Abstract
Study objectives
Use of a mandibular advancement appliance (MAA) is an effective treatment option for mild-to-moderate obstructive sleep apnea (OSA). MAA is well-tolerated but undesirable effects may be observed over time. The present systematic review aimed to assess the effect of MAA use on oral and periodontal health in patients with OSA.
Methods
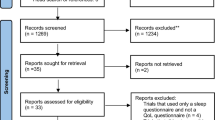
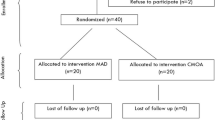
MEDLINE (PubMed), Cochrane, and Scopus were searched for randomized and non-randomized controlled trials (RCTs, NRCTs), cohorts, and case–control studies reporting on side effects of MAA treatment in OSA patients during a follow-up of at least 6 months.
Results
From a total of 169 articles screened, 28 were selected. The most frequently reported MAA-related effects on oral health were: hypersalivation (weighted mean prevalence, 33.3%), occlusal changes (30.2%), muscle pain (22.9%), tooth discomfort or pain (20.2%), and xerostomia (18.3%). No MAA-related periodontal effect was reported. The periodontal status prior to MAA treatment was rarely assessed and described, but 5 studies (17.8%) stated that periodontitis was an exclusion criterion for MAA. Only one retrospective study specifically evaluated periodontal parameters and reported no significant changes in periodontally healthy patients with OSA using MAA for over 7 years.
Conclusion
MAA use is associated with a number of clinical consequences on oral health, but there is no evidence to conclude whether or not MAA affects periodontal health in patients with OSA. This aspect appears to be under-evaluated and should be further investigated in relation to the type of MAA, the duration of treatment, and prior history of periodontitis.


Similar content being viewed by others
Data availability
Data will be made available on reasonable request.
References
Sutherland K, Vanderveken OM, Tsuda H, Marklund M, Gagnadoux F, Kushida CA, Cistulli PA (2014) Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med 10(2):215–227. https://doi.org/10.5664/jcsm.3460
Pattipati M, Gudavalli G, Zin M, Dhulipalla L, Kolack E, Karki M, Devarakonda PK, Yoe L (2022) Continuous positive airway pressure vs mandibular advancement devices in the treatment of obstructive sleep apnea: an updated systematic review and meta-analysis. Cureus 14(1):e21759. https://doi.org/10.7759/cureus.21759
Bratton DJ, Gaisl T, Wons AM, Kohler M (2015) CPAP vs mandibular advancement devices and blood pressure in patients with obstructive sleep apnea: a systematic review and meta-analysis. JAMA 314(21):2280–2293. https://doi.org/10.1001/jama.2015.16303
Li P, Ning XH, Lin H, Zhang N, Gao YF, Ping F (2020) Continuous positive airway pressure versus mandibular advancement device in the treatment of obstructive sleep apnea: a systematic review and metaanalysis. Sleep Med 72:5–11. https://doi.org/10.1016/j.sleep.2020.03.015
Schwartz M, Acosta L, Hung YL, Padilla M, Enciso R (2018) Effects of CPAP and mandibular advancement device treatment in obstructive sleep apnea patients: a systematic review and meta-analysis. Sleep Breath 22(3):555–568. https://doi.org/10.1007/s11325-017-1590-6
Aurora RN, Punjabi NM (2013) Obstructive sleep apnoea and type 2 diabetes mellitus: a bidirectional association. Lancet Respir Med 1(4):329–338. https://doi.org/10.1016/S2213-2600(13)70039-0
