. Hallmarks of Brain Aging: Adaptive and Pathological Modification by Metabolic States. Cell Metab. 2018;27:1176–99.
Grimm A, Friedland K, Eckert A. Mitochondrial dysfunction: the missing link between aging and sporadic Alzheimer’s disease. Biogerontology. 2016;17:281–96.
Błaszczyk JW. Energy metabolism decline in the aging brain-pathogenesis of neurodegenerative disorders. Metabolites. 2020;10(11):450.
Cunnane S, Nugent S, Roy M, Courchesne-Loyer A, Croteau E, Tremblay S, et al. Brain fuel metabolism, aging, and Alzheimer’s disease. Nutrition. 2011;27:3–20.
Pardo JV, Lee JT, Sheikh SA, Surerus-Johnson C, Shah H, Munch KR, et al. Where the brain grows old: decline in anterior cingulate and medial prefrontal function with normal aging. Neuroimage. 2007;35:1231–7.
Bi Q, Wang W, Niu N, Li H, Wang Y, Huang W, et al. Relationship between the disrupted topological efficiency of the structural brain connectome and glucose hypometabolism in normal aging. Neuroimage. 2021;226: 117591.
Habeck C, Risacher S, Lee G, et al. Relationship between baseline brain metabolism measured using [18F]FDG PET and memory and executive function in prodromal and early Alzheimer’s disease. Brain Imaging Behav. 2012;6(4):568–83.
Chételat G, Landeau B, Salmon E, Yakushev I, Bahri MA, Mézenge F, et al. Relationships between brain metabolism decrease in normal aging and changes in structural and functional connectivity. Neuroimage. 2013;76:167–77.
Adams JN, Lockhart SN, Li L, Jagust WJ. Relationships Between Tau and Glucose Metabolism Reflect Alzheimer’s Disease Pathology in Cognitively Normal Older Adults. Cereb Cortex. 2019;29:1997–2009.
Inoue K, Ito H, Uchida S, Taki Y, Kinomura S, Tsuji I, et al. Decrease in glucose metabolism in frontal cortex associated with deterioration of microstructure of corpus callosum measured by diffusion tensor imaging in healthy elderly. Hum Brain Mapp. 2008;29:375–84.
Cole JH, Poudel RPK, Tsagkrasoulis D, Caan MWA, Steves C, Spector TD, et al. Predicting brain age with deep learning from raw imaging data results in a reliable and heritable biomarker. Neuroimage. 2017;163:115–24.
de Lange AG, Anatürk M, Suri S, Kaufmann T, Cole JH, Griffanti L, et al. Multimodal brain-age prediction and cardiovascular risk: The Whitehall II MRI sub-study. Neuroimage. 2020;222: 117292.
Beheshti I, Mishra S, Sone D, Khanna P, Matsuda H. T1-weighted MRI-driven Brain Age Estimation in Alzheimer’s Disease and Parkinson’s Disease. Aging Dis. 2020;11:618–28.
Bergfield KL, Hanson KD, Chen K, Teipel SJ, Hampel H, Rapoport SI, et al. Age-related networks of regional covariance in MRI gray matter: Reproducible multivariate patterns in healthy aging. Neuroimage. 2010;49:1750–9.
Li TR, Dong QY, Jiang XY, Kang GX, Li X, Xie YY, et al. Exploring brain glucose metabolic patterns in cognitively normal adults at risk of Alzheimer’s disease: A cross-validation study with Chinese and ADNI cohorts. Neuroimage Clin. 2022;33: 102900.
Spetsieris PG, Ma Y, Dhawan V, Eidelberg D. Differential diagnosis of parkinsonian syndromes using PCA-based functional imaging features. Neuroimage. 2009;45:1241–52.
Eidelberg D. Metabolic brain networks in neurodegenerative disorders: a functional imaging approach. Trends Neurosci. 2009;32:548–57.
Nan Z, Gordon ML, Yilong M, Bradley C, Gomar JJ, Shichun P, et al. The Age-Related Perfusion Pattern Measured With Arterial Spin Labeling MRI in Healthy Subjects. Front Aging Neurosci. 2018;10:214.
Teune LK, Strijkert F, Renken RJ, Izaks GJ, de Vries JJ, Segbers M, et al. The Alzheimer’s disease-related glucose metabolic brain pattern. Curr Alzheimer Res. 2014;11:725–32.
Wu T, Ma Y, Zheng Z, Peng S, Wu X, Eidelberg D, et al. Parkinson’s disease-related spatial covariance pattern identified with resting-state functional MRI. J Cereb Blood Flow Metab. 2015;35:1764–70.
