Abstract
Background
Acute otitis media (AOM) is a prevalent childhood acute illness, with 13.6 million pediatric office visits annually, often stemming from upper respiratory tract infections (URI) and affected by environmental factors like air pollution and cold seasons.
Methods
Herein, we made use of territory-wide hospitalization data to investigate the relationships between meteorological factors, air pollutants, influenza infection, and AOM for children observed from 1998 to 2019 in Hong Kong. Quasi-Poisson generalized additive model, combined with a distributed-lag non-linear model, was employed to examine the relationship between weekly AOM admissions in children and weekly influenza-like illness-positive (ILI +) rates, as well as air pollutants (i.e., oxidant gases, sulfur dioxide, and fine particulate matter), while accounting for meteorological variations.
Results
There were 21,224 hospital admissions due to AOM for children aged ≤ 15 years throughout a 22-year period. The cumulative adjusted relative risks (ARR) of AOM were 1.15 (95% CI, 1.04–1.28) and 1.07 (95% CI, 0.97–1.18) at the 95th percentile concentration of oxidant gases (65.9 ppm) and fine particulate matter (62.2 μg/m3) respectively, with reference set to their medians of concentration. The ARRs exhibited a monotone increasing trend for all-type and type-specific ILI + rates. Setting the reference to zero, the cumulative ARRs of AOM rose to 1.42 (95% CI, 1.29–1.56) at the 95th percentile of ILI + Total rate, and to 1.07 (95% CI, 1.01–1.14), 1.19 (95% CI, 1.11–1.27), and 1.22 (95% CI, 1.13–1.32) for ILI + A/H1N1, A/H3N2, and B, respectively.
Conclusions
Our findings suggested that policy on air pollution control and influenza vaccination for children need to be implemented, which might have significant implications for preventing AOM in children.
Similar content being viewed by others
Background
Acute otitis media (AOM) is an infection that occurs in the middle ear usually accompanied by pain [1]. AOM is a common childhood disease with one in five children having at least an episode of AOM by the age of one. Approximately 60% of children will experience AOM at least one time by the age of three [2]. The high incidence rate of AOM imposes a significant burden on medical expenditure. In the United States, AOM accounts for an annual outpatient cost of $314 per child, and is associated with an extra medical expenditure of $2.88 billion per year [3]. Moreover, as most AOM cases are associated with bacterial infection such as Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis, [4] more than 70% AOM children are prescribed with antibiotics [5, 6], raising serious concern to antimicrobial resistance [7, 8]. The occurrence of AOM presents an extensive seasonal variation, with 66% of visits identified between November and April of each year [9], parallel to the influenza seasons.
Influenza infection is a risk factor for AOM occurrence. Most cases of AOM are preceded by a viral upper respiratory tract infection (URI). Such infection could subsequently induce inflammation of the Eustachian tube and negative middle ear pressure. These conditions thus facilitate the entrance of secretions containing both colonized infecting virus and pathogenic bacteria from the nasopharynx into the middle ear [10]. Common types of viruses associated with AOM include respiratory syncytial virus, adenovirus, rhinovirus, and influenza virus [11]. According to Nokso-Koivisto et al., of 303 URI episodes associated with single virus, the rate of AOM complicating URI associated with influenza virus was 31% [12]. Annual influenza vaccination is recommended for children older than six months [13] as it results in a 4% absolute reduction in AOM episodes and a 30% to 55% reduction in AOM during the respiratory illness season [14, 15].
The increased AOM risk under exposure to high concentration of air pollutants was supported by several epidemiological studies. Zemek R et al. studied the relationship between the incidence of AOM and air pollutants in children population, and suggested an exposure to nitrogen dioxide (NO2) was associated with the incidence of AOM [16]. Wang et al. revealed that AOM outpatient visit was positively correlated with sulfur dioxide (SO2), while ozone (O3) exhibited a negative correlation with it [17]. Apart from that, a retrospective study also found that particulate matters (i.e., PM2.5 and PM10) have adverse effects on AOM in children [18].
Although the relationship between air pollution and AOM in children was well supported by a wealth of evidence, to our knowledge, there are limited studies examining the effects of multiple exposome, including both pollutants and seasonal influenza on AOM at the population level. With the comprehensive population-based hospitalization records spanning from 1998 to 2019, our study aims to elucidate the relationships between air pollutants, meteorological factors, seasonal influenza, and AOM in children in Hong Kong, a non-industrial influenza epicenter.
