Abstract
Air pollution can cause disease and has become a major global environmental problem. It is currently believed that air pollution may be related to the progression of SSNHL. As a rapidly developing city in recent years, Hefei has serious air pollution. In order to explore the correlation between meteorological variables and SSNHL admissions, we conducted this study. This study investigated the short-term associations between SSNHL patients admitted to the hospital and Hefei climatic variables. The daily data on SSNHL-related hospital admissions and meteorological variables containing mean temperature (T-mean; °C), diurnal temperature range (DTR; °C), atmospheric pressure (AP; Hp), and relative humidity (RH; %), from 2014 to 2021 (2558 days), were collected. A time-series analysis integrating distributed lag non-linear models and generalized linear models was used. PubMed, Embase, Cochrane Library, and Web of Science databases were searched. Literature published up to August 2023 was reviewed to explore the potential impact mechanisms of meteorological factors on SSNHL. The mechanisms were determined in detail, focusing on wind speed, air pressure, temperature, humidity, and air pollutants. Using a median of 50.00% as a baseline, the effect of exceedingly low T-mean in the single-day hysteresis effect model began at a lag of 8 days (RR = 1.032, 95% CI: 1.001 ~ 1.064). High DTR affected the admission rate for SSNHL on lag 0 day. The significance of the effect was the greatest on that day (RR = 1.054, 95% CI: 1.007 ~ 1.104) and then gradually decreased. High and exceedingly high RH affected the admission rate SSNHL on lag 0 day, and these effects lasted for 8 and 7 days, respectively. There were significant associations between all grades of AP and SSNHL. This is the first study to assess the effect of meteorological variables on SSNHL-related admissions in China using a time-series approach. Long-term exposures to high DTR, RH values, low T-mean values, and all AP grades enhance the incidence of SSNHL in residents. Limiting exposure to extremes of ambient temperature and humidity may reduce the number of SSNHL-related hospital visits in the region. It is advisable to maintain a suitable living environment temperature and avoid extreme temperature fluctuations and high humidity. During periods of high air pollution, it is recommended to stay indoors and refrain from outdoor exercise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sudden sensorineural hearing loss (SSNHL) is defined as a hearing loss of at least 30 dB affecting three or more consecutive frequencies over 3 days for unknown reasons. It is commonly, but not always, accompanied by tinnitus and/or vertigo. Every year, five to 27 per 100,000 persons are affected by SSNHL, and approximately 66,000 new cases occur in the “”United States (Chandrasekhar et al. 2019). In China, the estimated annual incidence of SSNHL was 19 per 100,000 people (Chandrasekhar et al. 2019; Xie et al. 2020). Population studies of sudden sensorineural hearing loss have shown the occurrence of this condition in a broad age range with an average age of 50–60 years and no sex preference. The hearing loss is unilateral, with fewer than 5% of instances reporting bilateral involvement (Oh et al. 2007). The categories of hearing loss severity include mild, moderate, and severe-profound hearing loss (Nieman and Oh 2020). The hearing loss might impact high, low, or all frequencies depending on how it is configured (Moore 2016). Approximately 80% of patients have tinnitus, and about 30% experience vertigo, which is indicative of a related peripheral vestibular dysfunction (Nosrati-Zarenoe et al. 2007). The sense of having a plugged or numb ear is another typical ailment. Up to 80% of patients report a feeling of ear fullness (Sakata and Kato 2006). SSNHL may appear as a standalone issue, as a systemic disease’s presenting symptom, or during an established diagnosis. The complex etiology of SSNHL is still unknown, although risk factors for SSNHL include viral infection, environmental or occupational factors (such as loud noises, heavy metals, and organic solvents), autoimmune diseases, cardiovascular diseases, accidental events, endothelial dysfunction, metabolic diseases, and health habits (such as smoking and alcohol consumption) (Aimoni et al. 2010; Chau et al. 2010; Ciorba et al. 2010; Levy and Amedee 2010; Capaccio et al. 2012; Choi and Kim 2014; Quaranta et al. 2016; Umesawa et al. 2017; Chen et al. 2019; Jeong et al. 2019).
During the past 10 years, air pollution has emerged as a significant environmental problem, in both developing and developed nations. Population density, automobile emissions, agriculture, industrial emissions, power plants, and fossil fuel burning have strong positive relationships with air pollutant levels (Liu et al. 2016; Gu et al. 2019). In recent years, mounting research has suggested that several environmental variables may operate as potential risk factors for the development of SSNHL (Lee et al. 2019b; Zhang et al. 2021b; Tsai et al. 2021). Additionally, a preliminary report has indicated a seasonal pattern of SSNHL episodes. The results showed that the incidence of SSNHL was lowest in winter and highest in spring (Simani et al. 2022). However, no study has been conducted using advanced statistical models to systematically quantify and assess the influence of meteorological variables containing the temperature mean (T-mean), diurnal temperature range (DTR), atmospheric pressure (AP), relative humidity (RH), and wind speed on SSNHL, despite the previously clarified role of ambient temperature in SSNHL. To further explore the relationship between climatic conditions and SSNHL, it is very important to carry out such a systematic quantification and evaluation since it may increase our knowledge of how environmental variables affect SSNHL and provide ideas for enhancing public health.
In order to explore the correlation between meteorological variables and SSNHL admissions, we conducted a time-series analysis to further investigate if these connections varied among subpopulations (groups defined by sex, age, and position of hospital admission). In addition, we collated the previous relevant literature to deeply investigate the possible effects and mechanisms of meteorological factors on SSNHL from several aspects: wind speed, air pressure, temperature, humidity, and air pollutants. This is the first study to comprehensively measure and assess the effect of meteorological variables such as MT, DTR, AP, and RH on SSNHL-related admissions in China using a time-series approach.
Materials and methods
Basic information and overview of the study site
Hefei, the capital city of Anhui Province, is situated in East China within central Anhui Province (31°52′N, 117°17′E). Hefei experiences a modest annual rainfall of approximately 1000 mm, with prevailing southeasterly winds in spring and summer and northwesterly winds in autumn and winter. The city maintains an annual average temperature of 15.7 °C, with lower temperatures in winter and higher temperatures and humidity in summer due to a thicker inversion layer and slower air flow. These conditions reflect the typical subtropical monsoon climate of eastern China (Chen et al. 2023) (Fig. 1). According to the 2021 census data, Hefei has a population of 9,369,881, a built-up area of 528.5 km2, an urbanization rate (urban population/total population) of 82.28%, and a gross domestic product of 100.4572 billion renminbi (RMB) (China APBoSo. 21 May 2021 edn: https://zwgk.hefei.gov.cn/public/14891/106487817.html, 2019). By selecting Hefei as the focus of this study, the meteorological characteristics of cities in eastern China are accurately represented, allowing for a universal and representative correlation between meteorological variables and SSNHL.