Gilat H, Vinker S, Buda I, Soudry E, Shani M, Bachar G (2014) Obstructive sleep apnea and cardiovascular comorbidities: a large epidemiologic study. Medicine (Baltimore) 93(9):e45. https://doi.org/10.1097/MD.0000000000000045
Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, D’Agostino RB, Newman AB, Lebowitz MD, Pickering TG (2000) Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study JAMA 283(14):1829–1836. https://doi.org/10.1001/jama.283.14.1829
Cistulli PA, Sutherland K (2019) Phenotyping obstructive sleep apnoea-bringing precision to oral appliance therapy. J Oral Rehabil 46(12):1185–1191. https://doi.org/10.1111/joor.12857
Randerath W, Verbraecken J, de Raaff CAL, Hedner J, Herkenrath S, Hohenhorst W, Jakob T, Marrone O, Marklund M, McNicholas WT, Morgan RL, Pepin JL, Schiza S, Skoetz N, Smyth D, Steier J, Tonia T, Trzepizur W, van Mechelen PH, Wijkstra P (2021) European Respiratory Society guideline on non-CPAP therapies for obstructive sleep apnoea. Eur Respir Rev 30(162):210200. https://doi.org/10.1183/16000617.0200-2021
Hartfield PJ, Janczy J, Sharma A, Newsome HA, Sparapani RA, Rhee JS, Garcia GJM (2023) Anatomical determinants of upper airway collapsibility in obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med Rev 68. https://doi.org/10.1016/j.smrv.2022.101741
Chen H, Eckert DJ, van der Stelt PF, Guo J, Ge S, Emami E, Huynh NT (2020) Phenotypes of responders to mandibular advancement device therapy in obstructive sleep apnea patients: A systematic review and meta-analysis. Sleep Med Rev 49. https://doi.org/10.1016/j.smrv.2019.101229
Alessandri-Bonetti G, Ippolito DR, Bartolucci ML, D’Anto V, Incerti-Parenti S (2015) Cephalometric predictors of treatment outcome with mandibular advancement devices in adult patients with obstructive sleep apnea: a systematic review. Korean J Orthod 45(6):308–321. https://doi.org/10.4041/kjod.2015.45.6.308
Dieltjens M, Vanderveken O (2019) Oral Appliances in Obstructive Sleep Apnea. Healthcare (Basel) 7. https://doi.org/10.3390/healthcare7040141
Agha B, Johal A (2017) Facial phenotype in obstructive sleep apnea-hypopnea syndrome: a systematic review and meta-analysis. J Sleep Res 26(2):122–131. https://doi.org/10.1111/jsr.12485
Tallamraju H, Newton JT, Fleming PS, Johal A (2021) Factors influencing adherence to oral appliance therapy in adults with obstructive sleep apnea: a systematic review and meta-analysis. J Clin Sleep Med 17(7):1485–1498. https://doi.org/10.5664/jcsm.9184
National Guideline C (2021) NICE Evidence Reviews Collection. Oral devices: obstructive sleep apnoea/hypopnoea syndrome and obesity hypoventilation syndrome in over 16s: evidence review G, National Institute for Health and Care Excellence (NICE) Copyright © NICE 2021., London
Bernhardt O, Giannakopoulos NN, Heise M, Meyer A, Norden D, Schlieper J, Kares H (2023) Mandibular advancement device: prescription in adult dental sleep medicine — guideline of the German Society of Dental Sleep Medicine. Sleep Breath 27(1):389–397. https://doi.org/10.1007/s11325-022-02601-6
Lang NP, Bartold PM (2018) Periodontal health. J Clin Periodontol 45(Suppl 20):S9–S16. https://doi.org/10.1111/jcpe.12936
Chapple ILC, Mealey BL, Van Dyke TE, Bartold PM, Dommisch H, Eickholz P, Yoshie H (2018) Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol 45(Suppl 20):S68–S77. https://doi.org/10.1111/jcpe.12940
Ghazal A, Jonas IE, Rose EC (2008) Dental side effects of mandibular advancement appliances - a 2-year follow-up. J Orofac Orthop 69(6):437–447. https://doi.org/10.1007/s00056-008-0811-9