Methods
Data sources
Hospital admission data
We collected weekly hospital admission data for children aged 0 to 15 years who were diagnosed with AOM from all public hospitals in Hong Kong, using the aggregated data provided by the Hong Kong Hospital Authority. The investigation data were obtained for the period between January 1, 1998, and December 31, 2019. Diagnoses of AOM for hospital admissions were identified based on codes 381–382 from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM).
Air pollutants data
We collected weekly average levels of air pollutants from the Environment Protection Department, including NO2, SO2, O3, and PM2.5, which were measured by 13 general air monitoring stations namely Central/Western, Eastern, Kwai Chung, Kwun Tong, Sham Shui Po, Sha Tin, Tai Po, Tap Mun, Tseng Kwan O, Tsuen Wan, Tuen Mun, Tung Chung, and Yuen Long. However, Tap Mun station, located in a remote area with low population density, was excluded from the analysis. The pollutant concentrations were then averaged on a weekly basis using data from the remaining 12 general air monitoring stations.
We used redox-weighted oxidant capacity (Ox), calculated as Ox = (1/3) NO2 + (2/3) O3, to represent the combined oxidative effect of NO2 and O3 [19], which has been used in similar studies [20, 21]. The redox-weighted oxidant capacity was proven to be an alternative proxy for atmospheric oxidation capacity, which is better than the unweighted oxidant capacity [22].
Meteorological data
The data of weekly mean ambient temperature, mean relative humidity, and total rainfall were obtained from the Hong Kong Observatory, and they were measured in the station of the Hong Kong Observatory Headquarters.
Influenza data
Weekly consultation rates of influenza-like illness (ILI) were obtained from a local sentinel surveillance system which contains 64 general outpatient clinics and over 40 private medical practitioner clinics from the Center for Health Protection, Hong Kong. The surveillance system reported the proportion of outpatient consultations with cough, fever > 38.5℃, and sore throat on a weekly basis. Surveillance data on influenza virus isolation were obtained from the Public Health Laboratory Service of the Centre for Health Protection. Outpatient clinics and inpatient hospitals regularly submitted respiratory specimens to the Branch for surveillance and diagnosis. The number of test specimens was collected, and the number of influenza-positive specimens was classified by type and subtype. We further determined the influenza-like illness-positive (ILI +) rate as a proxy for influenza activity by multiplying the proportion of ILI consultations by the proportion of positive respiratory specimens for a specific influenza subtype. The proportion of ILI consultations reflects the changing numbers of sick individuals sampled for testing, while the viral positivity indicator accounts for variation in the proportion of ILI cases that are attributable to influenza infection. Consequently, the use of ILI + rates can not only reduce the sampling uncertainty of laboratory testing when there are fewer samples to be tested during periods of non-influenza epidemics, but also reduce the number of over-diagnoses from clinical consultations [23,24,25,26]. The aggregation time series of ILI + A/H1N1, A/H3N2, and B, as well as the combined rate including all influenza strains (i.e., ILI + Total) were obtained.
Statistical methods
To examine the effects of air pollutants, weather factors, and influenza on AOM, we used quasi-Poisson generalized additive models in combination with the distributed lag non-linear model (DLNM) [27,28,29]. The full form of the model is as follows:
where μt is the expected number of AOM admissions in a given week. The cross-basis function cb(.) is employed to model both the relationship between exposure and response, as well as delayed effects. Function s(.) represents a smoothing spline function. As PM2.5, SO2, and Ox are highly correlated with each other, the effect of these air pollutants was examined individually as the term pollutantt in the model to avoid collinearity. The mean temperature (tempt), relative humidity (humidt), total rainfall (raint), and the rate of ILI + Total (ILI + Totalt) at week t were included in the model. Yeart and weekt denote the year and the week of the year, respectively, which were used to capture long-term trends and seasonal patterns. The offset term (offsett) represents the natural logarithm of the total number of hospital admissions for all causes in week t. The degrees of freedom of the exposure variables and lag parameters in the cb(.) functions were determined through the minimization of the generalized cross-validation statistic, with a maximum lag of 2 weeks. The assumption of maximum lag was additionally tested by altering it to 1 week and 3 weeks.