Besides, in recent years, China has experienced rapid economic growth and accelerated urbanization, leading to a significant increase in man-made pollution issues. The Yangtze River Delta region, being the most economically developed coastal special economic zone in China, faces dense cities and highly concentrated air pollution emissions, showcasing distinct regional air pollution characteristics. This area is among the most air-polluted and densely populated regions in China (Feng et al. 2006). Hefei, as a representative city in the Yangtze River Delta region, is situated amidst the heavily polluted areas of Beijing-Tianjin-Hebei, Fenwei Plain, and the Yangtze River Delta to the north, west, and east respectively, resulting in severe cross-regional pollution. The primary pollutants contributing to air pollution in Hefei are fine particulate matter (PM2.5) and inhalable particulate matter (PM10), which could potentially impact sudden sensorineural hearing loss (SSNHL). This study not only investigates the correlation between meteorological factors and SSNHL but also delves into the connection between air pollutants and SSNHL in Hefei. Such research can offer a deeper insight into the link between air pollution and disease progression in the Yangtze River Delta region and beyond, serving as a valuable resource for clinical and air quality management practices.
Source and collection of data
The Department of Head and Neck Surgery at the First Affiliated Hospital of Anhui Medical University and the Second Affiliated Hospital of Anhui Medical University, two of the city’s largest public head and neck surgery clinics preferred by local patients with head and neck surgery diseases, provided daily data on hospital admissions (including first admissions and readmissions) for SSNHL in Hefei from 2014 to 2021 (2,558 days). Demographic factors such as age, sex, home address, date of hospital admission, and status of hospital admission were used in the data collection for SSNHL (i.e., first admission or readmission). Hospital admissions records for patients whose demographic details (including sex and age) were not identified or whose residence locations were not in Hefei City were excluded to render the obtained data legitimate and trustworthy. The Ethical Committee of the Anhui Medical University authorized the current research, which was carried out following the Ethical Principles for Medical Research from the Declaration of Helsinki (20,131,220).
The meteorological data were collected from the Hefei Meteorological Bureau and the air pollutant data from Hefei Environmental Monitoring Center. Air pollutant data from Hefei Environmental Monitoring Center contained the daily 8-h highest ozone concentration (O3), particulate matter (PM2.5), carbonic oxide (CO), inhalable particles (PM10), nitrogen dioxide (NO2), and sulfur dioxide (SO2). Meteorological data from Hefei Meteorological Bureau contained RH, daily average temperature, AP, wind speed, daily maximum temperature, and daily minimum temperature, where daily maximum and minimum temperatures were used to calculate the daily average temperature difference.
Statistical analysis
Categorical variables were presented as numbers (%). Continuous variables with a normal distribution were expressed as means (standard deviations, SD) and otherwise as medians (interquartile ranges, IQR). In addition, we removed the strongly correlated variables using the Spearman correlation test, and two variables were considered to be strongly correlated when the test result was greater than 0.7 (Shao et al. 2021). Given that environmental exposures are complex and variable, their effects on human health are often non-linear. And the flexibility of generalized additive models is widely used due to their ability to deal well with non-linear points in the environment (Ma et al. 2014; Li et al. 2022), given that the daily number of hospitalizations for SSNHL in this study is a small probability event and follows a quasi-Poisson distribution. Consistent with previous studies (Gasparrini 2014), we used a quasi-Poisson generalized additive model combined with distributed nonlinear lag model (DLNM) to explore the relationship between the admission rate for SSNHL and the climate. The time series model of meteorological factors (MF) was as follows:
where \({\mu }_{t}\) represents the number of daily hospitalizations for SSNHL; \(\alpha\) means the intercept distance; \({MF}_{t,l}\) is the 0 ~ l day lag matrix of MF, β corresponds to the vector coefficients of MF matrix; ns denotes natural cubic spline function; Pollutant represents O3, PM10, SO2, NO2, and CO; a natural cubic spline with 8 degrees of freedom per year was used to adjust for seasonality and long-term trend. The effect of weekends and holidays was controlled for by including “DOW” and “Holiday” in the models, respectively.
The evaluation of the degree of fit and freedom of these two models was done with the Akaike information criterion and residual analysis. Based on the incubation period for SSNHL, we reviewed similar literature and determined the lag days as 2 weeks (14 days). We used RR and its 95% CI to depict cumulative and single-day risk results for the admission rate for SSNHL. Finally, the 50th percentile of MF was used as a reference to classify MF into four categories: exceedingly high (95th), high (75th), low (25th), and exceedingly low (5th).
Software usage
The map of Hefei City, Anhui Province, China, was obtained from the software of ArcMap Desktop (10.7.0.10450 version). Descriptive analyses were performed using SPSS 23.0 and the remaining statistical analyses using R software (version 4.1.2). The matching of meteorological models in time series was implemented with “spline” and “DLNM” packages. The criteria for determining bilateral statistical differences were based on a “”p value < 0.05.
Literature review
Two researchers independently searched the Cochrane Database, EMBASE, PubMed, and Web of Science. It was searched using a combination of Medical Subject Heading terms (MeSH), free-text search terms, and Boolean operators. They collected the relevant literature focused on the potential impact mechanisms of meteorological factors on SSNHL until August 2023. The search terms included sudden sensorineural hearing loss, wind speed, air pressure, temperature, humidity, and air pollutants.
The inclusion criteria are research studies that delineated the potential impact mechanisms of meteorological factors on SSNHL. The exclusion criteria are (1) reports of individual cases, evaluations, remarks, and summaries presented at conferences, commentaries, and letters without unique data and (2) data that could not be entirely extracted.
Results
Descriptive summary
The distribution of the daily number of patients with SSNHL, major pollutants, and MFs in Hefei, China, 2014–2021, is shown in Table 1. We identified a total of 4984 patients with SSNHL over a period of 2558 days, with an average of 1.43 patients with SSNHL per day. Among all patients with SSNHL, there were 1871 instances (51.02%) in men, 1796 (48.98%) in women, 3158 (86.15%) in the 0–65 year age group, and 508 (13.85%) in the ≥ 65 years age group. Among them, the ratio of male to female was about 1:1, and the ratio of young individuals (aged 0–65 years) to older (aged ≥ 65 years) was about 7:1. The T-mean, DTR, RH, AP, and wind speed were 17.40 °C (range: − 5.90 to 35.60 °C), 8.70 (range: 0.60–22.10 °C), 78.00% (range: 33.00–100%), 1012.10 hPA (range: 987.50–1041.00 hPA), and 1.90 m/s (range: 0.30–6.60 m/s), respectively. The average concentrations of the air pollutants PM2.5, PM10, SO2, NO2, CO, and O3 were 44.00 μg/m3 (PM2.5, range: 5.00–351.00 μg/m3), 74.00 μg/m3 (PM10, range: 11.00–413.00 μg/m3), 10.00 μg/m3 (SO2, range: 2.00–58.00 μg/m3), 36.00 μg/m3 (NO2, range: 9.00–134.00 μg/m3), 800.00 μg/m3 (CO, range: 320.00–2860.00 μg/m3), and 52.00 μg/m3 (O3, range: 4.00–185.00 μg/m3), respectively. Supplementary Fig. 1 presented the temporal trends of meteorological variables and SSNHL outpatient visits in Hefei City during the study period.