Mudali D, Teune LK, Renken RJ, Leenders KL, Roerdink JB. Classification of Parkinsonian syndromes from FDG-PET brain data using decision trees with SSM/PCA features. Comput Math Methods Med. 2015;2015: 136921.
Chen K, Roontiva A, Thiyyagura P, Lee W, Liu X, Ayutyanont N, et al. Improved power for characterizing longitudinal amyloid-β PET changes and evaluating amyloid-modifying treatments with a cerebral white matter reference region. J Nucl Med. 2015;56:560.
Iizuka T, Kameyama M. Spatial metabolic profiles to discriminate dementia with Lewy bodies from Alzheimer disease. J Neurol. 2020;267:1960–9.
Habeck C, Foster NL, Perneczky R, Kurz A, Alexopoulos P, Koeppe RA, et al. Multivariate and univariate neuroimaging biomarkers of Alzheimer’s disease. Neuroimage. 2008;40:1503–15.
Jack CR Jr, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease. Alzheimer’s Dementia. 2018;14:535–62.
Wilson RS, Yu L, Lamar M, Schneider JA, Boyle PA, Bennett DA. Education and cognitive reserve in old age. Neurology. 2019;92:e1041–50.
Stern Y, Arenaza-Urquijo EM, Bartrés-Faz D, Belleville S, Cantilon M, Chetelat G, et al. Whitepaper: Defining and investigating cognitive reserve, brain reserve, and brain maintenance. Alzheimer’s Dementia. 2020;16:1305–11.
Pettigrew C, Soldan A, Zhu Y, Cai Q, Wang MC, Moghekar A, et al. Cognitive reserve and rate of change in Alzheimer’s and cerebrovascular disease biomarkers among cognitively normal individuals. Neurobiol Aging. 2020;88:33–41.
Sotoudeh N, Namavar MR, Zarifkar A, Heidarzadegan AR. Age-dependent changes in the medial prefrontal cortex and medial amygdala structure, and elevated plus-maze performance in the healthy male Wistar rats. IBRO Rep. 2020;9:183–94.
Bennett IJ, Rivera HG, Rypma B. Isolating age-group differences in working memory load-related neural activity: assessing the contribution of working memory capacity using a partial-trial fMRI method. Neuroimage. 2013;72:20–32.
Moeller JR, Ishikawa T, Dhawan V, Spetsieris P, Mandel F, Alexander GE, et al. The metabolic topography of normal aging. J Cereb Blood Flow Metab. 1996;16:385–98.
Liu D, Gu X, Zhu J, Zhang X, Han Z, Yan W, et al. Medial prefrontal activity during delay period contributes to learning of a working memory task. Science. 2014;346:458–63.
Günseli E, Aly M. Preparation for upcoming attentional states in the hippocampus and medial prefrontal cortex. Elife. 2020;9:e53191.
Kakimoto A, Ito S, Okada H, Nishizawa S, Minoshima S, Ouchi Y. Age-Related Sex-Specific Changes in Brain Metabolism and Morphology. J Nucl Med. 2016;57:221–5.
Rojkova K, Volle E, Urbanski M, Humbert F, Dell’Acqua F, Thiebaut de Schotten M. Atlasing the frontal lobe connections and their variability due to age and education: a spherical deconvolution tractography study. Brain Struct Funct. 2016;221:1751–66.
Salat DH, Buckner RL, Snyder AZ, Greve DN, Desikan RS, Busa E, et al. Thinning of the cerebral cortex in aging. Cereb Cortex. 2004;14:721–30.
Sullivan EV, Rohlfing T, Pfefferbaum A. Quantitative fiber tracking of lateral and interhemispheric white matter systems in normal aging: relations to timed performance. Neurobiol Aging. 2010;31:464–81.
Sakurai R, Fujiwara Y, Yasunaga M, Suzuki H, Kanosue K, Montero-Odasso M, et al. Association between Hypometabolism in the Supplementary Motor Area and Fear of Falling in Older Adults. Front Aging Neurosci. 2017;9:251.
Green PE, Ridding MC, Hill KD, Semmler JG, Drummond PD, Vallence AM. Supplementary motor area-primary motor cortex facilitation in younger but not older adults. Neurobiol Aging. 2018;64:85–91.
Sodums DJ, Bohbot VD. Negative correlation between grey matter in the hippocampus and caudate nucleus in healthy aging. Hippocampus. 2020;30:892–908.