Hamoda MM, Almeida FR, Pliska BT (2019) Long-term side effects of sleep apnea treatment with oral appliances: nature, magnitude and predictors of long-term changes. Sleep Med 56:184–191. https://doi.org/10.1016/j.sleep.2018.12.012
Knappe SW, Bakke M, Svanholt P, Petersson A, Sonnesen L (2017) Long-term side effects on the temporomandibular joints and oro-facial function in patients with obstructive sleep apnoea treated with a mandibular advancement device. J Oral Rehabil 44(5):354–362. https://doi.org/10.1111/joor.12485
Martins OFM, Chaves Junior CM, Rossi RRP, Cunali PA, Dal-Fabbro C, Bittencourt L (2018) Side effects of mandibular advancement splints for the treatment of snoring and obstructive sleep apnea: a systematic review. Dental Press J Orthod 23(4):45–54. https://doi.org/10.1590/2177-6709.23.4.045-054.oar
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, Group P-P (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4(1):1. https://doi.org/10.1186/2046-4053-4-1
Higgins J, Savović J, Page M, Sterne J (2019) Revised Cochrane risk-of-bias tool for randomized trials (RoB 2)
Higgins J, Sterne J, Savović J, Page M, Hróbjartsson A, Boutron I, Reeves B, Eldridge S (2016) A revised tool for assessing risk of bias in randomized trials. In: Chandler J, McKenzie J, Boutron I, Welch V (eds) Cochrane methods. Cochrane Database of Systematic Reviews Vol. 10 (Suppl 1)
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Walker-Engstrom ML, Ringqvist I, Vestling O, Wilhelmsson B, Tegelberg A (2003) A prospective randomized study comparing two different degrees of mandibular advancement with a dental appliance in treatment of severe obstructive sleep apnea. Sleep Breath 7(3):119–130. https://doi.org/10.1007/s11325-003-0119-3
Doff MH, Hoekema A, Pruim GJ, Huddleston Slater JJ, Stegenga B (2010) Long-term oral-appliance therapy in obstructive sleep apnea: a cephalometric study of craniofacial changes. J Dent 38(12):1010–1018. https://doi.org/10.1016/j.jdent.2010.08.018
Doff MH, Veldhuis SK, Hoekema A, Slater JJ, Wijkstra PJ, de Bont LG, Stegenga B (2012) Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on temporomandibular side effects. Clin Oral Investig 16(3):689–697. https://doi.org/10.1007/s00784-011-0555-6
Doff MH, Finnema KJ, Hoekema A, Wijkstra PJ, de Bont LG, Stegenga B (2013) Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on dental side effects. Clin Oral Investig 17(2):475–482. https://doi.org/10.1007/s00784-012-0737-x
Aarab G, Lobbezoo F, Hamburger HL, Naeije M (2011) Oral appliance therapy versus nasal continuous positive airway pressure in obstructive sleep apnea: a randomized, placebo-controlled trial. Respiration 81(5):411–419. https://doi.org/10.1159/000319595
Aarab G, Nikolopoulou M, Ahlberg J, Heymans MW, Hamburger HL, de Lange J, Lobbezoo F (2017) Oral appliance therapy versus nasal continuous positive airway pressure in obstructive sleep apnea: a randomized, placebo-controlled trial on psychological distress. Clin Oral Investig 21(7):2371–2378. https://doi.org/10.1007/s00784-016-2045-3
Nikolopoulou M, Byraki A, Ahlberg J, Heymans MW, Hamburger HL, De Lange J, Lobbezoo F, Aarab G (2017) Oral appliance therapy versus nasal continuous positive airway pressure in obstructive sleep apnoea syndrome: a randomised, placebo-controlled trial on self-reported symptoms of common sleep disorders and sleep-related problems. J Oral Rehabil 44(6):452–460. https://doi.org/10.1111/joor.12505