Correlation analysis
The outcomes of the Spearman correlation analysis of air pollutants and MF are shown in Fig. 2A. There were positive correlations between PM2.5 and PM10 (P < 0.001, rs = 0.826), and between PM2.5 and CO (P < 0.001, rs = 0.835). The T-mean and AP were negatively associated with NO2, PM2.5, SO2, PM10, and CO and positively associated with O3 (all P < 0.001). The DTR was positively associated with NO2, PM2.5, SO2, O3, PM10, and CO (all P < 0.001). However, RH was negatively associated with NO2, PM2.5, SO2, PM10, CO, and O3 (all P < 0.001).
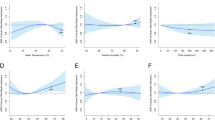
A Spearman’s correlation coefficients for meteorological factors and atmospheric pollutants. B A three-dimensional plot of the relative risk of daily SSNHL vs. T-mean, diurnal temperature range, relative humidity, and atmospheric pressure. C The overall exposure–response association with SSNHL. SSNHL, sudden sensorineural hearing loss
The overall effect of T-mean, DTR, RH, and AP on the admission rate for SSNHL
The exposure–response relationships of the T-mean, DTR, RH, and AP at different values with the admission rate for SSNHL are shown in Fig. 2B, C. We found a monotonically increasing trend between DTR and SSNHL hospitalization risk. Specifically, the risk of hospitalization in SSNHL increased with increasing DTR values. We also observed that low levels of AP were not associated with the risk of SSNHL admission, but after AP reached a certain level, AP values were positively associated with the risk of SSNHL admission. The association between the T-mean and the admission rate for SSNHL is shown in Table 2. In the single-day lag, with a median of 50.00% as the reference, extremely low temperature increased the risk of SSNHL admission from lag8 (RR = 1.032, 95% CI: 1.001–1.064) to lag14 (RR = 1.095, 95% CI: 1.03, 1.163), and lag14 had the highest RR. Table 3 records the relationship between DTR and the admission rate for SSNHL. Except for high and exceedingly high DTR, no significant effect was found for the DTR of other grades. Overall, extremely high DTR affected the admission rate for SSNHL on lag 0 day. The significance of the effect was greatest on that day (RR = 1.054, 95% CI: 1.007–1.104) and then gradually decreased. The cumulative risk curve showed a gradual increase in the cumulative risk. In terms of the high RH, the single-day lag association was statistically significant from lag0 to lag7 with the highest RR of SSNHL admission being at lag0 (RR = 1.029, 95%CI: 1.008, 1.050). In the cumulative lag structure, estimated risk effects appeared to be significant from lag0 to lag 0–14. Similar results were observed for the association between extremely high RH and the risk of SSNHL admission (Table 4). Interestingly, all grades of AP had significant effects on SSNHL (Table 5). The effects of low grades AP were delayed, whereas the effects of high grades AP were immediate.
Stratified analysis by age and sex
Figure 3 shows the stratified analysis results of the “”T-mean according to age and sex. Both hypothermia and hyperthermia had significant effects on SSNHL. At very low DTR, men were affected, and the effect appeared on day 4 of the delay and lasted for 7 days. Both men and women were affected by extremely high DTR, and the effects on women were immediate, whereas men showed significant effects only after a delay of 5 days (Fig. 4). At very low RH, men and women as well as the elderly and non-elderly were affected. At extremely high RH, all but the older individuals were affected (Fig. 5). Among older individuals and men, SSNHL was almost unaffected by AP. However, under different AP levels, non-elderly women were affected, and the effects were delayed and sustained to different degrees (Fig. 6).
Literature review
Using the originally set search terms, we further read the full text after reviewing the titles, abstracts, and eliminating duplicates, resulting in the inclusion of 15 literatures (Herbert et al. 1987; Preyer 1996; Danielides et al. 2002; Lin et al. 2006; Li and Feng 2013; Seo et al. 2014; Yun et al. 2014; Ryu et al. 2017; Lee et al. 2019a; Choi et al. 2019; Zhang et al. 2019b; Tsai et al. 2021; Zhang et al. 2021a; Tang et al. 2022; Cheng et al. 2022). We deeply investigate the possible effects and mechanisms of meteorological factors on SSNHL from several aspects: wind speed, air pressure, temperature, humidity, and air pollutants (Table 6). Database and search strategy are shown in Supplement Table 1.
Discussion
Hippocrates proposed that meteorological changes could affect human health in the fifth century (Nastos and Matzarakis 2006). And the impact of meteorological factors on acute gouty arthritis (Park et al. 2017), rheumatoid arthritis (Azzouzi and Ichchou 2020), systemic lupus erythematosus, and Behcet’s disease (Lee et al. 2015) has now been demonstrated. As a common emergency in otorhinolaryngology, the etiology of SSNHL is not clear. Now, although there are many studies reporting the seasonal and meteorological effects on the incidence, severity, and prognosis of SSNHL, controversy remains. So, we collated the previous relevant literature to deeply investigate the possible effects and mechanisms of meteorological factors on SSNHL from several aspects: wind speed, air pressure, temperature, humidity, and air pollutants. In addition, a time-series analysis integrating distributed lag non-linear models and generalized linear models was used in order to investigate the short-term associations between SSNHL patients admitted to the hospital and Hefei climatic variables.
Wind speed and atmospheric pressure
Recent viral infection is known to be associated with SSNHL. Several possible mechanisms have been proposed to explain how viral infections lead to SSNHL. The first may be that viral invasion of the cochlear nerve and spiral ganglia through the bloodstream or other routes induces SSNHL (Merchant et al. 2008); the second is that under certain conditions, viral reactivation in inner ear tissues initiates the inner ear’s immune response system, activating multiple inflammatory factors, causing endotheliosis and cytokine activation, which can lead to macrothrombi in the inner ear; the third is that viral infection triggers antigenic cross-reactivity in the inner ear, damaging the inner ear (Wilson 1986). Seo et al. reported that SSNHL incidence was significantly associated with mean wind speed and maximum wind speed when investigating the association between meteorological factors and SSNHL (Seo et al. 2014). Lee (Lee et al. 2019a) and Yun’s (Yun et al. 2014) findings also supported this view, which may be because strong winds increase the spread of the virus and enhance viral susceptibility (Fig. 7). Moreover, viral reactivation is based on decreased immune activity, which can be triggered by metabolic changes, physiological stressors, co-infections, cold, psychological stressors, and immunosuppressive states. So strong wind may induce the reactivation of neurotropic virus in spiral ganglion by decreasing immune activity and increase the risk of SSNHL (Seo et al. 2014). It has already been reported that higher wind speed may cause idiopathic facial paralysis and vestibular neuritis, and its etiology is similar to that of SSNHL, supporting the association between wind speed and the pathogenesis of SSNHL (Jeon et al. 2013).
