Abstract
Purpose
To review various smartphone applications (apps) for sleep architecture and screening of obstructive sleep apnea (OSA) and to outline their utility for sleep physicians.
Methods
Mobile application stores (Google Play and Apple iOS App Store) were searched for sleep analysis applications (apps) that are targeted for consumer use. Apps were identified by two independent investigators for apps published through July 2022. App information including parameters obtained for sleep analysis were extracted from each app.
Results
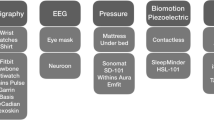
The search identified 50 apps that reported sufficient outcome measures to be considered for assessment. Half of the apps tracked sleep with phone-only technology, while 19 utilized sleep and fitness trackers, three utilized sleep-only wearable devices, and three utilized nearable devices. Seven apps provided data useful for tracking users for signs and symptoms of obstructive sleep apnea.
Conclusion
There are a variety of sleep analysis apps available on the market to consumers currently. Though the sleep analysis of these apps may not be validated, sleep physicians should be aware of these apps to improve understanding and education of their patients.
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AHI:
-
Apnea–hypopnea index
- App:
-
Applications
- CPAP:
-
Continuous positive airway pressure device
- EEG:
-
Electroencephalogram
- EOG:
-
Electrooculogram
- NREM:
-
Non-rapid eye movement sleep
- OSA:
-
Obstructive sleep apnea
- PPG:
-
Photoplethysmography
- PSG:
-
Polysomnogram
- REM:
-
Rapid eye movement sleep
References
Hillman DR, Lack LC (2013) Public health implications of sleep loss: the community burden. Med J Aust 199(8):S7-10. https://doi.org/10.5694/mja13.10620
Franklin KA, Lindberg E (2015) Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. J Thorac Dis 7(8):1311–1322. https://doi.org/10.3978/j.issn.2072-1439.2015.06.11
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006–1014. https://doi.org/10.1093/aje/kws342
EtindeleSosso FA (2022) Measuring sleep health disparities with polysomnography: a systematic review of preliminary findings. Clocks Sleep 4(1):80–87. https://doi.org/10.3390/clockssleep4010009
Ahmadi N, Shapiro GK, Chung SA, Shapiro CM (2009) Clinical diagnosis of sleep apnea based on single night of polysomnography vs. two nights of polysomnography. Sleep Breath 13(3):221–6. https://doi.org/10.1007/s11325-008-0234-2
Grandner MA ea (2019) Chapter 12 – Actigraphic sleep tracking and wearables: historical context, scientific applications and guidelines, limitations, and considerations for commercial sleep devices. In: MA G, ed. Sleep and Health. Academic Press; 147–157:chap 12
Kolla BP, Mansukhani S, Mansukhani MP (2016) Consumer sleep tracking devices: a review of mechanisms, validity and utility. Expert Rev Med Devices 13(5):497–506. https://doi.org/10.1586/17434440.2016.1171708
Baron KG, Duffecy J, Berendsen MA, Cheung Mason I, Lattie EG, Manalo NC (2018) Feeling validated yet? A scoping review of the use of consumer-targeted wearable and mobile technology to measure and improve sleep. Sleep Med Rev 40:151–159. https://doi.org/10.1016/j.smrv.2017.12.002
Bianchi MT (2018) Sleep devices: wearables and nearables, informational and interventional, consumer and clinical. Metabolism 84:99–108. https://doi.org/10.1016/j.metabol.2017.10.008
Sadeh A (2011) The role and validity of actigraphy in sleep medicine: an update. Sleep Med Rev 15(4):259–267. https://doi.org/10.1016/j.smrv.2010.10.001
Ong AA, Gillespie MB (2016) Overview of smartphone applications for sleep analysis. World J Otorhinolaryngol Head Neck Surg 2(1):45–49. https://doi.org/10.1016/j.wjorl.2016.02.001
Lui GY, Loughnane D, Polley C, Jayarathna T, Breen PP (2022) The Apple Watch for monitoring mental health-related physiological symptoms: literature review. JMIR Ment Health 9(9):e37354. https://doi.org/10.2196/37354