Nikolopoulou M, Aarab G, Ahlberg J, Hamburger HL, de Lange J, Lobbezoo F (2020) Oral appliance therapy versus nasal continuous positive airway pressure in obstructive sleep apnea: a randomized, placebo-controlled trial on temporomandibular side-effects. Clin Exp Dent Res 6(4):400–406. https://doi.org/10.1002/cre2.288
Robertson CJ (2001) Dental and skeletal changes associated with long-term mandibular advancement. Sleep 24(5):531–537. https://doi.org/10.1093/sleep/24.5.531
Rose EC, Staats R, Virchow C Jr, Jonas IE (2002) Occlusal and skeletal effects of an oral appliance in the treatment of obstructive sleep apnea. Chest 122(3):871–877. https://doi.org/10.1378/chest.122.3.871
Robertson C, Herbison P, Harkness M (2003) Dental and occlusal changes during mandibular advancement splint therapy in sleep disordered patients. Eur J Orthod 25(4):371–376. https://doi.org/10.1093/ejo/25.4.371
Monteith BD (2004) Altered jaw posture and occlusal disruption patterns following mandibular advancement therapy for sleep apnea: a preliminary study of cephalometric predictors. Int J Prosthodont 17(3):274–280
Fransson AM, Tegelberg A, Johansson A, Wenneberg B (2004) Influence on the masticatory system in treatment of obstructive sleep apnea and snoring with a mandibular protruding device: a 2-year follow-up. Am J Orthod Dentofacial Orthop 126(6):687–693. https://doi.org/10.1016/j.ajodo.2003.10.040
Fransson AMC, Benavente-Lundahl C, Isacsson G (2020) A prospective 10-year cephalometric follow-up study of patients with obstructive sleep apnea and snoring who used a mandibular protruding device. Am J Orthod Dentofacial Orthop 157(1):91–97. https://doi.org/10.1016/j.ajodo.2019.02.018
Almeida FR, Lowe AA, Otsuka R, Fastlicht S, Farbood M, Tsuiki S (2006) Long-term sequellae of oral appliance therapy in obstructive sleep apnea patients: part 2. Study-model analysis. Am J Orthod Dentofacial Orthop 129(2):205–213. https://doi.org/10.1016/j.ajodo.2005.04.034
Hou HM, Sam K, Hagg U, Rabie AB, Bendeus M, Yam LY, Ip MS (2006) Long-term dentofacial changes in Chinese obstructive sleep apnea patients after treatment with a mandibular advancement device. Angle Orthod 76(3):432–440. https://doi.org/10.1043/0003-3219(2006)076[0432:LDCICO]2.0.CO;2
Hammond RJ, Gotsopoulos H, Shen G, Petocz P, Cistulli PA, Darendeliler MA (2007) A follow-up study of dental and skeletal changes associated with mandibular advancement splint use in obstructive sleep apnea. Am J Orthod Dentofacial Orthop 132(6):806–814. https://doi.org/10.1016/j.ajodo.2005.08.047
Marklund M, Franklin KA (2007) Long-term effects of mandibular repositioning appliances on symptoms of sleep apnoea. J Sleep Res 16(4):414–420. https://doi.org/10.1111/j.1365-2869.2007.00615.x
Chen H, Lowe AA, de Almeida FR, Fleetham JA, Wang B (2008) Three-dimensional computer-assisted study model analysis of long-term oral-appliance wear. Part 2. Side effects of oral appliances in obstructive sleep apnea patients. Am J Orthod Dentofacial Orthop 134(3):408–417. https://doi.org/10.1016/j.ajodo.2006.10.031
Martinez-Gomis J, Willaert E, Nogues L, Pascual M, Somoza M, Monasterio C (2010) Five years of sleep apnea treatment with a mandibular advancement device. Side effects and technical complications. Angle Orthod 80(1):30–36. https://doi.org/10.2319/030309-122.1
