Abstract
Pulmonary rehabilitation is essential in post-COVID subjects, reporting respiratory impairment after the discharge from the hospital. Because the number of patients with respiratory outcomes is high and there are few facilities available, we wonder if a spa setting could represent a valid out-of-hospital alternative. We aim to explore recent evidence related to respiratory rehabilitation in the spa environment to understand if it can represent an appropriate setting for respiratory rehabilitation interventions in post-COVID subjects. Studies were found by screening PubMed, MEDLINE, and Google Scholar databases from 2011 up to February 2021. Studies were eligible if they were reviews, randomized controlled trials (RCTs), or clinical trials, investigating respiratory interventions in the spa environment. Recent evidence has shown that inhalations and mineral-rich water immersions are effective in fighting and preventing multiple chronic respiratory tract diseases. Therefore, these treatments could also be applied to post-COVID patients with medium long-term respiratory outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In late December 2019, the novel coronavirus-2019 (COVID-19) pandemic emerged in Wuhan, China, and soon spread exponentially to more than 200 countries around the globe. At present, 169,597,415 confirmed cases have been reported (World Health Organisation 2021).
Although the infection can manifest with symptoms affecting different systems, the major concern is related to the involvement of the respiratory system. Indeed, although in most cases (80%) the infection proceeds asymptomatically or with mild symptoms, 13.8% of cases have severe disease and 6.1% are critical and require hospitalization in the Intensive Care Unit for significant respiratory involvement (Vermund and Pitzer 2020). Respiratory symptoms include dyspnea, reduced blood oxygen saturation, and respiratory failure, requiring mechanical ventilation primarily in patients with comorbidities such as obesity, diabetes mellitus, ischaemic heart disease, cancer, and chronic obstructive pulmonary disease (COPD) (Siddiq et al. 2020). Patients with mechanical ventilation may also develop acute respiratory distress syndrome (ARDS), pulmonary oedema, atelectasis, and pulmonary embolism with right-sided heart failure (Boyer et al. 2015).
In these patients, early pulmonary rehabilitation treatments can enhance physical outcomes and Quality of Life (QoL) (Brown et al. 2019). The 2013 American Thoracic Society (ATS)/European Respiratory Society (ERS) Statement defines pulmonary rehabilitation as “a comprehensive intervention based on a thorough patient assessment followed by patient-tailored therapies, which include, but are not limited to, exercise training, education, and behaviour change, designed to improve the physical and psychological condition of people with chronic respiratory disease and to promote the long- term adherence of health-enhancing behaviors” (Spruit et al. 2013).
Given the possibility of long-term disabling outcomes involving the cardiorespiratory domain, post-hospitalization pulmonary rehabilitation may be considered in all patients hospitalized with COVID-19 (Wang et al. 2020), also after the resolution of the acute infection. In post-discharge survivors of COVID-19 infection, restrictive ventilation disorders, compromised diffusion capability, and residual impaired lung function have been reported, particularly in elderly patients (You et al. 2020).
Spas can offer rehabilitation interventions for patients with musculoskeletal and neurological disabilities alone or in association with other traditional thermal therapies (Masiero et al. 2020a, b, Bernetti et al. 2020). Since it is necessary to start respiratory treatments as soon as possible, continuous reorganization hospitals and rehabilitation activities are needed (Bai et al. 2021), and there are limited facilities available to treat patients in the post-acute period (Maccarone and Masiero 2021), we aim to explore recent evidence related to pulmonary rehabilitation in the spa environment in order to understand if it can represent an appropriate setting for respiratory rehabilitation interventions in post-COVID subjects.
Material and methods
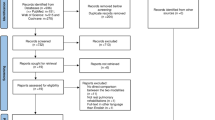
A literature update was conducted with the aim of searching for recent evidence of spa therapy interventions’ effectiveness in respiratory disorders.