Potential mechanisms for linkage of wind speed and SSNHL. Strong wind speed can trigger SSNHL from three pathways: enhanced viral transmission, inflammatory immune response, and cross-reactivity. Enhanced viral transmission: In the case of strong wind speed, the virus can invade the spiral ganglion through respiratory transmission and blood transmission, infect the cochlear nerve, and cause hearing damage; inflammatory immune response: strong wind speed can cause elevated levels of IL-6 and TNF and promote the activation and differentiation of CD4T cells, CD8T cells, and B cells, thereby triggering inflammatory responses; cross-reactivity: strong wind speed can trigger cross-reactions and promote IgM production, which binds virus antigens and accidentally binds inner ear antigens and damaging the inner ear. SSNHL, sudden sensorineural hearing loss; IL-6, interleukin 6; TNF, tumor necrosis factor; NF-κB, nuclear factor kappa-B; SIP, steroid receptor coactivator, SRC, SRC-interacting protein; IgM, ImmunoglobulinM; Th17, T helper cell 17; CTL, cytotoxic T lymphocyte; CD4 + , cluster of differentiation 4 plus; CD8 + cluster of differentiation 8 plus
An increase in tympanic membrane tension, which, in turn, results from a variance between middle ear pressure and AP, is thought to be the origin of a feeling of ear fullness in normal ears (Sakata et al. 2009). Comprehensive focus is drawn to the processes behind the feeling of ear fullness in acute sensorineural hearing loss, including Meniere’s disease, acute low-tone sensorineural hearing loss, abrupt deafness, and additional hearing-related illnesses. According to Sakata et al. (2012), there was a noticeable disparity in the minimum sensory threshold for air pressure with negative pressure between the affected and unaffected side of SSNHL patients, suggesting AP to be a key factor in the onset of SSNHL. Herbert suggests that SSNHL is more likely to occur at low pressure, especially when the pressure difference is large (Herbert et al. 1987), which is also supported by Preyer (1996). And he compared patients with complete recovery of hearing thresholds with those who had not yet recovered hearing and found that the former had smaller differences in air pressure and air temperature changes. We hypothesized that this may be due to the lower partial pressure of oxygen during hypobaric pressure, which leads to impaired microcirculation in the inner ear by affecting the production of reactive oxygen species (ROS) and related pathways (Fig. 8) (Alde et al. 2023). In addition, hyperbaric oxygen treatment is considered a salvage therapy to treat SSNHL, which indicates the effect of AP on SSNHL. However, there is no consensus on the relationship between air pressure and SSNHL, and further verification and discussion are still needed.
Potential mechanisms for linkage of atmospheric pressure and SSNHL. Under the conditions of low air pressure, the partial pressure of oxygen decreases, and hypoxia-induced ROS. ROS depresses levels of NO, induces monocyte invasion, elevates lipid peroxidation, promotes phenotype switching of VSMCs, induces EC dysfunction, precipitates inflammation as well as alters vascular responses and vasotone, which can cause vascular endothelial damage on the one hand, and on the other hand, it can promote Ca2+ inward flow, consume ATP, inhibit the guanylate cycle, reduce cGMP production, and cause vascular smooth muscle spasm, resulting in microcirculation disorders in the inner ear. SSNHL, sudden sensorineural hearing loss; ROS, reactive oxygen species; ATP, adenosine triphosphate; cGMP, cyclic guanosine monophosphate; O2, oxygen; NO, nitrogen; GTP, guanosine triphosphate; PKG, protein kinase G
In contrast to previous studies, our results indicate that all grades of AP have a significant effect on SSNHL. The effects of low grades AP were delayed, whereas the effects of high grades AP were immediate. Besides, we found that AP affected only young women, but not the rest of the population. Given the lack of relevant research in this context, we conjecture that estrogen might play an important role and explain the differences between individuals with and without sensitivity to AP.
Temperature and humidity
The current study with a time-series analysis examined whether the subpopulation-specific (stratified by sex, age, and status of hospital admission) correlations between MF such as T-mean, DTR, AP, and RH, and hospital outpatients for SSNHL varied over the short term and were non-linear and lag-related. We discovered that there was an enhanced positive correlation between DTR and SSNHL risk. This implies that vascular factors may contribute to the development of this subtype of SSNHL. At present, many studies have confirmed the association between cerebrovascular disease and SSNHL. Lin et al. (2008) found that patients with SSNHL had a significantly higher risk of stroke within 5 years than controls, and stroke patients also had a significantly higher probability of developing SSNHL than non-stroke patients (Kuo et al. 2016). For cerebrovascular disease, acute attack of cerebrovascular disease is closely related to temperature, and rapid changes in environmental temperature will dramatically increase the risk of stroke (Lavados et al. 2018; Mohammad et al. 2018). This suggests that ambient temperature may cause the onset of SSNHL.
There are many studies about the relation between temperature and SSNHL and suggest that the effect of temperature changes on SSNHL is similar to the mechanism by which temperature changes affect cerebrovascular disease (Lee et al. 2019b; Zhang et al. 2021b). The blood supply of the cochlea is supplied by the labyrinthine artery, which lacks collateral circulation. When endothelial injury, hypercoagulability, or blood stasis occurs, the cochlear microcirculation may be damaged, resulting in edema, ischemia, and hypoxia of the inner ear tissue, and thus hearing damage (Capaccio et al. 2007). Large temperature difference can activate the function of autonomic nerve, enhance the excitability of sympathetic nerve of inner ear, and increase sympathetic excitability of the inner ear. At the same time, it can cause vasospasm, increase platelet count, increase blood viscosity in the inner ear, and even lead to vascular embolism or thrombosis, resulting in microcirculatory disorders in the inner ear and causing SSNHL under the influence of body fluid (Lavados et al. 2018). Zhang et al. have found that the characteristics of temperature changes at onset in patients with full-frequency descending SSNHL were similar to those at onset of ischemic stroke, which further supported the pathogenesis discussed earlier: temperature may affect the inner ear microcirculation (Zhang et al. 2019a). Additionally, the temperature variation may function as a catalyst for the disruption of microcirculation in the inner ear. SSNHL was more easily induced by high DTR to low DTR. The sympathetic nervous system and the renin-angiotensin system are triggered when the body’s ability to adjust to a temperature shift is exceeded (Du et al. 2021). This increased secretion of sweat causes the increase of blood viscosity and slow blood stasis, which affects the inner ear microcirculation leading to the pathogenesis (Fig. 9).