We examined the association of each influenza type by substituting the term ILI + Totalt with a combination of the terms ILI + A/H1N1t, ILI + A/H3N2t, and ILI + Bt,
The exposure effects were quantified using cumulative adjusted relative risk (ARR) over the lag period, accompanied by the corresponding 95% confidence intervals (CIs). The medians of air pollutants and meteorological variables such as mean temperature and relative humidity served as their respective reference values, while zero was set as the reference value for ILI + rates and rainfall.
In light of the previous outbreaks of severe acute respiratory syndrome (SARS) in 2003 and swine-originated influenza A (H1N1) in 2009 experienced in Hong Kong, we conducted a sensitivity analysis by excluding data from these two years to account for any potential disruptions in hospitalization patterns and ensure the robustness of the results.
All the statistical analyses were performed in the R environment (version 4.0.3; ) using the “dlnm” and “mgcv” packages.
Results
Descriptive statistics of the weekly hospital admissions due to AOM, ILI + rates, meteorological variables, and air pollutants from 1998 to 2019 in Hong Kong are presented in Table 1, and the temporal trends of ILI + rates and environmental factors are shown in Figure S1. There were 21,224 hospital admissions for AOM throughout the study period, with a median (IQR) of 16 (12–23) AOM admissions per week. The median rate (IQR) of ILI + Total was 3.40 (1.23–8.02) per 1,000 consultations, with ILI + A/H3N2 being the dominant strain. Pearson correlation coefficients between air pollutants are presented in Table S1.
A high concentration of Ox, among air pollutants examined, exhibited a statistically significant association with an increased risk of AOM admissions (Fig. 1). The cumulative ARR of admission at the 95th percentile of Ox concentration (65.9 ppm) was 1.15 (95% CI, 1.04–1.28), using the median Ox concentration (42.8 ppm) as the reference value. Similarly, the 95th percentile of PM2.5 concentration (62.2μg/m3) was marginally significantly associated with AOM, with a cumulative ARR of 1.07 (95% CI, 0.97–1.18) compared to the median level (30.3μg/m3). However, no significant associations were found between AOM and SO2 or meteorological factors such as ambient temperature, relative humidity, and total rainfall.
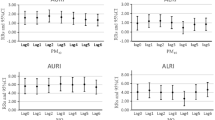
Cumulative adjustive relative risks (ARRs) with 95% confidence intervals on acute otitis media admissions against different environmental variables. The cumulative ARRs at the 95th percentiles of the environmental variables were dotted in the figures. The reference values were set as zero for total rainfall, and medians for other environmental variables
The rates of ILI + Total, ILI + A/H1N1, ILI + A/H3N2, and ILI + B were all found to be significantly associated with an increased risk of AOM admissions (Fig. 2). When the reference rate for ILI + Total was set to zero, the cumulative ARR of AOM admissions rose to 1.42 (95% CI, 1.29–1.56) at the 95th percentile of ILI + Total rate. In addition, the cumulative ARRs increased to 1.07 (95% CI, 1.01–1.14), 1.19 (95% CI, 1.11–1.27), and 1.22 (95%CI, 1.13–1.32) for ILI + A/H1N1, A/H3N2, and B, respectively, when their rates reached the 95th percentile.
In the sensitivity analyses, although excluding data from 2003 and 2009 led to slight alterations in the cumulative ARRs of the variables of interest, their significance remained unchanged (Figure S2 and S3).
Discussion
In this study, we elucidate the relationships between multiple environmental factors, seasonal influenza, and AOM in children in Hong Kong. According to our results, a high concentration of PM2.5 and oxidant gases increased the risk of AOM hospitalization in pediatric patients. Previous studies have reported air pollutants influence the occurrence of otitis media (OM), but the results were generally inconsistent [16, 30,31,32]. A study conducted in Canada suggested that exposure to carbon monoxide and NO2 were positively related to AOM, especially in warmer months, while PM2.5 was not found to be a risk factor [16]. Nevertheless, some investigations reported a strong link between OM and multiple air pollutants, particularly in the warm seasons for children with a recent history of URI [31]. We speculate that the variation in levels of air pollutants, individual exposure patterns, and the socioeconomic characteristics of the participants may contribute to the inconsistent results among the studies [33].