Lithfous S, Dufour A, Després O. Spatial navigation in normal aging and the prodromal stage of Alzheimer’s disease: insights from imaging and behavioral studies. Ageing Res Rev. 2013;12:201–13.
Chen JJ, Rosas HD, Salat DH. Age-associated reductions in cerebral blood flow are independent from regional atrophy. Neuroimage. 2011;55:468–78.
Galiano A, Mengual E, García de Eulate R, Galdeano I, Vidorreta M, Recio M, et al. Coupling of cerebral blood flow and functional connectivity is decreased in healthy aging. Brain Imaging Behav. 2020;14:436–50.
An Y, Varma VR, Varma S, Casanova R, Dammer E, Pletnikova O, et al. Evidence for brain glucose dysregulation in Alzheimer’s disease. Alzheimer’s Dementia. 2018;14:318–29.
Chételat G, Arbizu J, Barthel H, Garibotto V, Law I, Morbelli S, et al. Amyloid-PET and (18)F-FDG-PET in the diagnostic investigation of Alzheimer’s disease and other dementias. Lancet Neurol. 2020;19:951–62.
Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dementia. 2011;7:280–92.
Scheltens P, De Strooper B, Kivipelto M, Holstege H, Chételat G, Teunissen CE, et al. Alzheimer’s disease. Lancet. 2021;397(10284):1577–90.
Guo T, Landau SM, Jagust WJ. Detecting earlier stages of amyloid deposition using PET in cognitively normal elderly adults. Neurology. 2020;94:e1512–24.
Vila-Castelar C, Tariot PN, Sink KM, Clayton D, Langbaum JB, Thomas RG, et al. Sex differences in cognitive resilience in preclinical autosomal-dominant Alzheimer’s disease carriers and non-carriers: Baseline findings from the API ADAD Colombia Trial. Alzheimer’s Dement. 2022;10.1002/alz.12552.
Buckley RF, Mormino EC, Rabin JS, Hohman TJ, Landau S, Hanseeuw BJ, et al. Sex Differences in the Association of Global Amyloid and Regional Tau Deposition Measured by Positron Emission Tomography in Clinically Normal Older Adults. JAMA Neurol. 2019;76:542–51.
Hohman TJ, Dumitrescu L, Barnes LL, Thambisetty M, Beecham G, Kunkle B, et al. Sex-Specific Association of Apolipoprotein E With Cerebrospinal Fluid Levels of Tau. JAMA Neurol. 2018;75:989–98.
Oveisgharan S, Arvanitakis Z, Yu L, Farfel J, Schneider JA, Bennett DA. Sex differences in Alzheimer’s disease and common neuropathologies of aging. Acta Neuropathol. 2018;136:887–900.
Acknowledgements
Data collection and dissemination for this project were funded by the Alzheimer’s Disease Neuroimaging Initiative (ADNI): the National Institutes of Health (grant number U01 AG024904), and the Department of Defense (award numberW81XWH-12-2-0012). ADNI is funded by the National Institute of Aging and the National Institute of Biomedical Imaging and Bioengineering as well as through generous contributions from the following organizations: AbbVie, Alzheimer’s Association, Alzheimer’s Drug Discovery Foundation, Araclon Biotech, BioClinica Inc., Biogen, Bristol-Myers Squibb Company, CereSpir Inc., Eisai Inc., Elan Pharmaceuticals Inc., Eli Lilly and Company, EuroImmun, F. Hoffmann-La Roche Ltd. and its affiliated company Genentech Inc., Fujirebio, GE Healthcare, IXICO Ltd., Janssen Alzheimer Immunotherapy Research & Development LLC., Johnson & Johnson Pharmaceutical Research &Development LLC., Lumosity, Lundbeck, Merck & Co. Inc., Meso Scale Diagnostics LLC., NeuroRx Research, Neurotrack Technologies, Novartis Pharmaceuticals Corporation, Pfizer Inc., Piramal Imaging, Servier, Takeda Pharmaceutical Company, and Transition Therapeutics. The Canadian Institutes of Health Research are providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Disease Cooperative Study at the University of California, San Diego, CA, USA. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California, CA, USA.