Potential mechanisms for linkage of temperature and SSNHL. Under high temperatures or large temperature differences, on the one hand, norepinephrine is elevated, which promotes vascular smooth muscle contraction by binding to α1 receptors. Changes in blood flow within the inner ear lead to microcirculatory disorders, causing ischemia, decreased blood oxygen levels, and edema in local tissue cells of the inner ear. This ultimately results in damage to the nerves of the inner ear; on the other hand, high-temperature conditions cause microcirculatory disorders in the inner ear due to the diastole of erector spinae muscles and blood vessels, the increased secretion of sweat, and the increased viscosity of blood, which lead to microcirculatory disorders and damage of the inner ear. SSNHL, sudden sensorineural hearing loss; ATP, adenosine triphosphate; NE, noradrenaline
Our study also supports the findings of previous studies that high temperatures increase the incidence of SSNHL. Besides, we also found that low DTR may reduce the onset of SSNHL in men. Further research into this phenomenon is required to conclude the potential relationship between DTR and SSNHL.
Up to now, there are few studies on the humidity and SSNHL. In our study, RH affected practically all groups. The audiogram configuration of SSNHL can be categorized into five distinct patterns: ascending, descending, flat, profound, and others (Mattox and Simmons 1977). According to a prior study, when RH levels were high, individuals were most likely to be ascending patterns. Our results also support this opinion. However, different patterns were proved to be associated with various pathogenetic mechanisms (Kuhn et al. 2011). According to a prior study, individuals with ascending patterns had RH levels that were noticeably higher on the day of commencement (Zhang et al. 2021b). Therefore, we speculate that the large effect of RH may be related to end lymphatic hydrops, although further confirmation is needed.
Air pollution
Industrial production increases the health and economic burden caused by air pollution (Bai et al. 2018). Air pollutants include many kinds: NO2, NO, CO, PM2.5, etc. Several studies suggest that air pollution could induce SSNHL by many ways including toxic effects, oxidative stress, and inflammatory pathways (Choi et al. 2019; Lee et al. 2019a; Tsai et al. 2021; Cheng et al. 2022; Tang et al. 2022). The possible specific mechanisms of this may be as follows: oxidative stress is dysregulated after inhalation of air pollutants, resulting in increased reactive oxygen species (ROS), which destroys endothelial cells, affects inner ear microcirculation, and induces SSNHL (Lehner et al. 2011); when exposed to air pollution, inflammatory cytokine expression is increased, causing an inflammatory response, thereby increasing susceptibility to infection (Hesterberg et al. 2009) (Fig. 10); in addition, air pollutants are associated with increased cardiovascular morbidity (Dehbi et al. 2017). Combined with the above association of SSNHL with cardiovascular disease, it can also be speculated that air pollution may have an impact on SSNHL. And air pollutants may also interact with each other, for example, NO2 can affect the concentration of NO in the cochlea, and NO, as a signaling molecule between the cochlear space and blood vessels, can lead to changes in cochlear neurotransmission and neuroregulation, which leads to hearing impairment (Heinrich and Helling 2012).
Potential mechanisms for linkage of air pollution and SSNHL. Air pollutants damage inner ear epithelial cells by inducing ROS and inflammatory responses, resulting in inner ear microcirculation disorders. ROS: when the concentration of air pollutants is high, ROS will be induced to increase. ROS depresses levels of NO, induces monocyte invasion, elevates lipid peroxidation, promotes phenotype switching of VSMCs, induces EC dysfunction, precipitates inflammation, and alters vascular responses and vasotone, which can cause vascular endothelial damage on the one hand, and on the other hand, it can promote Ca2+ inward flow, consume ATP, inhibit the guanylate cycle, reduce cGMP production, and cause vascular smooth muscle spasm, resulting in microcirculation disorders in the inner ear. Inflammatory immune response: Air pollutants can cause elevated levels of IL-6 and TNF and promote the activation and differentiation of CD4T cells, CD8T cells, and B cells, thereby triggering inflammatory responses. SSNHL, sudden sensorineural hearing loss; ROS, reactive oxygen species; ATP, adenosine triphosphate; cGMP, cyclic guanosine monophosphate; O2, oxygen; NO, nitrogen; GTP, guanosine triphosphate; PKG, protein kinase G; IL-6, interleukin 6; TNF, tumor necrosis factor; NF-κB, nuclear factor kappa-B; SIP, steroid receptor coactivator, Th17, T helper cell 17; CTL, cytotoxic T lymphocyte; CD4 + , cluster of differentiation 4 plus; CD8 + cluster of differentiation 8 plus
Based on the results of previous studies, we analyzed the correlation between air pollutants and MF. The results showed that the T-mean and AP were negatively associated with NO2, PM2.5, SO2, PM10, and CO and positively associated with O3. The DTR was positively associated with NO2, PM2.5, SO2, O3, PM10, and CO. However, RH was negatively associated with NO2, PM2.5, SO2, PM10, CO, and O3.
Limitation and advantage
It is important to note that the present study has some limitations. First, the lack of specific information on the participants’ time spent outside, which can indicate their true degree of exposure to meteorological factors, may result in exposure measurement inaccuracies. Second, since there is a dearth of detailed information, certain possible confounding variables, such as socioeconomic position and family history, could not be adjusted. Finally, since the statistics used in this study were solely from one single city, care should be used when extrapolating the findings of our research to other areas with different climates. More epidemiological studies founded on larger-scale regions and different populations, together with mechanism findings, are urgently required to understand the specific processes responsible for the connections between meteorological variables and SSNHL onset.
Despite these limitations, our study has several advantages. Currently, there are few studies reporting the correlation between meteorological factors and SSNHL. This may be because: (1) SSNHL may appear as a standalone issue, as a systemic disease’s presenting symptom, or during an established diagnosis, which makes it difficult to diagnose, and there are few related reports. As a common disease among the elderly, hearing loss has become a serious public health problem as aging intensifies (Jiang et al. 2023). To the best of our knowledge, this is the first study to comprehensively measure and assess the effect of meteorological variables such as MT, DTR, AP, and RH on SSNHL-related admissions in China using a time-series approach. Additionally, the subgroup analysis was further conducted based on sex, age, and status of admission to identify possible vulnerable individuals and obtain a much more accurate estimation of the influence of MF on hospital admission for SSNHL. Additional epidemiological data confirming the effects of meteorological variables on SSNHL could be discovered in our current investigation. Our current investigation discussed the effects of meteorological variables, such as AP, DTR, RH, and T-mean on SSNHL based on additional epidemiological data. Finally, we collated the previous relevant literature to deeply investigate the possible effects and mechanisms of meteorological factors on SSNHL from several aspects: wind speed, air pressure, temperature, humidity, and air pollutants. Based on the results of this study, it is advisable to maintain a suitable living environment temperature and avoid extreme temperature fluctuations and high humidity. During periods of high air pollution, it is recommended to stay indoors and refrain from outdoor exercise. Individuals with underlying conditions like high blood pressure should focus on a balanced diet, and regular exercise and monitor environmental factors such as temperature, humidity, air quality, and air pressure, taking necessary precautions when needed.