We showed that oxidant gases were positively associated with the risk of AOM hospitalization in children. In fact, many in vivo and in vitro studies suggested plausible pathophysiological mechanisms for the relationship. Firstly, short-term exposure to NO2 results in a significant reduction in mucociliary activity, which may disrupt mucociliary clearance in the middle ear and upper airway. This ultimately leads to eustachian tube dysfunction, which causes middle ear fluid stasis and subsequent middle ear infections [34, 35]. Secondly, acute exposure to oxidant gases induces ciliostasis in the upper and lower airways, preventing the nasal and bronchial mucosa from filtering inhaled particles, such as airborne allergens, bacteria, or viruses, which makes children more susceptible to viral diseases of the upper respiratory tract, thus resulting in AOM [36, 37]. Meanwhile, oxidant gases can amplify the production of inflammatory cytokines by infected cells, exacerbating virus-induced inflammation of the respiratory system [38,39,40].
In our study, an increased PM2.5 was marginally associated with a higher risk of AOM in the children population. Literature has indeed suggested potential pathophysiological mechanisms to explain the association. Inhalation of PM2.5 may lead to particulate matters passing through the nasopharyngeal cavity and entering the airways and lungs, where the expression of genes associated with the inflammatory response is upregulated and mucus protein secretion is stimulated [41, 42]. Increased mucus proteins and inflammatory responses are capable of narrowing or blocking the eustachian tube, allowing pathogen growth and susceptibility to middle ear inflammation. Moreover, exposure to PM2.5 may further reduce mucus clearance by cilia, leading to inflammation and increased susceptibility to AOM [43].
In this study, we showed that seasonal influenza was associated with an increased risk of AOM admissions. Not surprisingly, influenza and other respiratory viruses are known to be common causes of AOM. Upper respiratory tract infection causes congestion of the nasopharyngeal mucosa and inflammation of the eustachian tube [44]. This can lead to eustachian tube dysfunction, which is thought to be the most important factor in the development of AOM [45]. Apart from that, studies have demonstrated that respiratory viruses promote the release of inflammatory mediators, some of which (e.g., histamine, kinins) can induce eustachian tube dysfunction [46]. Eustachian tube dysfunction hinders the clearance of middle ear secretions, leading to fluid accumulation. Bacteria and viruses can easily grow in the accumulated fluid, thus causing acute otitis media. In spite of a strong link between influenza and AOM, the risk of influenza A/H1N1 was lower than that of A/H3N2 and B. We speculate that the variation of susceptibility by influenza type may influence the magnitude of risk for AOM incidents [47].
While studies demonstrated that meteorological factors could be related to the incidence of AOM [48], we did not identify any significant meteorological factors as risk factors. In fact, dry and cold conditions were suggested to cause dryness of the nasal and nasopharyngeal mucosa and reduced surface ciliary activity, increasing the spread of pathogens [48]. As the incidence of influenza also peaks in cold seasons, we suspect that the elevated risk of AOM in cold temperatures may be due to the modulating effect of influenza infection.
This study also has some limitations. Firstly, it is a modelling study using aggregate data to draw relevant conclusions, so ecological fallacies may occur. Secondly, in our data analysis, we didn’t take the influenza vaccination rate into account, while the vaccination uptake rate was low during the study period [49].
Conclusions
We demonstrated that exposure to PM2.5, oxidant gases, and seasonal influenza were risk factors for AOM in children in Hong Kong, a non-industrial influenza epicenter. Given the high incidence of AOM in children and the ubiquitous characteristic of air pollutant exposure, influenza vaccination and policy on air pollution control are necessary to be implemented.
Availability of data and materials
The data that support the findings of this study are available from the Hospital Authority, The Government of the Hong Kong Special Administrative Region but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Hospital Authority.
References
Centers for Disease Control and Prevention. Ear Infections. 2013. Available from: https://web.archive.org/web/20150219034155/http://www.cdc.gov/getsmart/antibiotic-use/uri/ear-infection.html. Cited 2022 10 Dec.
Kaur R, Morris M, Pichichero ME. Epidemiology of acute otitis media in the postpneumococcal conjugate vaccine era. Pediatrics. 2017;140(3):e20174067. https://doi.org/10.1542/peds.2017-0181. Epub 20170807 PubMed PMID: 28784702; PubMed Central PMCID: PMC5574724.