Michael W. Weiner7, Paul Aisen8, Ronald Petersen9, Clifford R. Jack9, William Jagust10, John Q. Trojanowski11, Arthur W. Toga12, Laurel Beckett13, Robert C. Green14, Andrew J. Saykin15, John Morris16, Leslie M. Shaw11, Zaven Khachaturian13,17, Greg Sorensen18, Lew Kuller19, Marcus Raichle16, Steven Paul20, Peter Davies21, Howard Fillit22, Franz Hefti23, David Holtzman16, Marek M. Mesulam24, William Potter25, Peter Snyder26, Adam Schwartz27, Tom Montine28, Ronald G. Thomas28, Michael Donohue28, Sarah Walter28, Devon Gessert28, Tamie Sather28, Gus Jiminez28, Danielle Harvey13, Matthew Bernstein9, Paul Thompson29, Norbert Schuff7,13, Bret Borowski9, Jeff Gunter9, Matt Senjem9, Prashanthi Vemuri9, David Jones9, Kejal Kantarci9, Chad Ward9, Robert A. Koeppe30, Norm Foster31, Eric M. Reiman32, Kewei Chen32, Chet Mathis19, Susan Landau10, Nigel J. Cairns16, Erin Householder16, Lisa Taylor-Reinwald16, Virginia Lee11, Magdalena Korecka11, Michal Figurski11, Karen Crawford12, Scott Neu12, Tatiana M. Foroud15, Steven G. Potkin33, Li Shen15, Kelley Faber15, Sungeun Kim15, Kwangsik Nho15, Leon Thal8, Neil Buckholtz34, Marylyn Albert35, Richard Frank36, John Hsiao34, Jeffrey Kaye37, Joseph Quinn37, Betty Lind37, Raina Carter37, Sara Dolen37, Lon S. Schneider12, Sonia Pawluczyk12, Mauricio Beccera12, Liberty Teodoro12, Bryan M. Spann12, James Brewer8, Helen Vanderswag8, Adam Fleisher8,32, Judith L. Heidebrink30, Joanne L. Lord30, Sara S. Mason9, Colleen S. Albers9, David Knopman9, Kris Johnson9, Rachelle S. Doody38, Javier Villanueva-Meyer38, Munir Chowdhury38, Susan Rountree38, Mimi Dang38, Yaakov Stern38, Lawrence S. Honig38, Karen L. Bell38, Beau Ances16, Maria Carroll16, Sue Leon16, Mark A. Mintun16, Stacy Schneider16, Angela Oliver16, Daniel Marson39, Randall Griffith39, David Clark39, David Geldmacher39, John Brockington39, Erik Roberson39, Hillel Grossman40, Effie Mitsis40, Leyla de Toledo-Morrell41, Raj C. Shah41, Ranjan Duara42, Daniel Varon42, Maria T. Greig42, Peggy Roberts42, Chiadi Onyike35, Daniel D’Agostino35, Stephanie Kielb35, James E. Galvin43, Brittany Cerbone43, Christina A. Michel43, Henry Rusinek43, Mony J. de Leon43, Lidia Glodzik43, Susan De Santi43, P Murali Doraiswamy44, Jeffrey R. Petrella44, Terence Z. Wong44, Steven E. Arnold11, Jason H. Karlawish11, David Wolk11, Charles D. Smith45, Greg Jicha45, Peter Hardy45, Partha Sinha45, Elizabeth Oates45, Gary Conrad45, Oscar L. Lopez19, MaryAnn Oakley19, Donna M. Simpson35, Anton P. Porsteinsson46, Bonnie S. Goldstein46, Kim Martin46, Kelly M. Makino46, M Saleem Ismail46, Connie Brand46, Ruth A. Mulnard33, Gaby Thai33, Catherine McAdams-Ortiz33, Kyle Womack47, Dana Mathews47, Mary Quiceno47, Ramon Diaz-Arrastia47, Richard King47, Myron Weiner47, Kristen Martin-Cook47, Michael DeVous47, Allan I Levey48, James J. Lah48, Janet S. Cellar48, Jeffrey M. Burns48, Heather S. Anderson49, Russell H. Swerdlow49, Liana Apostolova29, Kathleen Tingus29, Ellen Woo29, Daniel H.S. Silverman29, Po H. Lu29, George Bartzokis29, Neill R. Graff-Radford50, Francine Parfitt50, Tracy Kendall50, Heather Johnson50, Martin R. Farlow15, Ann Marie Hake15, Brandy R. Matthews15, Scott Herring15, Cynthia Hunt15, Christopher H. van Dyck51, Richard E. Carson51, Martha G. MacAvoy51, Howard Chertkow52, Howard Bergman52, Chris Hosein52, Ging-Yuek Robin Hsiung53, Howard Feldman53, Benita Mudge53, Michele Assaly53, Charles Bernick54, Donna Munic54, Andrew Kertesz55, John Rogers55, Dick Trost55, Diana Kerwin24, Kristine Lipowski24, Chuang-Kuo Wu24, Nancy Johnson24, Carl Sadowsky56, Walter Martinez56, Teresa