Conclusion
This is the first study to comprehensively measure and assess the effect of meteorological variables such as MT, DTR, AP, and RH on SSNHL-related admissions in China using a time-series approach. Our study concludes that exposure to high DTR and RH values, low T-mean values, and all AP grades might increase hospital admissions for SSNHL in areas with humid subtropical monsoon climates, particularly for the first admission. Interestingly, whereas women are vulnerable to all grades of AP exposure, men appear to be more sensitive to low DTR exposure, although older individuals tend to be more sensitive to high RH exposure. Therefore, it is advisable to avoid extreme temperature fluctuations and high humidity. During periods of high air pollution, it is recommended to stay indoors and refrain from outdoor exercise. Individuals with underlying conditions like high blood pressure should focus on a balanced diet, regular exercise, and monitor environmental factors such as temperature, humidity, air quality, and air pressure, taking necessary precautions when needed.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Change history
08 July 2024
A Correction to this paper has been published: https://doi.org/10.1007/s11356-024-34299-2
References
Aimoni C, Bianchini C, Borin M, Ciorba A, Fellin R, Martini A et al (2010) Diabetes, cardiovascular risk factors and idiopathic sudden sensorineural hearing loss: a case-control study. Audiol Neurootol 15(2):111–115. https://doi.org/10.1159/000231636
Alde M, Cantarella G, Piatti G, Ambrosetti U (2023) Sudden hearing loss and early hyperbaric oxygen therapy: a preliminary study. Undersea Hyperb Med 50(2):145–153. https://doi.org/10.22462/01.00.2023.18
Azzouzi H, Ichchou L (2020) Seasonal and weather effects on rheumatoid arthritis: myth or reality? Pain Res Manag 2020:5763080. https://doi.org/10.1155/2020/5763080
Bai R, Lam JCK, Li VOK (2018) A review on health cost accounting of air pollution in China. Environ Int 120:279–294. https://doi.org/10.1016/j.envint.2018.08.001
Capaccio P, Ottaviani F, Cuccarini V, Bottero A, Schindler A, Cesana BM et al (2007) Genetic and acquired prothrombotic risk factors and sudden hearing loss. Laryngoscope 117(3):547–551. https://doi.org/10.1097/MLG.0b013e31802f3c6a
Capaccio P, Pignataro L, Gaini LM, Sigismund PE, Novembrino C, De Giuseppe R et al (2012) Unbalanced oxidative status in idiopathic sudden sensorineural hearing loss. Eur Arch Otorhinolaryngol 269(2):449–453. https://doi.org/10.1007/s00405-011-1671-2
Chandrasekhar SS, Tsai Do BS, Schwartz SR, Bontempo LJ, Faucett EA, Finestone SA et al (2019) Clinical practice guideline: sudden hearing loss (update). Otolaryngol Head Neck Surg 161(1_suppl):S1–S45. https://doi.org/10.1177/0194599819859885
Chau JK, Lin JR, Atashband S, Irvine RA, Westerberg BD (2010) Systematic review of the evidence for the etiology of adult sudden sensorineural hearing loss. Laryngoscope 120(5):1011–1021. https://doi.org/10.1002/lary.20873
Chen X, Fu YY, Zhang TY (2019) Role of viral infection in sudden hearing loss. J Int Med Res 47(7):2865–2872. https://doi.org/10.1177/0300060519847860
Chen C, He YS, Tao SS, Fang Y, Zhang RD, Fang X et al (2023) Climate change and daily outpatient visits for dermatomyositis in Hefei, China: a time-series study. Environ Sci Pollut Res Int 30(45):101053–101063. https://doi.org/10.1007/s11356-023-29542-1
Cheng C-G, Chen Y-H, Yen S-Y, Lin H-C, Lin H-C, Chou K-R et al (2022) Air pollution exposure and the relative risk of sudden sensorineural hearing loss in Taipei. Int J Environ Res Public Health 19(10):6144. https://doi.org/10.3390/ijerph19106144
Choi YH, Kim K (2014) Noise-induced hearing loss in Korean workers: co-exposure to organic solvents and heavy metals in nationwide industries. PLoS One 9(5):e97538. https://doi.org/10.1371/journal.pone.0097538
Choi HG, Min C, Kim SY (2019) Air pollution increases the risk of SSNHL: a nested case-control study using meteorological data and national sample cohort data. Sci Rep 9(1):8270. https://doi.org/10.1038/s41598-019-44618-0
Ciorba A, Bovo R, Castiglione A, Pirodda A, Martini A (2010) Sudden bilateral sensorineural hearing loss as an unusual consequence of accidental ingestion of potassium hydroxide. Med Princ Pract 19(5):406–408. https://doi.org/10.1159/000316382
Danielides V, Nousia C-S, Bartzokas A, Lolis CJ, Kateri M, Skevas A (2002) Weather conditions and sudden sensorineural hearing loss. BMC Ear Nose Throat Disord 2(1):2–2. https://doi.org/10.1186/1472-6815-2-2
Dehbi HM, Blangiardo M, Gulliver J, Fecht D, de Hoogh K, Al-Kanaani Z et al (2017) Air pollution and cardiovascular mortality with over 25years follow-up: a combined analysis of two British cohorts. Environ Int 99:275–281. https://doi.org/10.1016/j.envint.2016.12.004
Du J, He Z, Xu M, Qu X, Cui J, Zhang S et al (2021) Brown adipose tissue rescues bone loss induced by cold exposure. Front Endocrinol (lausanne) 12:778019. https://doi.org/10.3389/fendo.2021.778019
Feng J, Chan CK, Fang M, Hu M, He L, Tang X (2006) Characteristics of organic matter in PM2.5 in Shanghai. Chemosphere 64(8):1393–1400. https://doi.org/10.1016/j.chemosphere.2005.12.026
Gasparrini A (2014) Modeling exposure-lag-response associations with distributed lag non-linear models. Stat Med 33(5):881–899. https://doi.org/10.1002/sim.5963
Gu Y, Li Q, Wei D, Gao L, Tan L, Su G et al (2019) Emission characteristics of 99 NMVOCs in different seasonal days and the relationship with air quality parameters in Beijing, China. Ecotoxicol Environ Saf 169:797–806. https://doi.org/10.1016/j.ecoenv.2018.11.091
Heinrich UR, Helling K (2012) Nitric oxide–a versatile key player in cochlear function and hearing disorders. Nitric Oxide 27(2):106–116. https://doi.org/10.1016/j.niox.2012.05.005
Herbert I, Nolte E, Eichhorn T (1987) [Weather status and incidence of idiopathic facial nerve paralyses, vestibular disorders, Meniere’s attacks and sudden deafness] [English Abstract Journal Article]. Laryngol Rhinol Otol 66(5):249–250. https://doi.org/10.1055/s-2007-998647
Hesterberg TW, Bunn WB, McClellan RO, Hamade AK, Long CM, Valberg PA (2009) Critical review of the human data on short-term nitrogen dioxide (NO2) exposures: evidence for NO2 no-effect levels. Crit Rev Toxicol 39(9):743–781. https://doi.org/10.3109/10408440903294945