Ahmed S, Shapiro NL, Bhattacharyya N. Incremental health care utilization and costs for acute otitis media in children. Laryngoscope. 2014;124(1):301–5. https://doi.org/10.1002/lary.24190. Epub 20130531 PubMed PMID: 23649905.
Hullegie S, Venekamp RP, van Dongen TMA, Hay AD, Moore MV, Little P, et al. Prevalence and antimicrobial resistance of bacteria in children with acute otitis media and ear discharge: a systematic review. Pediatr Infect Dis J. 2021;40(8):756–62. https://doi.org/10.1097/inf.0000000000003134. PubMed PMID:34166300;PubMed Central PMCID:PMC8274581.
Olsen JK, Lykkegaard J, Hansen MP, Waldorff FB, Lous J, Andersen MK. Prescription of antibiotics to children with acute otitis media in Danish general practice. BMC Fam Pract. 2020;21(1):177. https://doi.org/10.1186/s12875-020-01248-0. PubMed PMID: 32854621; PubMed Central PMCID: PMC7457240.
Kim SH, Kim JR, Song JJ, Chae SW. Trend and patterns in the antibiotics prescription for the acute otitis media in Korean children. Int J Pediatr Otorhinolaryngol. 2020;130:109789. https://doi.org/10.1016/j.ijporl.2019.109789. Epub 20191122. PubMed PMID: 31805491.
Sillanpää S, Sipilä M, Hyöty H, Rautiainen M, Laranne J. Antibiotic resistance in pathogens causing acute otitis media in Finnish children. Int J Pediatr Otorhinolaryngol. 2016;85:91–4. https://doi.org/10.1016/j.ijporl.2016.03.037. Epub 20160411. PubMed PMID: 27240503.
Zielnik-Jurkiewicz B, Bielicka A. Antibiotic resistance of Streptococcus pneumoniae in children with acute otitis media treatment failure. Int J Pediatr Otorhinolaryngol. 2015;79(12):2129-33.https://doi.org/10.1016/j.ijporl.2015.09.030. Epub 20150930. PubMed PMID: 26454530
Stockmann C, Ampofo K, Hersh AL, Carleton ST, Korgenski K, Sheng X, et al. Seasonality of acute otitis media and the role of respiratory viral activity in children. Pediatr Infect Dis J. 2013;32(4):314–9. https://doi.org/10.1097/INF.0b013e31827d104e. PubMedPMID:23249910;PubMedCentralPMCID:PMC3618601.
Kalu SU, Ataya RS, McCormick DP, Patel JA, Revai K, Chonmaitree T. Clinical spectrum of acute otitis media complicating upper respiratory tract viral infection. Pediatr Infect Dis J. 2011;30(2):95–9. https://doi.org/10.1097/INF.0b013e3181f253d5. PubMedPMID:20711085;PubMedCentralPMCID:PMC3010420.
Nokso-Koivisto J, Marom T, Chonmaitree T. Importance of viruses in acute otitis media. Curr Opin Pediatr. 2015;27(1):110–5. https://doi.org/10.1097/mop.0000000000000184. PubMedPMID:25514574;PubMedCentralPMCID:PMC4383320.
Nokso-Koivisto J, Pyles RB, Miller AL, Jennings K, Loeffelholz M, Chonmaitree T. Role of human bocavirus in upper respiratory tract infections and acute otitis media. J Pediatric Infect Dis Soc. 2014;3(2):98–103. https://doi.org/10.1093/jpids/pit061. PubMed PMID: 26625362; PubMed Central PMCID: PMC4865000.
Centers for Disease Control and Prevention. Pneumococcal vaccine recommendations. Available from: https://www.cdc.gov/vaccines/vpd/pneumo/hcp/recommendations.html. Cited 2022 10 December.
Lieberthal AS, Carroll AE, Chonmaitree T, Ganiats TG, Hoberman A, Jackson MA, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013;131(3):e964-99. https://doi.org/10.1542/peds.2012-3488. Epub 20130225. PubMed PMID: 23439909.
Norhayati MN, Ho JJ, Azman MY. Influenza vaccines for preventing acute otitis media in infants and children. Cochrane Database Syst Rev. 2017;10(10):Cd010089. https://doi.org/10.1002/14651858.CD010089.pub3. Epub 20171017 PubMed PMID: 29039160; PubMed Central PMCID: PMC6485791.