Villena56, Raymond Scott Turner57, Kathleen Johnson57, Brigid Reynolds57, Reisa A. Sperling14, Keith A. Johnson14, Gad Marshall14, Meghan Frey14, Barton Lane14, Allyson Rosen14, Jared Tinklenberg14, Marwan N. Sabbagh58, Christine M. Belden58, Sandra A. Jacobson58, Sherye A. Sirrel58, Neil Kowall58, Ronald Killiany59, Andrew E. Budson59, Alexander Norbash59, Patricia Lynn Johnson59, Joanne Allard59, Alan Lerner61, Paula Ogrocki61, Leon Hudson61, Evan Fletcher13, Owen Carmichae23, John Olichney13, Charles DeCarli13, Smita Kittur62, Michael Borrie63, T-Y. Lee63, Rob Bartha63, Sterling Johnson64, Sanjay Asthana64, Cynthia M. Carlsson64, Adrian Preda29, Dana Nguyen29, Pierre Tariot31, Stephanie Reeder31, Vernice Bates65, Horacio Capote65, Michelle Rainka65, Douglas W. Scharre66, Maria Kataki66, Anahita Adeli66, Earl A. Zimmerman67, Dzintra Celmins67, Alice D. Brown67, Godfrey D. Pearlson68, Karen Blank68, Karen Anderson68, Robert B. Santulli69, Tamar J. Kitzmiller69, Eben S. Schwartz69, Kaycee M. Sink70, Jeff D. Williamson70, Pradeep Garg70, Franklin Watkins70, Brian R. Ott71, Henry Querfurth71, Geoffrey Tremont71, Stephen Salloway72, Paul Malloy72, Stephen Correia72, Howard J. Rosen7, Bruce L. Miller7, Jacobo Mintzer73, Kenneth Spicer73, David Bachman73, Stephen Pasternak55, Irina Rachinsky55, Dick Drost55, Nunzio Pomara74, Raymundo Hernando74, Antero Sarrael74, Susan K. Schultz75, Laura L. Boles Ponto75, Hyungsub Shim75, Karen Elizabeth Smith75, Norman Relkin20, Gloria Chaing20, Lisa Raudin17,20, Amanda Smith76, Kristin Fargher76, Balebail Ashok Raj76, Thomas Neylan7, Jordan Grafman24, Melissa Davis8, Rosemary Morrison8, Jacqueline Hayes7, Shannon Finley7, Karl Friedl77, Debra Fleischman41, Konstantinos Arfanakis41, Olga James44, Dino Massoglia73, J Jay Fruehling64, Sandra Harding64, Elaine R. Peskind28, Eric C. Petrie66, Gail Li66, Jerome A. Yesavage78, Joy L. Taylor78 & Ansgar J. Furst78
7UC San Francisco, San Francisco, CA 94143, USA. 8UC San Diego, San Diego, CA 92093, USA. 9Mayo Clinic, Rochester, NY 14603, USA. 10UC Berkeley, Berkeley, CA 94720, USA. 11UPenn, Philadelphia, PA 9104, USA. 12USC, Los Angeles, CA 90089, USA. 13UC Davis, Davis, CA 95616, USA. 14Brigham and Women’s Hospital/Harvard Medical School, Boston, MA 02115, USA. 15Indiana University, Bloomington, IN 47405, USA. 16Washington University in St Louis, St Louis, MI 63130, USA. 17Prevent Alzheimer’s Disease 2020, Rockville, MD 20850, USA. 18Siemens, Munich 80333, Germany. 19University of Pittsburgh, Pittsburgh, PA 15260, USA. 20Weill Cornell Medical College, Cornell University, New York City, NY 10065, USA. 21Albert Einstein College of Medicine of Yeshiva University, Bronx, NY 10461, USA. 22AD Drug Discovery Foundation, New York City, NY 10019, USA. 23Acumen Pharmaceuticals, Livermore, CA 94551, USA. 24Northwestern University, Evanston and Chicago, IL 60208, USA. 25National Institute of Mental Health, Rockville, MD 20852, USA. 26Brown University, Providence, RI 02912, USA. 27Eli Lilly, Indianapolis, IN 46225, USA. 28University of Washington, Seattle, WA 98195, USA. 29UCLA, Los Angeles, CA 90095, USA. 30University of Michigan, Ann Arbor, MI 48109, USA. 31University of Utah, Salt Lake City, UT 84112, USA. 32Banner Alzheimer’s Institute, Phoenix, AZ 85006, USA. 33UC Irvine, Irvine, CA 92697, USA. 34National Institute on Aging, Bethesda, MD 20892, USA. 35Johns Hopkins University, Baltimore, MD 21218, USA. 36Richard Frank Consulting, Washington, DC 20001, USA. 37Oregon Health and Science University, Portland, OR 97239, USA. 38Baylor College of Medicine, Houston, TX 