Screening of PubMed, MEDLINE, and Google Scholar databases from 2011 up to February 2021 was performed by MCM in order to find studies. The keywords chosen were spa therapy, balneotherapy, Health resort medicine, inhalations, respiratory rehabilitation, and pulmonary rehabilitation. The Boolean Logic has been used to produce various configurations of search strings.
Studies were eligible if they were reviews, randomized controlled trials (RCTs), or clinical trials. Only studies on human subjects and written in English were considered.
Results
Inhalations
Spa treatments specifically targeting the respiratory tract, which include inhalations, aerosol, and nasal showers, are recommended in the treatment of respiratory disorders. They have a well-known therapeutic and preventive effect, stimulating the immune responses and the resistance of the respiratory tract to pathogenic microorganisms. This positive effect is generally based on the patients’ subjective sense of wellbeing, whereas is more difficult to quantify clinical improvements (Corradi et al. 2012).
Inhalations involve inhaling water particles with a diameter of more than 20 μm that reach the mucosa of the nasopharynx and larynx. Therefore, they are indicated in diseases of the upper respiratory tract, such as rhinitis, sinusitis, chronic pharyngitis, and laryngitis.
Sulphur-rich water inhalation has been demonstrated in COPD patients to increase muco-ciliary clearance, decrease the synthesis of pro-inflammatory cytokines and the inflammatory mucosal infiltration, and reduce the levels of elastase produced by the neutrophils. Also, treatment with inhaled salt-bromide-iodine thermal water has been shown to have a mild anti-inflammatory effect on the airways in COPD patients (Khaltaev et al. 2020). Inhalation therapy with salsojodic mineral waters has vasodilating activity on the bronchial mucosa and increases the production of secretory IgA and muco-ciliary clearance (Khaltaev et al. 2020).
In chronic inflammatory diseases of the upper airways nonresponsive to pharmacological therapy, a 14-day course of radioactive water warm vapour inhalations followed by nasal aerosol has been demonstrated to be effective in improving the muco-ciliary clearance (Passali et al. 2013).
In elderly subjects affected by chronic rhinosinusitis treated with crenotherapy with sodium chloride sulphate hyperthermal water, 1 month after the treatment the nasal cytological assessment showed statistically significant improvements in the ciliary motility and in the count of neutrophils (Cantone et al. 2014).
Radon-enriched inhalation therapy has been demonstrated to improve objective indicators of nasal functionality in allergic rhinitis and chronic rhinosinusitis and to cause relief of pulmonary obstruction in asthma (Kesiktas et al. 2011). In patients with airflow obstruction (FEV1/FVC < 0.7), the index FEV1/FVC (forced vital capacity) significantly increased after 12 days of inhalation treatments (Corradi et al. 2012).
Mineral-rich water immersions
The utilization of thermal mineral-rich waters for water immersions is often difficult to study, since it is usually part of the global spa therapy. Physical modalities combined with mineral-rich water immersions have been demonstrated to be associated with significant improvements in dyspnea scale and spirometric measurements in patients affected by fibromyalgia at the end of the treatment and also after 6 months (Passali et al. 2017).
In COPD patients, exercise in thermal water has been demonstrated to be more suitable when compared to gym-based exercises and they could encourage socialization (Khaltaev et al. 2020).
Finally, thermal baths have been shown to improve biochemical parameters in exhaled breath condensate of heavy smokers (Carubbi et al. 2019).
Discussion
For post-COVID-19 subjects, a comprehensive rehabilitative approach comprising a multidisciplinary and professional team, offering cardiorespiratory, neuromuscular, and psychological interventions, is recommended (Agostini et al. 2021). The main goals of respiratory rehabilitation in post-COVID-19 subjects are to improve symptoms of dyspnea, to reduce chronic inflammation in the airways, to ameliorate chest wall kinematics, to reduce complications and long-term outcomes, to minimize disability, and to improve QoL (Wang et al. 2020, Liu et al. 2020, Antonelli and Donelli 2020).