Jeon EJ, Park YS, Kim DH, Nam IC, Park SY, Noh H et al (2013) Effects of meteorological factors on the onset of Bell’s palsy. Auris Nasus Larynx 40(4):361–365. https://doi.org/10.1016/j.anl.2012.10.008
Jeong J, Lim H, Lee K, Hong CE, Choi HS (2019) High risk of sudden sensorineural hearing loss in several autoimmune diseases according to a population-based national sample cohort study. Audiol Neurootol 24(5):224–230. https://doi.org/10.1159/000502677
Jiang CY, Han K, Yang F, Yin SY, Zhang L, Liang BY et al (2023) Global, regional, and national prevalence of hearing loss from 1990 to 2019: a trend and health inequality analyses based on the Global Burden of Disease Study 2019. Ageing Res Rev 92:102124. https://doi.org/10.1016/j.arr.2023.102124
Kuhn M, Heman-Ackah SE, Shaikh JA, Roehm PC (2011) Sudden sensorineural hearing loss: a review of diagnosis, treatment, and prognosis. Trends Amplif 15(3):91–105. https://doi.org/10.1177/1084713811408349
Kuo CL, Shiao AS, Wang SJ, Chang WP, Lin YY (2016) Risk of sudden sensorineural hearing loss in stroke patients: a 5-year nationwide investigation of 44,460 patients. Medicine (baltimore) 95(36):e4841. https://doi.org/10.1097/MD.0000000000004841
Lavados PM, Olavarria VV, Hoffmeister L (2018) Ambient temperature and stroke risk: evidence supporting a short-term effect at a population level from acute environmental exposures. Stroke 49(1):255–261. https://doi.org/10.1161/STROKEAHA.117.017838
Lee JH, Cheon JH, Hong SP, Kim TI, Kim WH (2015) Seasonal variation in flares of intestinal Behcet’s disease. Dig Dis Sci 60(11):3373–3378. https://doi.org/10.1007/s10620-015-3863-x
Lee HM, Kim MS, Kim DJ, Uhm TW, Yi SB, Han JH et al (2019a) Effects of meteorological factor and air pollution on sudden sensorineural hearing loss using the health claims data in Busan, Republic of Korea. Am J Otolaryngol - Head Neck Med Surg 40(3):393–399. https://doi.org/10.1016/j.amjoto.2019.02.010
Lee HM, Kim MS, Kim DJ, Uhm TW, Yi SB, Han JH et al (2019b) Effects of meteorological factor and air pollution on sudden sensorineural hearing loss using the health claims data in Busan, Republic of Korea. Am J Otolaryngol 40(3):393–399. https://doi.org/10.1016/j.amjoto.2019.02.010
Lehner C, Gehwolf R, Tempfer H, Krizbai I, Hennig B, Bauer HC et al (2011) Oxidative stress and blood-brain barrier dysfunction under particular consideration of matrix metalloproteinases. Antioxid Redox Signal 15(5):1305–1323. https://doi.org/10.1089/ars.2011.3923
Levy JM, Amedee RG (2010) In reference to systematic review of the evidence for the etiology of adult sudden sensorineural hearing loss. Laryngoscope 120(11):2347. https://doi.org/10.1002/lary.21213
Li Y, Wu J, Hao J, Dou Q, Xiang H, Liu S (2022) Short-term impact of ambient temperature on the incidence of influenza in Wuhan, China. Environ Sci Pollut Res Int 29(12):18116–18125. https://doi.org/10.1007/s11356-021-16948-y
Li K, Feng W (2013) [Influence of both solar activity and the global warming on the variation trend of occurrence of sudden deafness]. Lin chuang er bi yan hou tou jing wai ke za zhi = Journal of clinical otorhinolaryngology, head, and neck surgery 27(16):894–898. https://www.embase.com/search/results?subaction=viewrecord&id=L603397589&from=export. Accessed 24 Aug 2023
Lin H-C, Lee H-C, Chao P-Z, Wu C-S (2006) The effects of weather on the incidence of sudden sensorineural hearing loss: a 5-year population-based study. Audiol Neuro-otology 11(3):165–171. https://doi.org/10.1159/000091268
Lin HC, Chao PZ, Lee HC (2008) Sudden sensorineural hearing loss increases the risk of stroke: a 5-year follow-up study. Stroke 39(10):2744–2748. https://doi.org/10.1161/STROKEAHA.108.519090
Liu J, Mauzerall DL, Chen Q, Zhang Q, Song Y, Peng W et al (2016) Air pollutant emissions from Chinese households: a major and underappreciated ambient pollution source. Proc Natl Acad Sci U S A 113(28):7756–7761. https://doi.org/10.1073/pnas.1604537113
Ma WP, Gu S, Wang Y, Zhang XJ, Wang AR, Zhao NQ et al (2014) The use of mixed generalized additive modeling to assess the effect of temperature on the usage of emergency electrocardiography examination among the elderly in Shanghai. PLoS One 9(6):e100284. https://doi.org/10.1371/journal.pone.0100284
Mattox DE, Simmons FB (1977) Natural history of sudden sensorineural hearing loss. Ann Otol Rhinol Laryngol 86(4 Pt 1):463–480. https://doi.org/10.1177/000348947708600406
Merchant SN, Durand ML, Adams JC (2008) Sudden deafness: is it viral? ORL J Otorhinolaryngol Relat Spec 70(1):52–60. https://doi.org/10.1159/000111048. (discussion 60-52)
Mohammad MA, Koul S, Rylance R, Frobert O, Alfredsson J, Sahlen A et al (2018) Association of weather with day-to-day incidence of myocardial infarction: a SWEDEHEART Nationwide Observational Study. JAMA Cardiol 3(11):1081–1089. https://doi.org/10.1001/jamacardio.2018.3466
Moore BC (2016) A review of the perceptual effects of hearing loss for frequencies above 3 kHz. Int J Audiol 55(12):707–714. https://doi.org/10.1080/14992027.2016.1204565
Nastos PT, Matzarakis A (2006) Weather impacts on respiratory infections in Athens. Greece Int J Biometeorol 50(6):358–369. https://doi.org/10.1007/s00484-006-0031-1
Nieman CL, Oh ES (2020) Hearing Loss. Ann Intern Med 173(11):ITC81–ITC96. https://doi.org/10.7326/AITC202012010
Nosrati-Zarenoe R, Arlinger S, Hultcrantz E (2007) Idiopathic sudden sensorineural hearing loss: results drawn from the Swedish national database. Acta Otolaryngol 127(11):1168–1175. https://doi.org/10.1080/00016480701242477
Oh JH, Park K, Lee SJ, Shin YR, Choung YH (2007) Bilateral versus unilateral sudden sensorineural hearing loss. Otolaryngol Head Neck Surg 136(1):87–91. https://doi.org/10.1016/j.otohns.2006.05.015
Park KY, Kim HJ, Ahn HS, Yim SY, Jun JB (2017) Association between acute gouty arthritis and meteorological factors: an ecological study using a systematic review and meta-analysis. Semin Arthritis Rheum 47(3):369–375. https://doi.org/10.1016/j.semarthrit.2017.05.006