Zemek R, Szyszkowicz M, Rowe BH. Air Pollution and emergency department visits for otitis media: a case-crossover study in Edmonton, Canada. Environ Health Perspect. 2010;118(11):1631–6. https://doi.org/10.1289/ehp.0901675.
Wang X, Wang M, Wang J, Tian H, Zhong C. Research on the correlation between otorhinolaryngologic diseases and environmental meteorological factors in children. Journal of Clinical Otorhinolaryngology Head and Neck Surgery. 2020;34(6):546–53. https://doi.org/10.13201/j.issn.2096-7993.2020.06.016.
Park M, Han J, Park J, Jang MJ, Park MK. Particular matter influences the incidence of acute otitis media in children. Sci Rep. 2021;11(1):19730. https://doi.org/10.1038/s41598-021-99247-3. Epub 20211005. PubMed PMID: 34611241; PubMed Central PMCID: PMC8492675.
Weichenthal S, Pinault LL, Burnett RT. Impact of oxidant gases on the relationship between outdoor fine particulate air pollution and nonaccidental, cardiovascular, and respiratory mortality. Sci Rep. 2017;7(1):16401. https://doi.org/10.1038/s41598-017-16770-y.
Chong KC, Chen Y, Chan EYY, Lau SYF, Lam HCY, Wang P, et al. Association of weather, air pollutants, and seasonal influenza with chronic obstructive pulmonary disease hospitalization risks. Environ Pollut. 2022;293:118480. https://doi.org/10.1016/j.envpol.2021.118480. Epub 20211109 PubMed PMID: 34763018.
Chong KC, Yeoh EK, Leung CC, Lau SYF, Lam HCY, Goggins WB, et al. Independent effect of weather, air pollutants, and seasonal influenza on risk of tuberculosis hospitalization: an analysis of 22-year hospital admission data. Sci Total Environ. 2022;837:155711. https://doi.org/10.1016/j.scitotenv.2022.155711. Epub 20220504. PubMed PMID: 35523336.
Guo H. Comparisons of combined oxidant capacity and redox-weighted oxidant capacity in their association with increasing levels of FeNO. Chemosphere. 2018;211:584–90. https://doi.org/10.1016/j.chemosphere.2018.07.191.
Cowling BJ, Wong IOL, Ho L-M, Riley S, Leung GM. Methods for monitoring influenza surveillance data. Int J Epidemiol. 2006;35(5):1314–21. https://doi.org/10.1093/ije/dyl162.
Goldstein E, Viboud C, Charu V, Lipsitch M. Improving the estimation of influenza-related mortality over a seasonal baseline. Epidemiology. 2012;23(6):829–38. https://doi.org/10.1097/EDE.0b013e31826c2dda. PubMed PMID: 22992574.
Xiong X, Wei Y, Lam HCY, Wong CKH, Lau SYF, Zhao S, et al. Association between cold weather, influenza infection, and asthma exacerbation in adults in Hong Kong. Sci Total Environ. 2023;857(Pt 1):159362. https://doi.org/10.1016/j.scitotenv.2022.159362. Epub 20221012.PubMed PMID: 36240934.
Li C, Jiang X, Yue Q, Wei Y, Wang Y, Ho JYE, et al. Relationship between meteorological variations, seasonal influenza, and hip fractures in the elderly: a modelling investigation using 22-year data. Science of The Total Environment. 2023;862:160764. https://doi.org/10.1016/j.scitotenv.2022.160764.
Gasparrini A, Armstrong B, Kenward MG. Distributed lag non-linear models. Stat Med. 2010;29(21):2224–34.
Mohammad KN, Chan EYY, Lau SY, Lam HCY, Goggins WB, Chong KC. Relationship between acute kidney injury, seasonal influenza, and environmental factors: A 14-year retrospective analysis. Environ Int. 2021;153:106521. https://doi.org/10.1016/j.envint.2021.106521. Epub 2021/04/06. PubMed PMID: 33819723.