Since recent evidence has shown that in chronic pathologies of the lower and upper respiratory tract, thermal water treatments are effective in improving respiratory function, the use of spa therapy can be hypothesized also in post-COVID patients with persistent respiratory outcomes.
The spa setting, benefiting also from a multidisciplinary staff, can offer specific breathing physio-kinesiotherapy associated with mineral waters inhalation treatments, focused on the enhancement of respiratory outcomes that could affect COVID-19 survivor (Antonelli and Donelli 2020; Masiero et al. 2020a).
Mineral-rich water inhalations have been demonstrated to be effective in ameliorating the elastic properties of pulmonary interstitium, reducing inflammation, and stimulating the muco-ciliary function. One of the current hypotheses explaining the mechanism of action of inhalation treatments is that inhalations can replace or increase glutathione (GSH), reducing oxidative stress associated with inflammation in lung disorders and production of reactive oxygen species (ROS) (Corradi et al. 2012). The heat applied to the whole body during the water immersions could have ulteriorly positive effects on the respiratory system modulating innate and acquired immune defences (Cohen 2020; Masiero et al. 2020b; Maccarone et al. 2021a; Maccarone et al. 2020).
Spa treatments can also offer psychological benefits and enhance mental wellness, improving relaxation and increasing stress resilience and QoL (Antonelli and Donelli 2020; Masiero et al. 2020a; Cohen 2020).
Moreover, spa setting can represent an appropriate location to take care of comorbidities such as obesity, advanced age, COPD, fatigue, neurological, and musculoskeletal conditions (Masiero et al. 2020a; Masiero 2008; Masiero et al. 2018; Masiero et al. 2019; Maccarone et al. 2021b).
Combining all these beneficial effects, in the spa setting, customized post-COVID programmes could be drawn, referring, as suggested by Antonelli et al. [20], to already existing rehabilitative plans, such as those ones prescribed for work-related respiratory diseases.
Finally, we would like to remark that post-COVID-19 subjects accessing spa treatments must not be infectious anymore, which means that they must have no residual symptoms and two consecutive negative RT-PCR results (Antonelli and Donelli 2020; Masiero et al. 2020a).
Conclusion
Recent evidence has shown that different treatments using thermal water are effective in several respiratory tract diseases; therefore, spa environment could represent an appropriate out-of-hospital setting for respiratory rehabilitation in post-COVID subject. Further studies are needed to test the effectiveness of respiratory rehabilitation protocols in the spa setting for these patients.
References
Agostini F, Mangone M, Ruiu P, Paolucci T, Santilli V, Bernetti A (2021) Rehabilitation setting during and after Covid-19: an overview on recommendations. J Rehabil Med 53(1):jrm00141. https://doi.org/10.2340/16501977-2776
Antonelli M, Donelli D (2020) Respiratory rehabilitation for post-COVID19 patients in spa centers: first steps from theory to practice. Int J Biometeorol 64:1811–1813. https://doi.org/10.1007/s00484-020-01962-5
Bai AV, Rabasco J, Ceccatelli V, Floridia S, Sbardella S, Petrignani C, Agostini F, Paoloni M (2021) (2021) Suggestions for changes in professional procedures and adaptation to COVID-19: new models of care in the rehabilitation setting. Ann Ig 33(3):299–304. https://doi.org. https://doi.org/10.7416/ai.2021.2434
Bernetti A, Mangone M, Alviti F, Paolucci T, Attanasi C, Murgia M, Di Sante L, Agostini F, Vitale M, Paoloni M (2020) Spa therapy and rehabilitation of musculoskeletal pathologies: a proposal for best practice in Italy. Int J Biometeorol 64(6):905–914. https://doi.org/10.1007/s00484-019-01731-z