Perez CV, de Leeuw R, Okeson JP, Carlson CR, Li HF, Bush HM, Falace DA (2013) The incidence and prevalence of temporomandibular disorders and posterior open bite in patients receiving mandibular advancement device therapy for obstructive sleep apnea. Sleep Breath 17(1):323–332. https://doi.org/10.1007/s11325-012-0695-1
Pliska BT, Nam H, Chen H, Lowe AA, Almeida FR (2014) Obstructive sleep apnea and mandibular advancement splints: occlusal effects and progression of changes associated with a decade of treatment. J Clin Sleep Med 10(12):1285–1291. https://doi.org/10.5664/jcsm.4278
Wang X, Gong X, Yu Z, Gao X, Zhao Y (2015) Follow-up study of dental and skeletal changes in patients with obstructive sleep apnea and hypopnea syndrome with long-term treatment with the Silensor appliance. Am J Orthod Dentofacial Orthop 147(5):559–565. https://doi.org/10.1016/j.ajodo.2015.01.013
Minagi HO, Okuno K, Nohara K, Sakai T (2018) Predictors of side effects with long-term oral appliance therapy for obstructive sleep apnea. J Clin Sleep Med 14(1):119–125. https://doi.org/10.5664/jcsm.6896
Heda P, Alalola B, Almeida FR, Kim H, Peres BU, Pliska BT (2021) Long-term periodontal changes associated with oral appliance treatment of obstructive sleep apnea. J Clin Sleep Med 17(10):2067–2074. https://doi.org/10.5664/jcsm.9358
Al-Jewair TS, Al-Jasser R, Almas K (2015) Periodontitis and obstructive sleep apnea’s bidirectional relationship: a systematic review and meta-analysis. Sleep Breath 19(4):1111–1120. https://doi.org/10.1007/s11325-015-1160-8
Keller JJ, Wu CS, Chen YH, Lin HC (2013) Association between obstructive sleep apnoea and chronic periodontitis: a population-based study. J Clin Periodontol 40(2):111–117. https://doi.org/10.1111/jcpe.12036
Sales-Peres SH, Groppo FC, Rojas LV, de C. Sales‐Peres M, Sales-Peres A (2016) Periodontal status in morbidly obese patients with and without obstructive sleep apnea syndrome risk: a cross-sectional study. J Periodontol 87(7):772–782
Stazic P, Roguljic M, Dogas Z, Lusic Kalcina L, Pavlinac Dodig I, Valic M, Bozic D, Pecotic R (2022) Periodontitis severity in obstructive sleep apnea patients. Clin Oral Investig 26(1):407–415. https://doi.org/10.1007/s00784-021-04012-5
Zhang Z, Ge S, Zhai G, Yu S, Cui Z, Si S, Chou X (2022) Incidence and risk of periodontitis in obstructive sleep apnea: a meta-analysis. PLoS One 17(7):e0271738. https://doi.org/10.1371/journal.pone.0271738
Sanders AE, Essick GK, Beck JD, Cai J, Beaver S, Finlayson TL, Zee PC, Loredo JS, Ramos AR, Singer RH, Jimenez MC, Barnhart JM, Redline S (2015) Periodontitis and sleep disordered breathing in the Hispanic Community Health Study/Study of Latinos. Sleep 38(8):1195–1203. https://doi.org/10.5665/sleep.4890
Seo WH, Cho ER, Thomas RJ, An SY, Ryu JJ, Kim H, Shin C (2013) The association between periodontitis and obstructive sleep apnea: a preliminary study. J Periodontal Res 48(4):500–506. https://doi.org/10.1111/jre.12032
Carra M, Eberhard J, Cistulli PA (2020) Periodontal diseases and OSA. In: Lavigne GJ, Cistulli PA, Smith MT (eds) Sleep medicine for dentists. An evidence-based overview. Quintessence Publishing, Batavia
Carra MC, Thomas F, Schmitt A, Pannier B, Danchin N, Bouchard P (2016) Oral health in patients treated by positive airway pressure for obstructive sleep apnea: a population-based case-control study. Sleep Breath 20(1):405–411. https://doi.org/10.1007/s11325-015-1239-2