77030, USA. 39University of Alabama, Birmingham, AL 35233, USA. 40Mount Sinai School of Medicine, New York City, NY 10029, USA. 41Rush University Medical Center, Chicago, IL 60612, USA. 42Wien Center, Miami, FL 33140, USA. 43New York University, New York City, NY 10003, USA. 44Duke University Medical Center, Durham, NC 27710, USA. 45University of Kentucky, Lexington, KY 0506, USA. 46University of Rochester Medical Center, Rochester, NY 14642, USA. 47University of Texas Southwestern Medical School, Dallas, TX 75390, USA. 48Emory University, Atlanta, GA 30322, USA. 49Medical Center, University of Kansas, Kansas City, KS 66103, USA. 50Mayo Clinic, Jacksonville, FL 32224, USA. 51Yale University School of Medicine, New Haven, CT 06510, USA. 52McGill University/Montreal-Jewish General Hospital, Montreal, QC H3T 1E2, Canada. 53University of British Columbia Clinic for AD & Related Disorders, Vancouver, BC V6T 1Z3, Canada. 54Cleveland Clinic Lou Ruvo Center for Brain Health, Las Vegas, NV 89106, USA. 55St Joseph’s Health Care, London, ON N6A 4V2, Canada. 56Premiere Research Institute, Palm Beach Neurology, Miami, FL 33407, USA. 57Georgetown University Medical Center, Washington, DC 20007, USA. 58Banner Sun Health Research Institute, Sun City, AZ 85351, USA. 59Boston University, Boston, MA 02215, USA. 60Howard University, Washington, DC 20059, USA. 61Case Western Reserve University, Cleveland, OH 20002, USA. 62Neurological Care of CNY, Liverpool, NY 13088, USA. 63Parkwood Hospital, London, ON N6C 0A7, Canada. 64University of Wisconsin, Madison, WI 53706, USA. 65Dent Neurologic Institute, Amherst, NY 14226, USA. 66Ohio State University, Columbus, OH 43210, USA. 67Albany Medical College, Albany, NY 12208, USA. 68Hartford Hospital, Olin Neuropsychiatry Research Center, Hartford, CT 06114, USA. 69Dartmouth- Hitchcock Medical Center, Lebanon, NH 03766, USA. 70Wake Forest University Health Sciences, Winston-Salem, NC 27157, USA. 71Rhode Island Hospital, Providence, RI 02903, USA. 72Butler Hospital, Providence, RI 02906, USA. 73Medical University South Carolina, Charleston, SC 29425, USA. 74Nathan Kline Institute, Orangeburg, NY 10962, USA. 75University of Iowa College of Medicine, Iowa City, IA 52242, USA. 76University of South Florida: USF Health Byrd Alzheimer’s Institute, Tampa, FL 33613, USA. 77Department of Defense, Arlington, VA 22350, USA. 78Stanford University, Stanford, CA 94305, USA
Funding
This study was supported by grants received from the National Natural Science Foundation of China (grant numbers 61633018, 82020108013, 61603236, 81830059, and 81801052); the National Key Research and Development Program of China (grant numbers 2016YFC1306300, 2018YFC1312000, and 2018YFC1707704); the 111 Project (grant number D20031); the Shanghai Municipal Science and Technology Major Project (grant number 2017SHZDZX01); and the Beijing Municipal Commission of Health and Family Planning (grant number PXM2020_026283_000002).
Author information
Authors and Affiliations
Consortia
Contributions
JJ and YH conceived of the study. CL and XJ performed the statistical analysis. CS, GC, SJ drafted the initial manuscript. XJ and LL drew the pictures. All authors contributed to revision and editing of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Jiang, J., Sheng, C., Chen, G. et al. Glucose metabolism patterns: A potential index to characterize brain ageing and predict high conversion risk into cognitive impairment. GeroScience 44, 2319–2336 (2022). https://doi.org/10.1007/s11357-022-00588-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-022-00588-2