Boyer AF, Schoenberg N, Babcock H, McMullen KM, Micek ST, Kollef MH (2015) A prospective evaluation of ventilator-associated conditions and infection-related ventilator-associated conditions. Chest. 147:68–81
Brown SM, Bose S et al (2019) Approaches to addressing post-intensive care syndrome among intensive care unit survivors. A narrative review Ann Am ThoracSoc 16:947–956
Cantone E, Marino A, Ferranti I, Castagna G, Maione N, Dirubbo V, Iengo M (2014) Nasal cytological assessment after crenotherapy in the treatment of chronic rhinosinusitis in the elderly. Int J ImmunopatholPharmacol 27(4):683–687. https://doi.org/10.1177/039463201402700427
Carubbi C, Masselli E, Calabrò E, Bonati E, Galeone C, Andreoli R, Goldoni M, Corradi M, Sverzellati N, Pozzi G, Banchini A, Pastorino U, Vitale M (2019) Sulphurous thermal water inhalation impacts respiratory metabolic parameters in heavy smokers. Int J Biometeorol 63:1209–1216
Cohen M (2020) Turning up the heat on COVID-19: heat as a therapeutic intervention. F1000Res 9:292. https://doi.org/10.12688/f1000research.23299.2
Corradi M, Folesani G, Gergelova P, Goldoni M, Pinelli S, Gainotti G, de Palma G, Mutti A (2012) Effect of salt-bromide-iodine thermal water inhalation on functional and biochemical lung parameters. ISRN Pulmonology 2012:1–8. https://doi.org/10.5402/2012/534290
Kesiktas N, Karagülle Z, Erdogan N, Yazıcıoglu K, Yılmaz H, Paker N (2011) The efficacy of balneotherapy and physical modalities on the pulmonary system of patients with fibromyalgia. J Back MusculoskeletRehabil 24(1):57–65. https://doi.org/10.3233/BMR-2011-0276
Khaltaev N, Solimene U, Vitale F, Zanasi A (2020) Balneotherapy and hydrotherapy in chronic respiratory disease. Journal of Thoracic Disease 12(8):4459–4468
Liu K, Zhang W, Yang Y, Zhang J, Li Y, Chen Y (2020) Respiratory rehabilitation in elderly patients with COVID-19: a randomized controlled study. Complement TherClinPract 39:101166. https://doi.org/10.1016/j.ctcp.2020.101166
Maccarone MC, Masiero S (2021) The important impact of COVID-19 pandemic on the reorganization of a Rehabilitation Unit in a National Healthcare System hospital in Italy. Am J Phys Med Rehabil 100:327–330. https://doi.org/10.1097/PHM.0000000000001707
Maccarone MC, Magro G, Solimene U, Masiero S (2020) The effects of balneotherapy on human immune function: should baths and mud applications have a role during Covid-19 pandemic? Bulletin of rehabilitation medicine 3:22–24. https://doi.org/10.38025/2078-1962-2020-97-3-22-24
Maccarone MC, Magro G, Solimene U, Scanu A, Masiero S (2021a) From in vitro research to real life studies: an extensive narrative review of the effects of balneotherapy on human immune response. Sport Sci Health. https://doi.org/10.1007/s11332-021-00778-z
Maccarone MC, Magro G, Tognolo L, Masiero S (2021b) Post COVID-19 persistent fatigue: a proposal for rehabilitative interventions in the spa. Int J Biometeorol:1–3. https://doi.org/10.1007/s00484-021-02158-1
Masiero S (2008) Thermal rehabilitation and osteoarticular diseases of the elderly. Aging ClinExp Res 20(3):189–194. https://doi.org/10.1007/BF03324772
Masiero S, Vittadini F, Ferroni C, Bosco A, Serra R, Frigo AC, Frizziero A (2018) The role of thermal balneotherapy in the treatment of obese patient with knee osteoarthritis. Int J Biometeorol 62(2):243–252. https://doi.org/10.1007/s00484-017-1445-7
Masiero S, Maghini I, Mantovani ME, Bakdounes L, Koutsikos K, del Felice A, Sale P (2019) Is the aquatic thermal environment a suitable place for providing rehabilitative treatment for person with Parkinson's disease? A retrospective study. Int J Biometeorol 63(1):13–18. https://doi.org/10.1007/s00484-018-1632-1