Leung SY, Lau SYF, Kwok KL, Mohammad KN, Chan PKS, Chong KC. Short-term association among meteorological variation, outdoor air pollution and acute bronchiolitis in children in a subtropical setting. Thorax. 2021;76(4):360-9. https://doi.org/10.1136/thoraxjnl-2020-215488. Epub 20210120. PubMed PMID: 33472969.
Park M, Han J, Jang M-j, Suh M-W, Lee JH, Oh SH, et al. Air pollution influences the incidence of otitis media in children: A national population-based study. PLoS One. 2018;13(6):e0199296. https://doi.org/10.1371/journal.pone.0199296.
Oh J, Lee S, Kim MH, Kwag Y, Kim HS, Kim S, et al. The impact of PM2.5 on acute otitis media in children (aged 0–3): A time series study. Environ Int. 2020;145:106133. https://doi.org/10.1016/j.envint.2020.106133.
Gestro M, Condemi V, Bardi L, Fantino C, Solimene U. Meteorological factors, air pollutants, and emergency department visits for otitis media: a time series study. Int J Biometeorol. 2017;61(10):1749–64. https://doi.org/10.1007/s00484-017-1356-7.
Burns J, Boogaard H, Polus S, Pfadenhauer LM, Rohwer AC, van Erp AM, et al. Interventions to reduce ambient air pollution and their effects on health: an abridged cochrane systematic review. Environ Int. 2020;135:105400. https://doi.org/10.1016/j.envint.2020.106133.
Helleday R, Huberman D, Blomberg A, Stjernberg N, Sandstrom T. Nitrogen dioxide exposure impairs the frequency of the mucociliary activity in healthy subjects. Eur Respir J. 1995;8(10):1664–8. https://doi.org/10.1183/09031936.95.08101664.
Bluestone CD. Pathogenesis of otitis media: role of eustachian tube. The Pediatric Infectious Disease Journal. 1996;15(4):281-91. PubMed PMID: 00006454-199604000-00002
Devalia JL, Campbell AM, Sapsford RJ, Rusznak C, Quint D, Godard P, et al. Effect of nitrogen dioxide on synthesis of inflammatory cytokines expressed by human bronchial epithelial cells in vitro. Am J Respir Cell Mol Biol. 1993;9(3):271–8. https://doi.org/10.1165/ajrcmb/9.3.271.
Heikkinen T, Thint M, Chonmaitree T. Prevalence of various respiratory viruses in the middle ear during acute otitis media. N Engl J Med. 1999;340(4):260–4. https://doi.org/10.1056/nejm199901283400402. PubMed PMID: 9920949.
Chauhan AJ, Johnston SL. Air pollution and infection in respiratory illness. Br Med Bull. 2003;68(1):95–112. https://doi.org/10.1093/bmb/ldg022.
Spannhake EW, Reddy SPM, Jacoby DB, Yu X-Y, Saatian B, Tian J. Synergism between rhinovirus infection and oxidant pollutant exposure enhances airway epithelial cell cytokine production. Environ Health Perspect. 2002;110(7):665–70. https://doi.org/10.1289/ehp.02110665.
Lambert AL, Mangum JB, DeLorme MP, Everitt JI. Ultrafine carbon black particles enhance respiratory syncytial virus-induced airway reactivity, pulmonary inflammation, and chemokine expression. Toxicol Sci. 2003;72(2):339–46. https://doi.org/10.1093/toxsci/kfg032.
Song J-J, Kwon JY, Park MK, Seo YR. Microarray analysis of gene expression alteration in human middle ear epithelial cells induced by micro particle. Int J Pediatr Otorhinolaryngol. 2013;77(10):1760–4. https://doi.org/10.1016/j.ijporl.2013.08.012.
Kerschner JE. Mucin gene expression in human middle ear Epithelium. Laryngoscope. 2007;117(9):1666–76. https://doi.org/10.1097/MLG.0b013e31806db531.
Shukla A, Timblin C, BeruBe K, Gordon T, McKinney W, Driscoll K, et al. Inhaled particulate matter causes expression of nuclear factor (NF)-kappa B-related genes and oxidant-dependent NF-kappa B activation in vitro. Am J Respir Cell Mol Biol. 2000;23(2):182–7. https://doi.org/10.1165/ajrcmb.23.2.4035.
Heikkinen T, Chonmaitree T. Importance of respiratory viruses in acute otitis media. Clin Microbiol Rev. 2003;16(2):230–41. https://doi.org/10.1128/CMR.16.2.230-241.2003.