Preyer S (1996) The influence of weather on the incidence of sudden idiopathic hearing loss. Laryngorhinootologie 75(8):443–446. https://doi.org/10.1055/s-2007-997612
Quaranta N, De Ceglie V, D’Elia A (2016) Endothelial dysfunction in idiopathic sudden sensorineural hearing loss: a review. Audiol Res 6(1):151. https://doi.org/10.4081/audiores.2016.151
Ryu IY, Park SH, Park EB, Kim HJ, Kim SH, Yeo SG (2017) Factors prognostic of season-associated sudden sensorineural hearing loss: a retrospective observational study. J Audiol Otol 21(1):44–48. https://doi.org/10.7874/jao.2017.21.1.44
Sakata T, Kato T (2006) Feeling of ear fullness in acute sensorineural hearing loss. Acta Otolaryngol 126(8):828–833. https://doi.org/10.1080/00016480500527268
Sakata T, Esaki Y, Yamano T, Sueta N, Nakagawa T, Kato T (2009) Air pressure-sensing ability of the middle ear-Investigation of sensing regions and appropriate measurement conditions. Auris Nasus Larynx 36(4):393–399. https://doi.org/10.1016/j.anl.2008.11.007
Sakata T, Higuchi H, Ueno T, Nakagawa T (2012) Modulation of somatosensory abilities and the feeling of ear fullness in patients with acute sensorineural hearing loss. Auris Nasus Larynx 39(3):265–269. https://doi.org/10.1016/j.anl.2011.05.004
Seo J-H, Jeon E-J, Park Y-S, Kim J, Chang K-H, Yeo S-W (2014) Meteorological conditions related to the onset of idiopathic sudden sensorineural hearing loss. Yonsei Med J 55(6):1678–1682. https://doi.org/10.3349/ymj.2014.55.6.1678
Shao M, Yu L, Xiao C, Deng J, Yang H, Xu W et al (2021) Short-term effects of ambient temperature and pollutants on the mortality of respiratory diseases: a time-series analysis in Hefei, China. Ecotoxicol Environ Saf 215:112160. https://doi.org/10.1016/j.ecoenv.2021.112160
Simani L, Oron Y, Shapira U, Handzel O, Abu Eta R, Warshavsky A et al (2022) Is idiopathic sudden sensorineural hearing loss seasonal? Otol Neurotol. https://doi.org/10.1097/mao.0000000000003661
Tang SE, Wu SY, Jhou FY, Chung CH, Chien WC, Wang CH (2022) Comparison of the incidence of sudden sensorineural hearing loss in Northern Taiwan and Southern Taiwan (2000–2015). J Med Sci (taiwan) 42(5):228–235. https://doi.org/10.4103/jmedsci.jmedsci_267_21
Tsai SC, Hsu YC, Lai JN, Chou RH, Fan HC, Lin FC et al (2021) Long-term exposure to air pollution and the risk of developing sudden sensorineural hearing loss. J Transl Med 19(1):424. https://doi.org/10.1186/s12967-021-03095-8
Umesawa M, Kobashi G, Kitoh R, Nishio SY, Ogawa K, Hato N et al (2017) Relationships among drinking and smoking habits, history of diseases, body mass index and idiopathic sudden sensorineural hearing loss in Japanese patients. Acta Otolaryngol 137(sup565):S17–S23. https://doi.org/10.1080/00016489.2017.1297898
Wilson WR (1986) The relationship of the herpesvirus family to sudden hearing loss: a prospective clinical study and literature review. Laryngoscope 96(8):870–877. https://doi.org/10.1002/lary.1986.96.8.870
Xie W, Dai Q, Liu J, Liu Y, Hellstrom S, Duan M (2020) Analysis of clinical and laboratory findings of idiopathic sudden sensorineural hearing loss. Sci Rep 10(1):6057. https://doi.org/10.1038/s41598-020-63046-z
Yun CJ, Cho SI, Hoonjae Oh (2014) The relationship of intra-annual distribution of sudden sensorineural hearing loss versus meteorological parameters yearly distribution of sudden hearing loss and its relationship to climatic factors. Korean J Otorhinolaryngol Head Neck Surg 57(12):826–829. https://doi.org/10.3342/kjorl-hns.2014.57.12.826
Zhang JL, Fang X, Lee S, Ma X, Yu LS, Jing YY (2019a) [Correlation analysis of incidence, season and temperature parameters of different types of sudden deafness]. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 33(8):692–695. https://doi.org/10.13201/j.issn.1001-1781.2019.08.003
Zhang JL, Fang X, Lee S, Ma X, Yu LS, Jing YY (2019b) [Correlation analysis of incidence, season and temperature parameters of different types of sudden deafness]. Lin chuang er bi yan hou tou jing wai ke za zhi J Clin Otorhinolaryngol Head Neck Surg 33(8):692–695. https://doi.org/10.13201/j.issn.1001-1781.2019.08.003
Zhang J, Ji S, Ma X, Yu L, Jing Y (2021b) Association between meteorological factors and audiogram configurations in patients with sudden sensorineural hearing loss: a cross-sectional study. BMJ Open 11(12):e045768. https://doi.org/10.1136/bmjopen-2020-045768
Zhang J, Ji S, Ma X, Yu L, Jing Y (2021a) Association between meteorological factors and audiogram configurations in patients with sudden sensorineural hearing loss: a cross-sectional study. BMJ Open 11(12). https://doi.org/10.1136/bmjopen-2020-045768
Acknowledgements
We thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Funding
The study was supported by funding from the National Natural Science Foundation of China [Grant No.82071055], the Incubation Program of the National Natural Science Foundation of China [Grant No. 2019GMFY06], and the Subject Co-construction project of Anhui Medical University [Grant No.2021lcxk036].
Author information
Authors and Affiliations
Contributions
Xiaobo Li, Yanxun Han, Ziyue Fu: designed the study. Yuchen Zhang and Min Fan: revision of manuscript. Shujia Sang and Xixi Chen: writing the manuscript. Bingyu Liang, Yuchen Liu and Pengcheng Lu: collecting and processing data. Huawei Li, Haifeng Pan, and Jianming Yang: analysis and interpretation of data. Jianming Yang is the sole corresponding author of this manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Ethical Committee of the Anhui Medical University. All procedures were taken follow the ethical standards of the Declaration of Helsinki.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The equal Author contribution statement and Acknowledgments are missing in the published proof.
Xiao-Bo Li, Yan-Xun Han and Zi-Yue Fu have contributed equally to this work and share the first authorship.
Acknowledgements
We thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, XB., Han, YX., Fu, ZY. et al. Association of sudden sensorineural hearing loss with meteorological factors: a time series study in Hefei, China, and a literature review. Environ Sci Pollut Res 31, 42970–42990 (2024). https://doi.org/10.1007/s11356-024-33943-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-024-33943-1