Masiero S, Maccarone MC, Agostini F (2020a) Health resort medicine can be a suitable setting to recover disabilities in patients tested negative for COVID-19 discharged from hospital? A challenge for the future Int J Biometeorol 64:1807–1809. https://doi.org/10.1007/s00484-020-01947-4
Masiero S, Maccarone MC, Magro G (2020b) Balneotherapy and human immune function in the era of COVID-19. Int J Biometeorol 64:1433–1434. https://doi.org/10.1007/s00484-020-01914-z
Passali D, De Corso E, Platzgummer S et al (2013) Spa therapy of upper respiratory tract inflammations. Eur Arch Otorhinolaryngol 270(2):565–570. https://doi.org/10.1007/s00405-012-2024-5
Passali D, Gabelli G, Passali GC, Mösges R, Bellussi LM (2017) Radon-enriched hot spring water therapy for upper and lower respiratory tract inflammation. Otolaryngol Pol 71(4):8–13. https://doi.org/10.5604/01.3001.0010.2242
Siddiq M, Rathore FA, Clegg D, Rasker JJ (2020) Pulmonary Rehabilitation in COVID-19 patients: a scoping review of current practice and its application during the pandemic. Turk J Phys Med Rehabil 66(4):480–494. https://doi.org/10.5606/tftrd.2020.6889
Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, Hill K, Holland AE, Lareau SC, Man WD, Pitta F, Sewell L, Raskin J, Bourbeau J, Crouch R, Franssen FM, Casaburi R, Vercoulen JH, Vogiatzis I, Gosselink R, Clini EM, Effing TW, Maltais F, van der Palen J, Troosters T, Janssen DJ, Collins E, Garcia-Aymerich J, Brooks D, Fahy BF, Puhan MA, Hoogendoorn M, Garrod R, Schols AM, Carlin B, Benzo R, Meek P, Morgan M, Rutten-van Mölken M, Ries AL, Make B, Goldstein RS, Dowson CA, Brozek JL, Donner CF, Wouters EF, ATS/ERS Task Force on Pulmonary Rehabilitation (2013) An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J RespirCrit Care Med 188:e13–e64
Vermund SH, Pitzer VE (2020) Asymptomatic transmission and the infection fatality risk for COVID-19: implications for school reopening. Clin Infect Dis 72:1493–1496. https://doi.org/10.1093/cid/ciaa855
Wang TJ, Chau B, Lui M, Lam GT, Lin N, Humbert S (2020) Physical medicine and rehabilitation and pulmonary rehabilitation for COVID-19. Am J Phys Med Rehabil 99(9):769–774. https://doi.org/10.1097/PHM.0000000000001505
World Health Organisation: World Health Organisation, Coronavirus Disease 2019 (COVID19) situation dashboard (cited May 31, 2021) Avaible from: https://covid19.who.int/
You J, Zhang L, Ni-Jia-Ti MY, Zhang J, Hu F, Chen L et al (2020) Anormal pulmonary function and residual CT abnormalities in rehabilitating COVID-19 patients after discharge. J Inf Secur 81:e150–e1e2
Availability of data and materials
Not applicable
Funding
Open access funding provided by Università degli Studi di Padova within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Both authors, Maria Chiara Maccarone and Stefano Masiero, contributed to the conception of the research, acquisition of data, drafting, and revision of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable. This research does not involve the use of any animal or human data or tissue. Articles referred to have all complied with ethical approval.
Consent to participate
Not applicable
Consent for publication
Not applicable”
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maccarone, .C., Masiero, S. Spa therapy interventions for post respiratory rehabilitation in COVID-19 subjects: does the review of recent evidence suggest a role?. Environ Sci Pollut Res 28, 46063–46066 (2021). https://doi.org/10.1007/s11356-021-15443-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-15443-8