Muzet A, Werner S, Fuchs G et al (2016) Assessing sleep architecture and continuity measures through the analysis of heart rate and wrist movement recordings in healthy subjects: comparison with results based on polysomnography. Sleep Med 21:47–56. https://doi.org/10.1016/j.sleep.2016.01.015
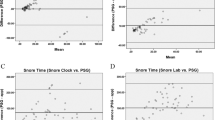
Chinoy ED, Cuellar JA, Huwa KE, et al. (2021) Performance of seven consumer sleep-tracking devices compared with polysomnography. Sleep 44(5). https://doi.org/10.1093/sleep/zsaa291
Nguyen QNT, Le T, Huynh QBT, Setty A, Vo TV, Le TQ (2021) Validation framework for sleep stage scoring in wearable sleep trackers and monitors with polysomnography ground truth. Clocks Sleep 3(2):274–288. https://doi.org/10.3390/clockssleep3020017
Wu X, Yang J, Pan Y, Zhang X, Luo Y (2020) Automatic sleep-stage scoring based on photoplethysmographic signals. Physiol Meas 41(6):065008. https://doi.org/10.1088/1361-6579/ab921d
Lee XK, Chee N, Ong JL et al (2019) Validation of a consumer sleep wearable device with actigraphy and polysomnography in adolescents across sleep opportunity manipulations. J Clin Sleep Med 15(9):1337–1346. https://doi.org/10.5664/jcsm.7932
Moreno-Pino F, Porras-Segovia A, López-Esteban P, Artés A, Baca-García E (2019) Validation of Fitbit Charge 2 and Fitbit Alta HR against polysomnography for assessing sleep in adults with obstructive sleep apnea. J Clin Sleep Med 15(11):1645–1653. https://doi.org/10.5664/jcsm.8032
Schade MM, Bauer CE, Murray BR et al (2019) Sleep validity of a non-contact bedside movement and respiration-sensing device. J Clin Sleep Med 15(7):1051–1061. https://doi.org/10.5664/jcsm.7892
Android SA (2020) How does Sleep as Android compare to the Sleep lab. Updated April 5, 2020. Accessed April 5, 2023, 2023. https://sleep.urbandroid.org/sleep-lab-comparison/
Haghayegh S, Khoshnevis S, Smolensky MH, Diller KR, Castriotta RJ (2019) Accuracy of wristband Fitbit models in assessing sleep: systematic review and meta-analysis. J Med Internet Res. 21(11):e16273. https://doi.org/10.2196/16273
Roberts DM, Schade MM, Mathew GM, Gartenberg D, Buxton OM (2020) Detecting sleep using heart rate and motion data from multisensor consumer-grade wearables, relative to wrist actigraphy and polysomnography. Sleep 43(7). https://doi.org/10.1093/sleep/zsaa045
Altini M, Kinnunen H (2021) The promise of sleep: a multi-sensor approach for accurate sleep stage detection using the Oura ring. Sensors (Basel) 21(13). https://doi.org/10.3390/s21134302
de Zambotti M, Rosas L, Colrain IM, Baker FC (2019) The sleep of the ring: comparison of the ŌURA sleep tracker against polysomnography. Behav Sleep Med Mar-Apr 17(2):124–136. https://doi.org/10.1080/15402002.2017.1300587
Henriksen A, Svartdal F, Grimsgaard S, Hartvigsen G, Hopstock LA (2022) Polar vantage and Oura physical activity and sleep trackers: validation and comparison study. JMIR Form Res 6(5):e27248. https://doi.org/10.2196/27248
Laricchia F US (2022) Wearable devices ownership by age 2021 - Statista. Accessed September 02, 2022. https://www.statista.com/statistics/1310364/wearable-devices-ownership-age-us/
Author information
Authors and Affiliations
Contributions
All authors have reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study did not utilize human or animal subjects and as such, ethical approval is not applicable.
Informed consent
This article does not contain any studies with human participants performed by any of the authors.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hathorn, T., Byun, Y.J., Rosen, R. et al. Clinical utility of smartphone applications for sleep physicians. Sleep Breath 27, 2371–2377 (2023). https://doi.org/10.1007/s11325-023-02851-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02851-y