Bianchi G, de’Angelis N, Gavriilidis P, Sobhani I, de’Angelis GL, Carra MC (2022) Oral microbiota in obstructive sleep apnea patients: a systematic review. Sleep Breath. https://doi.org/10.1007/s11325-022-02718-8
Lembo D, Caroccia F, Lopes C, Moscagiuri F, Sinjari B, D’Attilio M (2021) Obstructive sleep apnea and periodontal disease: a systematic review. Medicina (Kaunas) 57(6):640. https://doi.org/10.3390/medicina57060640
Zhu J, Yuan X, Zhang Y, Wei F, Hou Y, Zhang Y (2022) A meta-analysis on the association between obstructive sleep apnea and periodontitis. Sleep Breath. https://doi.org/10.1007/s11325-022-02668-1
Lavigne GJ, Herrero Babiloni A, Beetz G, Dal Fabbro C, Sutherland K, Huynh N, Cistulli PA (2020) Critical issues in dental and medical management of obstructive sleep apnea. J Dent Res 99(1):26–35. https://doi.org/10.1177/0022034519885644
Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Tonetti MS (2018) Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol 45(Suppl 20):S162–S170. https://doi.org/10.1111/jcpe.12946
Caton JG, Armitage G, Berglundh T, Chapple ILC, Jepsen S, Kornman KS, Tonetti MS (2018) A new classification scheme for periodontal and peri-implant diseases and conditions - Introduction and key changes from the 1999 classification. J Clin Periodontol 45(Suppl 20):S1–S8. https://doi.org/10.1111/jcpe.12935
Wei Y, Wang Z, Lei L, Chen L (2021) Global burden of periodontal disease and its relation with socioeconomic development during 1990–2019. Zhejiang Da Xue Xue Bao Yi Xue Ban 50(5):545–552. https://doi.org/10.3724/zdxbyxb-2021-0321
Herrera D, Sanz M, Kebschull M, Jepsen S, Sculean A, Berglundh T, Papapanou PN, Chapple I, Tonetti MS, Participants EFPW, Methodological C (2022) Treatment of stage IV periodontitis: the EFP S3 level clinical practice guideline. J Clin Periodontol 49(Suppl):244–71. https://doi.org/10.1111/jcpe.13639
Jepsen K, Tietmann C, Kutschera E, Wullenweber P, Jager A, Cardaropoli D, Gaveglio L, Sanz Sanchez I, Martin C, Fimmers R, Jepsen S (2021) The effect of timing of orthodontic therapy on the outcomes of regenerative periodontal surgery in patients with stage IV periodontitis: a multicenter randomized trial. J Clin Periodontol 48(10):1282–1292. https://doi.org/10.1111/jcpe.13528
Sanz M, Herrera D, Kebschull M, Chapple I, Jepsen S, Beglundh T, Sculean A, Tonetti MS, Participants EFPW, Methodological C (2020) Treatment of stage I-III periodontitis-the EFP S3 level clinical practice guideline. J Clin Periodontol 47(Suppl 22):4–60. https://doi.org/10.1111/jcpe.13290
Otsuka R, Almeida FR, Lowe AA (2007) The effects of oral appliance therapy on occlusal function in patients with obstructive sleep apnea: a short-term prospective study. Am J Orthod Dentofacial Orthop 131(2):176–183. https://doi.org/10.1016/j.ajodo.2005.03.028
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
This article does not contain any studies with human participants performed by any of the authors.
Research involving human participants and/or animals
Not applicable
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mansour, N., Saade, Y., Mora, F. et al. Effect of mandibular advancement appliance use on oral and periodontal health in patients with OSA: a systematic review. Sleep Breath 28, 1005–1017 (2024). https://doi.org/10.1007/s11325-023-02971-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02971-5