Bluestone CD. Pathogenesis of otitis media: role of eustachian tube. Pediatr Infect Dis J. 1996;15(4):281–91. https://doi.org/10.1097/00006454-199604000-00002.
Doyle WJ, Boehm S, Skoner DP. Physiologic responses to intranasal dose-response challenges with histamine, methacholine, bradykinin, and prostaglandin in adult volunteers with and without nasal allergy. J Allergy Clin Immunol. 1990;86(6 Pt 1):924–35. https://doi.org/10.1016/s0091-6749(05)80156-3. PubMed PMID: 2262647.
Bulut Y, Güven M, Otlu B, Yenişehirli G, Aladağ İ, Eyibilen A, et al. Acute otitis media and respiratory viruses. Eur J Pediatr. 2007;166(3):223–8. https://doi.org/10.1007/s00431-006-0233-x.
Tian H, Xu B, Wang X, Wang J, Zhong C. Study on the correlation between ambient environment-meteorological factors and the number of visits of acute otitis media, Lanzhou, China. J Otol. 2020;15(3):86–94. https://doi.org/10.1016/j.joto.2020.01.002.
Chan DP, Wong NS, Wong EL, Cheung AW, Lee SS. Household characteristics and influenza vaccination uptake in the community-dwelling elderly: a cross-sectional study. Prev Med Rep. 2015;2:803-8. Epub 20150921. https://doi.org/10.1016/j.pmedr.2015.09.002. PubMed PMID: 26844153; PubMed Central PMCID: PMC4721455.
Acknowledgements
The authors would like to thank the Hospital Authority, Hong Kong Observatory, and Hong Kong Environmental Protection Department for providing the data used in this study.
Funding
This work received support from the National Natural Science Foundation of China (grant number 71974165) and partial support from Health and Medical Research Fund (grant number INF-CUHK-1). The funding organizations were not involved in the study design and implementation; data collection, analysis, and interpretation; manuscript preparation, review, and approval; as well as the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Conglu Li: Methodology, Software, Formal analysis, Investigation, Writing—original draft, Visualization. Xiaoting Jiang: Methodology, Investigation, Writing—original draft, Writing—review & editing. Yuchen Wei: Methodology, Writing—review & editing, Supervision. Yawen Wang: Methodology, Writing—review & editing. Xiang Qian Lao: Writing—review & editing, Supervision. Qianying Yue: Data Curation, Methodology, Software, Formal analysis, Investigation, Writing—original draft, Visualization. Ka Chun Chong: Conceptualization, Methodology, Resources, Writing—review & editing, Supervision, Funding acquisition.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This was an observational study using aggregate data provided and permitted to use by the Hospital Authority, The Government of the Hong Kong Special Administrative Region. The data used in this study was anonymized before its use. Either ethics approval or informed consent was waived.
Consent for publication
NA.
Competing interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12889_2024_18962_MOESM1_ESM.pdf
Additional file 1: Figure S1. Temporal trends of influenza-like illness-positive (ILI+) rates and environmental variables in Hong Kong from 1998 to 2019.
12889_2024_18962_MOESM2_ESM.pdf
Additional file 2: Figure S2. Sensitivity analysis for impacts of environmental variables when data from 2003 and 2009 were removed. The cumulative adjustive relative risks (ARRs) at the 95th percentiles of the environmental variables were dotted in the figures. The reference values were set as zero for total rainfall, and medians for other environmental variables.
12889_2024_18962_MOESM3_ESM.pdf
Additional file 3: Figure S3. Sensitivity analysis for impacts of different influenza-like illness-positive (ILI+) rates when data from 2003 and 2009 were removed. The cumulative adjustive relative risks (ARRs) at the 95th percentiles of ILI+ rates were dotted in the figures. The reference values were set as zero.
12889_2024_18962_MOESM4_ESM.docx
Additional file 4: Table S1. Pearson correlation coefficient between different air pollutants during the study period (1998-2019).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, C., Jiang, X., Wei, Y. et al. Air pollutants, seasonal influenza, and acute otitis media in children: a population-based analysis using 22-year hospitalization data. BMC Public Health 24, 1581 (2024). https://doi.org/10.1186/s12889-024-18962-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18962-4